Abstract
Introduction and hypothesis
We aimed to evaluate the association between obstructive defecatory symptoms in women with levator ani deficiency (LAD), worsened minimum levator hiatus measurements, widened anorectal angle (ARA), and increased levator-plate descent angle (LPDA).
Methods
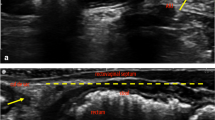
Using a cross-sectional study design, patients who had undergone 3D endovaginal ultrasound (3D EVUS) imaging of the pelvic floor were sampled and categorized into two groups: those with and those without obstructive defecatory symptoms (ODS) based on their Colorectal and Anal Distress Index (CRADI-8) questionnaire. The levator ani (LA) muscle was scored based on severity of defect. ARA and LPDA were measured and dichotomized (ARA ± 170°; LPDA ± 9°.
Results
One hundred patients were analyzed: 52 asymptomatic and 48 with ODS. The mean (standard deviation ) age was 59 years (SD ±14.97). There was no difference in the distribution of LAD severity between groups (p = 0.1438) or mean minimal levator hiatus (MLH) (p = 0.3326). ARA and LPDA were significantly different in those with ODS compared with their asymptomatic counterparts (p < 0.0001 and 0.0004, respectively) (Table 1). On multivariable logistic regression, ARA and LPDA were included in the final model. Patients with an ARA >170° had seven times the odds of ODS than those with ARA ≤170° [odds ratio (OR) = 7.01, 95 % confidence interval (CI) 2.30–21.35; p = 0.0006). Patients with an LPDA <9° had 3 times the odds of ODS than those with an LPDA ≥9° (OR = 3.30, 95 % CI 1.22, 8.96, p = 0.0190).
Conclusions
This study demonstrates that increased levator plate descent and widened ARA as measured on 3D endovaginal ultrasound imaging are associated with ODS.


Similar content being viewed by others
References
Blanchette G (2003) The prevalence of pelvic floor disorders and their relationship to gender, age and mode of delivery. Bjog 110(1):88, author reply 88–89
Kepenekci I, Keskinkilic B, Akinsu F, Cakir P, Elhan AH, Erkek AB, Kuzu MA (2011) Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery, and parity. Dis Colon Rectum 54(1):85–94
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2000) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG: Int J Obstet Gynaecol 107(12):1460–1470
Lam TJ, Kuik DJ, Felt-Bersma RJ (2012) Anorectal function evaluation and predictive factors for faecal incontinence in 600 patients. Color Dis 14(2):214–223
Lammers K, Futterer JJ, Inthout J, Prokop M, Vierhout ME, Kluivers KB (2013) Correlating signs and symptoms with pubovisceral muscle avulsions on magnetic resonance imaging. Am J Obstet Gynecol 208(2):5
Piloni V, Tosi P, Vernelli M (2013) MR-defecography in obstructed defecation syndrome (ODS): technique, diagnostic criteria and grading. Tech Coloproctol 17(5):501–510
Viscardi A, Ratto C, Parello A (2012) Dynamic transperineal ultrasound in the workup of men with obstructed defecation: a pilot study. Dis Colon Rectum 55(9):976–982
Beer-Gabel M, Teshler M, Barzilai N, Lurie Y, Malnick S, Bass D, Zbar A (2002) Dynamic transperineal ultrasound in the diagnosis of pelvic floor disorders: pilot study. Dis Colon Rectum 45(2):239–245, discussion 245–238
Martellucci J, Naldini G (2011) Clinical relevance of transperineal ultrasound compared with evacuation proctography for the evaluation of patients with obstructed defaecation. Color Dis 13(10):1167–1172
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–113. doi:10.1016/j.ajog.2004.12.025
Santoro GA, Wieczorek AP, Shobeiri SA, Mueller ER, Pilat J, Stankiewicz A, Battistella G (2011) Interobserver and interdisciplinary reproducibility of 3D endovaginal ultrasound assessment of pelvic floor anatomy. Int Urogynecol J Pelvic Floor Dysfunct 22:53–59
Shobeiri SA, Leclaire E, Nihira MA, Quiroz LH, O’Donoghue D (2009) Appearance of the levator ani muscle subdivisions in endovaginal three-dimensional ultrasonography. Obstet Gynecol 114:66–72
Rostaminia G, White D, Hegde A, Quiroz LH, Davila GW, Shobeiri SA (2013) Levator Ani Deficiency and Pelvic Organ Prolapse severity. Obstet Gynecol 121:1017–1024. doi:10.1097/AOG.0b013e31828ce97d
Shobeiri SA, Chesson RR, Gasser RF (2008) The internal innervation and morphology of the human female levator ani muscle. Am J Obstet Gynecol 199(6):686.e681–686.e686. doi:10.1016/j.ajog.2008.07.057
Shobeiri SA, Rostaminia G, White D, Quiroz LH (2013) The determinants of minimal levator hiatus and their relationship to the puborectalis muscle and the levator plate. BJOG: Int J Obstet Gynaecol 120(2):205–211
Athanasiadis S, Weyand G, Kuprian A, Kohler A (1995) What is the role of the pubococcygeal and puborectal muscles in patients with obstructive defecation disorders? An electromyography study. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 66(10):974–981
Saks EK, Harvie HS, Asfaw TS, Arya LA (2010) Clinical significance of obstructive defecatory symptoms in women with pelvic organ prolapse. Int J Gynaecol Obstet: Off Organ Int Fed Gynaecol Obstet 111(3):237–240
Dietz HP (2009) Rectocele or stool quality: what matters more for symptoms of obstructed defecation? Tech Coloproctology 13(4):265–268
Ellis CN, Essani R (2012) Treatment of obstructed defecation. Clin Colon Rectal Surg 25(1):24–33
Hicks CW, Weinstein M, Wakamatsu M, Pulliam S, Savitt L, Bordeianou L (2013) Are rectoceles the cause or the result of obstructed defaecation syndrome? A prospective anorectal physiology study. Colorectal Dis 15(8):993–999
Brown HW, Wexner SD, Segall MM, Brezoczky KL, Lukacz ES (2012) Quality of life impact in women with accidental bowel leakage. Int J Clin Pract 66(11):1109–1116
Pucciani F (2013) Faecal soiling: pathophysiology of postdefaecatory incontinence. Colorectal Dis 15(8):987–992
Financial disclaimers/conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Leary, D., Rostaminia, G., Quiroz, L.H. et al. Sonographic predictors of obstructive defecatory dysfunction. Int Urogynecol J 26, 415–420 (2015). https://doi.org/10.1007/s00192-014-2515-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2515-6