Abstract
Introduction and hypothesis
The prevalence of urinary incontinence (UI) varies among women in different cultures. Muslim women with UI have complex issues related to the need for cleaning (ablution) before prayer. The aim was to assess the prevalence of UI, factors associated with it, its effect on quality of life, and help-seeking behavior among Muslim women.
Methods
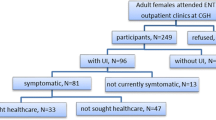
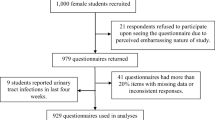
This was a cross-sectional study. Self-administered questionnaires completed by women 18–75 years of age who visited the primary care clinic between 21 June 2015 and 9 October 2015 and additional data collected from their medical records.
Results
A total of 492 women (mean age 31.8 ± 9.5 years) participated in the study. Of these, 43% suffered from UI and 19% from severe to very severe UI. The mean score for interference in daily life (0–10) was 6.3 ± 3.7. Sixty percent of women with UI had stress incontinence, 23% urge incontinence, and 9% mixed incontinence. Only 10% had consulted previously with their physician regarding UI. Increased BMI (OR = 1.048, 95% CI 1.009–1.089) and polygamy (OR = 1.943, 95% CI 1.007–3.749) were associated with severe to very severe UI. Age, parity, and more severe degrees of UI were associated with help-seeking behavior (OR = 1.065 95% CI 1.008–1.125, OR = 0.763 95% CI 0.624–0.934, OR = 4.073 95% CI 1.410–11.765 respectively).
Conclusions
Urinary incontinence is very common among Muslim women in primary care in southern Israel and significantly impairs their quality of life. Only a small percentage consults with their physician.
Similar content being viewed by others
References
Goroll HA, Mulley AG. Primary care medicine: office evaluation and management of the adult patient. Philadelphia: Wolters Kluwer Health; 2014.
Charalambous S, Trantafyldis A. Impact of urinary incontinence on quality of life. Pelviperineology. 2009;28:51–3.
Rogers RG. Clinical practice. Urinary stress incontinence in women. N Engl J Med. 2008;358:1029–36.
Abrams P, Cardozo LJ, Khouri S, et al. (2013) Incontinence. 5th edition ed. Bristol: ICUD-EAU.
Markland AD, Richter HE, Fwu CW, et al. Prevalence and trends of urinary incontinence in adults in the United States, 2001 to 2008. J Urol. 2011;186:589–93.
Cooper J, Annappa M, Quigley A, et al. Prevalence of female urinary incontinence and its impact on quality of life in a cluster population in the United Kingdom (UK): a community survey. Prim Health Care Res Dev. 2015;16:377–82.
Bedretdinova D, Fritel X, Panjo H, et al. Prevalence of female urinary incontinence in the general population according to different definitions and study designs. Eur Urol. 2016;69:256–64.
Garcia-Perez H, Harlow SD, Sampselle CM, et al. Measuring urinary incontinence in a population of women in northern Mexico: prevalence and severity. Int Urogynecol J. 2013;24:847–54.
Rebassa M, Taltavull JM, Gutierrez C, et al. Urinary incontinence in Mallorcan women: prevalence and quality of life. Actas Urol Esp. 2013;37:354–61.
Gozukara F, Koruk I, Kara B. Urinary incontinence among women registered with a family health center in the southeastern Anatolia region and the factors affecting its prevalence. Turk J Med Sci. 2015;45:931–9.
Altaweel W, Alharbi M. Urinary incontinence: prevalence, risk factors, and impact on health related quality of life in Saudi women. Neurourol Urodyn. 2012;31:642–5.
Jokhio AH, Rizvi RM, Rizvi J, et al. Urinary incontinence in women in rural Pakistan: prevalence, severity, associated factors and impact on life. BJOG. 2013;120:180–66.
Sange C, Thomas L, Lyons C, et al. Urinary incontinence in Muslim women. Nurs Times. 2008;104:49–52.
Wilkinson K. Pakistan women's perceptions and experiences of incontinence. Nurs Stand. 2008;16:33–9.
Van den Muijsenbergh ME, Largo-Janssen TA. Urinary incontinence in Moroccan and Turkish women: a qualitative study on impact and preferences for treatment. Br J Gen Pract. 2006;56:945–9.
Ben-Rabi D, Amiel S, Nijim F, et al. Bedouin children in the Negev: characteristics, needs, and patterns of service use. Jerusalem: Myers-JDC-Brookdale Institute. Research Report Publication; 2009.
Hashim H, Avery K, Mourad MS, et al. The Arabic ICIQ-UI SF: an alternative language version of the English ICIQ-UI SF. Neurourol Urodyn. 2006;25:277–82.
Al-Shaikh G, Al-Badr A, Al Maarik A, et al. Reliability of Arabic ICIQ-UI short form in Saudi Arabia. Urol Ann. 2013;5:34–8.
Klovning A, Avery K, Sandvik H, et al. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28:411–5.
Bar-Yakov M, Cohen A. New statistical activities and publications in Israel: population and demographics. Jerusalem: Israel Central Bureau of Statistics; 2010.
Treister-Goltzman Y, Peleg R. Literature review of type 2 diabetes mellitus among minority Muslim populations in Israel. World J Diabetes. 2015;6:192–9.
Zwickel J, Barak N. Health and welfare of Bedouin women in the Negev [Hebrew]. Beer-Sheva: Center for Regional Development, Center for the Study and Promotion of Women's Health, Center for Bedouin Studies and Development, Ben-Gurion University of the Negev; 2002.
Treister-Goltzman Y, Peleg R. Health and morbidity among Bedouin women in southern Israel: a descriptive literature review of the past two decades. J Community Health. 2014;39:819–25.
Rios AA, Cardoso JR, Rodrigues MA, et al. The help-seeking by women with urinary incontinence in Brazil. Int Urogynecol J. 2011;22:879–84.
El-Azab AS, Shaaban OM. Measuring the barriers against seeking consultation for urinary incontinence among Middle Eastern women. BMC Womens Health. 2010;10:3.
Perera J, Kirthinanda DS, Wijeratne S, et al. Descriptive cross sectional study on prevalence, perceptions, predisposing factors and health seeking behaviour of women with stress urinary incontinence. BMC Womens Health. 2014;14:78.
Cetinel B, Demirkesen O, Tarcan T, et al. Hidden female urinary incontinence in urology and obstetrics and gynecology outpatient clinics in Turkey: what are the determinants of bothersome urinary incontinence and help-seeking behavior? Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:659–64.
Ng SF, Lok MK, Pang SM, et al. Stress urinary incontinence in younger women in primary care: prevalence and opportunistic intervention. J Women's Health (Larchmt). 2014;23:65–8.
Amaral MO, Coutinho EC, Nelas PA, et al. Risk factors associated with urinary incontinence in Portugal and the quality of life of affected women. Int J Gynaecol Obstet. 2015;131:82–6.
Kilic M. Incidence and risk factors of urinary incontinence in women visiting family health centers. Springerplus. 2016;5:1331.
Saadia Z. Effect of age, educational status, parity and BMI on development of urinary incontinence—a cross sectional study in Saudi population. Mater Sociomed. 2015;27:251–4.
Khullar V, Sexton CC, Thompson CL, et al. The relationship between BMI and urinary incontinence subgroups: results from EpiLUTS. Neurourol Urodyn. 2014;33:392–29.
Kwon JG, Park KS, Park JH, et al. [Guidelines for the treatment of irritable bowel syndrome]. Korean J Gastroenterol. Taehan Sohwagi Hakhoe chi. 2011;57:82–99.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclaimer
This research was funded by a grant from the Israel Association of Family Physicians: 15,000 NIS.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Treister-Goltzman, Y., Peleg, R. Urinary incontinence among Muslim women in Israel: risk factors and help-seeking behavior. Int Urogynecol J 29, 539–546 (2018). https://doi.org/10.1007/s00192-017-3438-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3438-9