Abstract
Introduction and hypothesis
Development of a model that can predict in which group of women pre-operative urodynamics can be safely omitted.
Methods
Three hundred and eighty-one uncomplicated women who underwent pre-operative urodynamics were evaluated. A multivariate logistic regression model was developed based on medical history and physical examination predicting a high probability group of women with detrusor overactivity or a low (<20 cm H2O) mean urethral closure pressure and, therefore, are likely to benefit from urodynamics.
Results
Women are likely to benefit from pre-operative urodynamics if they (1) are 53 years of age or older or (2) have a history of prior incontinence surgery and are at least 29 years of age or (3) have nocturia complaints and are at least 36 years of age.
Conclusion
If urogynaecologists omitted pre-operative urodynamics in women in the low probability group, in our population, pre-operative urodynamics would be reduced by 29%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 13% of the female population is affected by stress urinary incontinence (SUI) [1]. If conservative therapy fails, surgical treatment is considered the therapy of choice. The lifetime risk that women will have surgical treatment for SUI is about 4% [2]. In current urogynaecological practice, urodynamics are routinely performed before considering surgical treatment for SUI. This strategy is recommended in both gynaecological and urological guidelines [3, 4].
Recent studies have shown that the sensitivity of urodynamics to diagnose SUI is far from perfect, especially in women with mixed urinary incontinence (MUI) [5, 6]. Therefore, routine use of pre-operative urodynamics in all women with an indication for surgical treatment of SUI is debatable [7–9].
On the other hand, detrusor overactivity (DO) is a risk factor for failure of mid-urethral sling (MUS) procedures or at least carries a worse prognosis [9–11]. A recent study even suggested that better results might be obtained with transobturator tape (TOT) compared to retropubic tension-free vaginal tape (TVT) in women with DO [12]. Another recently published prospective study showed that women with a low (<20 cm H2O) maximal urethral closure pressure (MUCP) benefit from a retropubic TVT [13]. Therefore, urodynamics can be used to select the proper MUS procedure.
Nevertheless, the indication for urodynamics needs to be more precisely determined considering the negative side effects (costs, a delay in surgery, risk of infection and patient discomfort). The aim of this study was to develop a model that can identify women for whom pre-operative urodynamics can be safely omitted.
Material and methods
This study is based on data from prospective studies investigating the outcome of the TVT and afterwards the TOTs (Monarc and TVT-O) as surgical treatment for female SUI. Both studies were approved by the Medical Ethical Committee of the St. Elisabeth Hospital Tilburg.
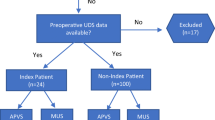
Since 1998, data were collected consecutively on women undergoing either TVT, Monarc or TVT-O in the St. Elisabeth Hospital Tilburg. For this study, we only report on women who did not undergo concomitant surgical procedures (like prolapse surgery). Excluded were women with missing values of DO or MUCP at urodynamics and women with neurological disorders or pre-existent voiding dysfunction.
Before surgery, each woman underwent a standardised urogynaecological workup. The definitions used are according to the recommendations of the International Continence Society [14]. A history of SUI was defined as the statement of the women of involuntary leakage during physical activity, coughing or sneezing. A history of urge urinary incontinence (UUI) was defined as the statement of involuntary leakage preceded by a strong sense of urgency. A history of MUI was defined as a combination of SUI and UUI. Nocturia was defined as a micturition frequency >1 during sleep. Pelvic organ prolapse was scored according to the Baden–Walker classification [15].
Multichannel urodynamic investigation was performed in all women according to the recommendations of the International Continence Society and followed by cystoscopy [16, 17]. During the initial visit and after the cystoscopy, a cough-stress test was performed in supine position with standard volume.
Two groups were discriminated during outcome assessment. Theoretically, the group of women who did not reveal DO or a low MUCP at urodynamics was expected not to benefit from pre-operative urodynamics. This group is referred to as ‘urodynamically normal’. The second group consisted of women who revealed DO and/or low MUCP at pre-operative urodynamics and therefore are likely to benefit from urodynamics [9–13]. This group is referred to as ‘urodynamically abnormal’.
The aim of the analysis was to develop a model that can predict a high probability group of urodynamically abnormal women using parameters from the medical history and findings at physical examination. First, the association between each diagnostic variable and abnormal urodynamics was quantified using logistic regression analyses. Subsequently, predictors that were univariately associated with the outcome (odds ratio with a p < 0.15) were included in a multivariate logistic regression model to evaluate their independent contribution to the prediction of abnormal urodynamics. Predictors in the multivariate analysis with p ≥ 0.10 were excluded from the final model.
The Hosmer and Lemeshow test was applied to assess if the model adequately fitted the data [18]. The resulting model can be considered as a ‘combined diagnostic test’, including several diagnostic findings, with the estimated probability of presence of abnormal urodynamics as its test result.
The diagnostic value of the model was quantified using the area under the receiver operating characteristic (ROC) curve. The ROC curve shows the model’s sensitivity against 1 minus its specificity for each cutoff value for the predicted probability of abnormal urodynamics above which the urodynamics of women are actually considered as abnormal. An area under the ROC curve of 0.5 implies that the discriminatory capacity of the model does not exceed chance levels (rendering it meaningless), whereas an area under the ROC curve of 1 implies a perfect discriminatory capacity [19].
With an area under the curve in between 0.5 and 1, a cutoff predicted probability should be chosen that optimises the balance between the number of women with normal urodynamics for whom unnecessary pre-operative urodynamics can be prevented and the number of women with abnormal urodynamics who will erroneously be excluded from urodynamics.
In order to define pre-operative workup guidelines, we subsequently assessed which combinations of parameter values of the predictors in the final model would suffice to increase a woman’s predicted probability of abnormal urodynamics above the chosen cutoff value.
Results
A total of 437 women were operated in the St. Elisabeth Hospital Tilburg, The Netherlands and included in one of both studies from January 1998 until December 2006. This study population contained 381 women because 56 women (13%) with missing values of DO or MUCP at urodynamics were excluded.
Baseline characteristics are shown in Table 1. All women had symptoms of predominant SUI. Two hundred and ninety-four women (77%) had symptoms of pure SUI and 87 women (23%) had symptoms of MUI. All women with MUI received anticholinergic treatment, which did not alleviate their symptoms. Twenty-five (7%) women showed DO, 39 (10%) women showed low MUCP and two women showed both.
Table 2 shows uni- and multivariate analyses and regression coefficients (ß) of the association of findings from medical history and physical examination with abnormal urodynamics. The final model included age, previous incontinence surgery and nocturia.
The predicted probabilities of abnormal urodynamics derived from the model were used to generate a ROC curve of the need for pre-operative urodynamics (Fig. 1). The corresponding area under the ROC curve was 0.65 (95% CI, 0.58–0.72). The cutoff predicted probability of abnormal urodynamics was set at 0.12. Hence, all women with a predicted probability of abnormal urodynamics above 0.12 would be subjected to urodynamic procedures.
To formulate clinical decision rules (prediction model), combinations of values for age (continuous), previous incontinence surgery (yes/no) and nocturia (yes/no) were determined in order for the prediction model, exp (0.031 × age + 0.743 × previous incontinence surgery + 0.525 × nocturia − 3.606), to exceed this cutoff predicted probability of 0.12. Hence, women are likely to benefit from pre-operative urodynamics if they (1) are 53 years of age or older or (2) have a history of prior incontinence surgery and are at least 29 years of age or (3) have nocturia complaints and are at least 36 years of age. This model fitted the data adequately (Hosmer and Lemeshow test p > 0.4).
This model, in our population, has a sensitivity of 90% (56/62) and a negative predictive value of 94% (95/101), as shown in Table 3. Exclusion of the less predictive variable (nocturia) from this model significantly decreased the negative predictive value (the number of women with abnormal urodynamics who would erroneously be excluded from urodynamics, doubled from 6 to 12).
If urogynaecologists would decide not to demand for pre-operative urodynamics in women with a low probability of abnormal urodynamics, in our population, pre-operative urodynamics would be reduced by 29% (101/351).
Discussion
The aim of this study was to investigate whether the findings of DO or a low MUCP in women with predominant SUI can be predicted by information obtained from medical history and physical examination. In this group of women, urodynamic results could have influenced pre-operative counselling and the choice of the surgical procedure [9–13]. Therefore, this group of women might benefit from pre-operative urodynamics.
Simple decision rules (53 years of age or older, a history of prior incontinence surgery and at least 29 years of age, complaints of nocturia and at least 36 years of age) containing only variables from medical history had a high sensitivity (90%) and negative predictive value (94%). Therefore, these rules accurately identify women in whom pre-operative urodynamics can be safely omitted. Nevertheless, before implementation of this model in clinical practice, the actual performance of these decision rules should be proven using these rules in a new group of women with SUI and an indication for surgical treatment [20].
An important question is “What are the consequences of missing DO or a low MUCP?” For missing DO, a consequence is too optimistic counselling for cure of SUI [9]. It is also known that persistence or worsening of the UUI after surgery negatively affects the outcome of MUS procedures [21, 22]. Furthermore, DO might play a role in predicting post-operative overactive bladder symptoms [23]. There are indications that a TOT procedure might give better results in women with DO, but these findings need to be confirmed in prospective randomised trials [12].
Missing a low MUCP, on the other hand, might have more evident consequences. Schierlitz et al. [13] found that women with a low MUCP performed significantly better after a TVT procedure compared with TOT. Six months after surgery, 21% had urodynamic stress incontinence in the TVT group compared with 45% in the TOT group. Furthermore, nine women in the TOT group underwent repeat sling surgery compared with none in the TVT group. These findings were confirmed in other studies [24–26]. In conclusion, missing DO does not influence surgical treatment, but a low MUCP should influence choice of suspension.
Because surgeries have irreversible outcome, high sensitivity of the decision rules was regarded most important and resulted in a conservative cutoff for predicted probability of abnormal urodynamics of 0.12. This indicates that urodynamics are performed if the model predicted a chance of abnormal urodynamics above 12%. The chosen cutoff generated the optimal balance between the number of women with normal urodynamics for whom unnecessary pre-operative urodynamics can be prevented and the number of women with abnormal urodynamics who will erroneously be excluded from urodynamics.
The area under the curve of 0.65 is not very high. However, the discriminative power of the investigated diagnostic test (urodynamics), an invasive investigation with considerable side effects, is not undisputed itself in uncomplicated women [7–9]. Therefore, the AUC of 0.65 seems acceptable for this research question.
Women who revealed DO or low MUCP at pre-operative urodynamics were combined in one group in this study. Separate models predicting DO or a low MUCP were substantially worse compared with this final model. Little evidence exists of other urodynamic parameters influencing treatment modus or outcome in uncomplicated women with an indication for surgical treatment of SUI [21]. Therefore, in this study, we made the premise that only women with DO or a low MUCP might benefit from urodynamics.
A possible drawback of this model is women with voiding dysfunction. Voiding dysfunction can be present without symptoms and without a pre-existing history. This group would not be properly identified by the presented model. However, as patients with known pre-existing voiding dysfunction and post-voiding bladder retention of more than 150 ml were already excluded from this study, this group is likely to be very small.
The strength of this study is the large number of women treated in the same clinic. Therefore, the same workup was used to evaluate symptoms and score findings at physical examination. We did not collect all the parameters we studied from each woman, as can been seen in Table 1. The most pronounced missing data are micturition frequency (8%) and nocturia (8%). We did not exclude these women because the other parameters might still have prognostic influence, and valuable information would be lost if they were excluded.
The variables decided upon are drawn from the patients' history and demographics. This contrasts with many of the earlier papers, which have looked at clinical features, and other simple tests, which are non-invasive and may be helpful. Therefore, this paper aims to introduce a new concept for approaching the difficult subject of pre-operative urodynamics, their validity and their role and stimulate the development of other models for discrimination.
Conclusion
Women without neurological disease or pre-existing voiding dysfunction and with an intention for surgical treatment of SUI (without concomitant prolapse surgery) are likely to benefit from pre-operative urodynamics if they (1) are 53 years of age or older or (2) have a history of prior incontinence surgery and are at least 29 years of age or (3) have nocturia complaints and are at least 36 years of age. The presented decision rules achieved a very high negative predictive value (94%) while still eliminating the need to perform urodynamics in 29% of the women. Before implementation in clinical practice, these rules should be validated.
References
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S, Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trøndelag (2000) A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trøndelag. J Clin Epidemiol 53(11):1150–1157
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Groenendijk AG, Vervest HAM, van der Vaart CH, van Geelen JM (2005) Richtlijn Urine Incontinentie. Nederlandse Vereniging voor Obstetrie en Gynaecologie, Utrecht
Venema PL, van Geelen JM, Kil PJM, van Capelle JW, Tjon Pan Gi NP, de Ridder D, Wiersema T (2003) Richtlijn Stressincontinentie bij de vrouw. Nederlandse vereniging voor Urologie, Utrecht
Gorton E, Stanton S (2000) Ambulatory urodynamics: do they help clinical management? BJOG 107:316–319
Cundiff GW, Harris RL, Coates KW, Bump RC (1997) Clinical predictors of urinary incontinence in women. Am J Obstet Gynecol 177:262–267
Ghoniem G, Stanford E, Kenton K, Achtari C, Goldberg R, Mascarenhas T, Parekh M et al (2008) Evaluation and outcome measures in the treatment of female urinary stress incontinence: International Urogynecological Association (IUGA) guidelines for research and clinical practice. Int Urogynecol J Pelvic Floor Dysfunct 19:5–33
Farrell SA, Epp A, Flood C, Lajoie F, MacMillan B, Mainprize T, Robert M (2003) The evaluation of stress incontinence prior to primary surgery. J Obstet Gynaecol Can 25:313–324
Houwert RM, Venema PL, Aquarius AE, Bruinse HW, Kil PJM, Vervest HAM (2009) Predictive value of urodynamics on outcome of midurethral sling surgery for female stress urinary incontinence. Am J Obstet Gynecol 200(6):649.e1–649.e12
Glazener CMA, Lapitan MC (2002) Urodynamic investigations for management of urinary incontinence in children and adults (review). Cochrane Database Syst Rev (3):CD003195
Kuo H-C (2007) Effect of detrusor function on the therapeutic outcome of a suburethral sling procedure using a polypropylene sling for stress urinary incontinence in women. Scand J Urol Nephrol 41:138–143
Houwert RM, Venema PL, Aquarius AE, Bruinse HW, Roovers JPWR, Vervest HAM (2009) Risk factors for failure of retropubic and transobturator midurethral slings. Am J Obstet Gynecol 201(2):202.e1–202.e8
Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, Lim YN, Hiscock R (2008) Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol 112(6):1253–1261
Abrahams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U (2002) The standardization of terminology of the lower urinary tract function. Report from the Standardization Subcommittee of the International Continence Society. Neurourol Urodynam 21:167–178
Baden WF, Walker TA (1972) Genesis of the vaginal profile: a correlated classification of vaginal relaxation. Clin Obstet Gynecol 15:1048–1054
Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A et al (2002) Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21:261-74.22
Swift SE, Yoon EA (1999) Test-retest reliability of the cough stress test in the evaluation of urinary incontinence. Obstet Gynecol 94:99–102
Hosmer DW, Lemeshow S (1989) Applied logistic regression. Wiley, New York
Hanley JA, McNeil BJ (1982) The meaning and use of the area under the receiver operating characteristic (ROC) curve. Radiology 143:29–36
Roovers JP, van der Bom JG, van der Vaart CH, Heintz AP (2005) Prediction of findings at defecography in patients with genital prolapse. BJOG 112(11):1547–1553
Fletcher SG, Lemack GE (2008) Clarifying the role of urodynamics in the preoperative evaluation of stress urinary incontinence. ScientificWorldJournal 25(8):1259–1268
Gamble TL, Botros SM, Beaumont JL, Goldberg RP, Miller JJ, Adeyanju O, Sand PK (2008) Predictors of persistent detrusor overactivity after transvaginal sling procedures. Am J Obstet Gynecol 199(6):696.e1–696.e7
Panayi DC, Duckett J, Digesu GA, Camarata M, Basu M, Khullar V (2009) Pre-operative opening detrusor pressure is predictive of detrusor overactivity following TVT in patients with pre-operative mixed urinary incontinence. Neurourol Urodyn 28(1):82–85
Miller JJ, Botros SM, Akl MN, Aschkenazi SO, Beaumont JL, Goldberg RP, Sand PK (2006) Is transobturator tape as effective as tension-free vaginal tape in patients with borderline maximum urethral closure pressure? Am J Obstet Gynecol 195(6):1799–1804
Jung HJ, Yim GW, Jeon MJ, Kim SK, Bai SW (2009) Preoperative maximum urethral closure pressure and valsalva leak point pressure as predictive parameters for midurethral sling. J Reprod Med 54(7):436–440
Gungorduk K, Celebi I, Ark C, Celikkol O, Yildirim G (2009) Which type of mid-urethral sling procedure should be chosen for treatment of stress urinary incontinance with intrinsic sphincter deficiency? Tension-free vaginal tape or transobturator tape. Acta Obstet Gynecol Scand 88(8):920–926
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Houwert, R.M., Roovers, J.P.W.R., Venema, P.L. et al. When to perform urodynamics before mid-urethral sling surgery for female stress urinary incontinence?. Int Urogynecol J 21, 303–309 (2010). https://doi.org/10.1007/s00192-009-1035-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-1035-2