Abstract
Introduction and hypothesis
The objective of this study was to assess the effect of the tension-free vaginal mesh (Prolift™) procedure on the non-treated and initially unaffected vaginal compartments.
Methods
This prospective observational cohort study involved 150 patients who underwent a Prolift™ procedure. Pelvic organ prolapse (POP) quantification and evaluation of prolapse symptoms with validated questionnaires was performed pre-operatively and 6 and 12 months postoperatively. Primary outcome was the rate of POP stage ≥II in the non-treated vaginal compartments.
Results
Twenty-three percent of all patients developed a de novo POP stage ≥II in the untreated compartment. This occurred in 46% and 25% of patients after an isolated anterior and isolated posterior Prolift™, respectively.
Conclusion
Tension-free vaginal mesh treatment of one vaginal compartment seems to provoke the development of vaginal prolapse in initially unaffected vaginal compartments, particularly after an isolated anterior Prolift™ procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) has a high prevalence in parous women [1]. A wide variety of abdominal and vaginal surgical techniques is available for the treatment of POP, indicating lack of consensus on the optimal treatment. The choice of the type of operation depends on multiple factors such as site and severity of prolapse, additional symptoms, and the surgeon’s preference and capability. In order to prevent recurrence, the use of synthetic meshes and biological grafts in pelvic reconstructive surgery has increased considerably in recent years. The results of prolapse repair with synthetic mesh are promising, with success rates ranging from 71-100% [2]. Mesh exposure, infection, dyspareunia, constipation, urgency, urge urinary incontinence, and urinary retention are reported as adverse effects, as well as bladder and rectal injury and bleeding during surgery.
Since 2005, we performed an ongoing prospective observational cohort study to evaluate the anatomical and functional efficacy as well as morbidity of POP repair with a tension-free Vaginal Mesh Kit (Prolift™ Ethicon, Somerville, NJ, USA). During the systematic follow-up of these patients, the clinical impression rose that mesh treatment of one vaginal compartment provoked the development of vaginal prolapse in other initially unaffected compartments. In a previous study, Raalte et al. reported prolapse in the non-mesh compartment after a Prolift™ procedure in 15.5% of cases [3]. In contrast, only 5.3% of patients who underwent conventional prolapse surgery without mesh needed repeat prolapse surgery within 5 years in the compartment that previously appeared well-supported [4].
The aim of this article, therefore, is to evaluate the anatomical effect of Prolift™ treatment and its impact on prolapse symptoms on the non-treated and initially unaffected vaginal compartments.
Material and methods
In two Dutch centers (Radboud University Nijmegen Medical Centre and Reinier de Graaf Group Delft) specializing in pelvic organ dysfunction and surgery, prolapse repair with the Prolift™ system was performed since September 2005. After obtained informed consent, consecutive patients with a recurrent POP stage ≥II and those with a primary POP stage ≥III were enrolled in this prospective observational cohort study. Surgery was performed by four gynecologists who were trained for the Prolift™ procedure as described in the paper by Fatton et al. prior to enrolment of patients in this study [5]. As recommended by these authors, a midline incision was made which included full thickness of the fibromuscular wall of the vagina. The vagina was closed without resection of any vaginal tissue with a continuous running Vicryl 2.0 suture. No simultaneous hysterectomy or T-incisions were made in order to reduce the chance of mesh exposure and erosions [5].
POP was quantified pre-operatively and during follow-up at 6 and 12 months postoperatively according to the pelvic organ prolapse quantification (POP-Q) system, as recommended by the International Continence Society [6]. Subjective symptoms were obtained pre-operatively and during follow-up visits at 6 and 12 months postoperatively with the standard urogynecological questionnaire of the Dutch Pelvic Floor Society (a disease-specific quality of life questionnaire which among others contains the Urogenital Distress Inventory (UDI). The questionnaire as a whole has been validated for the Dutch language [7]. Since the aim of this study was to specifically evaluate the anatomic effect of Prolift™ treatment on the non-treated and initially unaffected vaginal compartments, we only used the domain score on genital prolapse of the UDI. We choose to include only this domain since vaginal bulging symptoms are the only symptoms that are consistently associated with vaginal prolapse [8].
Primary outcome of this study was the rate of POP stage ≥II in the non-treated and initially unaffected compartments. Secondary outcomes were UDI scores on the domain of genital prolapse, anatomical success in the mesh-treated compartments, defined as POP stage≤I, as well as morbidity.
Data on patient and surgical characteristics are presented as numbers with corresponding percentages or medians with range. Comparison between proportions was performed using the Pearson’s chi-square test. Mean domain scores and standard deviations were calculated on the UDI domain genital prolapse. Differences in means between baseline and 12-month follow-up were tested with the paired sample t test and differences in means between different groups were tested with the independent sample t test. Data were analyzed with the Statistical Package for the Social Sciences, version 16.0. A p value of <0.05 was considered significant.
Results
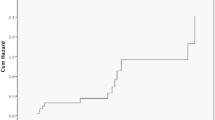
Since the start of our study, 297 patients underwent the Prolift™ procedure and were registered in our database. On January 1, 2009, 196 patients had completed a follow-up of at least 12 months. Patients with a total Prolift™ procedure (46 patients) for post-hysterectomy vaginal vault prolapse, in whom, by definition, all three compartments are restored, were excluded from this study, leaving 150 patients for analysis. At baseline, POPQ data of 147 patients were complete and these patients were eligible for anatomic analysis. Two patients could not visit the hospital for the 12-month follow-up, leaving 145 patients for follow-up analysis. At follow-up, 127 patients (88%) had completed the validated questionnaire.
Patient and surgical characteristics are presented in Table 1. Median age was 64 years (range 32–89). In those patients who underwent a primary repair, median age was 71 years (range 55–89). Ninety-five patients (63%) underwent prior POP surgery, 28 (19%) of those underwent more than one prior prolapse repair. Thirty-five patients (23%) underwent an anterior Prolift™ repair, 80 (54%) a posterior Prolift™ repair, and 35 (23%) a combined anterior and posterior Prolift ™ repair. Three (2%) bladder perforations occurred, all during dissection for an anterior Prolift™ procedure. In two of these patients, the anterior mesh was not placed, but the procedure was converted into a conventional anterior colporrhaphy. One superficial serosa lesion of the rectum occurred, without a perforation. The mesh procedure was continued, since the rectum wall was intact. One patient (1%) had significant hemorrhage (>500 ml) and five patients (3%) developed a postoperative hematoma. Ten patients (7%) had temporary postoperative urinary retention, which resolved spontaneously in all cases within 11 days. In 15 patients (10%), a mesh exposure was detected, six cases at the 6-month follow-up visit and nine at the 12-month follow-up visit. Most of these patients were asymptomatic. Only one patient complained of pain and one other of de novo dyspareunia, but none of them had vaginal discharge or signs of infection. The size of these mesh exposures varied from 2 to 20 mm. All mesh exposures were easily excised and covered with vaginal mucosa in a minor day-care procedure after initial treatment with local estrogens.
POP stages per compartment are shown in Table 2, divided into three categories: those who underwent a solitary anterior Prolift™, a solitary posterior Prolift™, or a combined anterior and posterior Prolift™ procedure. In Table 2, the patients who underwent concomitant, non-mesh surgery are included. Patients who underwent repeat surgery before 12 months follow-up were considered failures.
In Table 3, the effect on the non-operated compartment is shown in patients without concomitant surgery. UDI scores on the domain of genital prolapse are shown in Table 4.
Results after anterior Prolift™
Anatomical success at 1 year in the anterior compartment after anterior Prolift™ repair was 89% (Table 2). Sixteen patients (46%) had a post-operative POP stage II or III of the posterior compartment, of whom three patients had already undergone repeat surgery with a posterior Prolift™ before the 12 months follow-up visit, resulting in a 54% "success" rate. In Table 3, deterioration and improvement of the posterior vaginal wall (Bp) is shown. Twenty-six patients underwent an anterior Prolift™ without concomitant posterior colporrhaphy or sacrospinous fixation. In three patients (12%), point Bp improved with 1 cm. However, in 16 patients (62%), the posterior wall deteriorated (1-4 cm) and in 12 patients (46%), a de novo POP stage ≥II of the posterior compartment was diagnosed at the 12-month follow-up visit.
Five patients (14%) had a post-operative POP stage II or III of the apical compartment resulting in 86% "success" rate (Table 2). In Table 3, it is demonstrated that in five patients (19%) the apical compartment deteriorated, and in three patients (12%) a de novo POP stage ≥II of the apical compartment was detected. These three patients also developed a de novo prolapse in the posterior compartment. Pre-operatively, there was one patient with an apical compartment POP stage III. Due to scar tissue, it was not possible to perform any other surgery then an isolated anterior Prolift™. At 12 months, the apical compartment of this patient was classified as POP stage II. In two patients, a pre-operative POP stage II of the apical compartment resolved without concomitant intervention.
In conclusion, of the 26 patients who underwent an anterior Prolift™ without concomitant surgery, 12 (46%) developed a de novo POP stage ≥II in the non-mesh, non-treated compartment.
Genital prolapse symptoms were evaluated with UDI domain genital prolapse (Table 4). In all patients that underwent an anterior Prolift™, this score improved significantly. However, patients that developed de novo prolapse had a significantly higher bother score at 12 months as compared to patients without de novo prolapse.
Results after posterior Prolift™
Anatomical success in the posterior compartment in patients who underwent an isolated posterior Prolift™ was 90% at 12 months (Table 2). Thirty-one patients (40%) had a post-operative POP stage II or III in the anterior compartment, of whom one patient was treated with an anterior Prolift™ before the 12-months follow-up visit resulting in a 60% "success" rate.
In Table 3, deterioration and improvement of the anterior vaginal wall (Ba) is shown after a posterior Prolift™. Sixty-five patients underwent no concomitant surgery. Deterioration occurred in 35% of them. In 16 patients (25%), a de novo POP stage II or III of the anterior compartment was diagnosed at 12 months.
Five patients (8%) had a POP stage ≥II of the apical compartment at 12 months. In only two patients (3%), this was a de novo apical prolapse. These two patients were also diagnosed with a de novo anterior compartment prolapse.
In conclusion, of the 65 patients with a posterior Prolift™ without concomitant surgery, 16 (25%) developed a de novo POP stage ≥II in the non-mesh, non-treated compartment.
In all, patients that underwent a posterior Prolift™, the UDI score on the domain genital prolapse improved significantly (Table 4). Patients that developed de novo prolapse showed a higher bother score at 12 months as compared to patients without de novo prolapse. The difference, however, was not statistically significant (p = 0.06).
De novo POP after an isolated posterior Prolift™ was diagnosed less often compared to de novo POP after an isolated anterior Prolift™ (25% vs. 46%) (p = 0.044).
Results after a combined anterior and posterior Prolift™
Anatomical success at 12 months in patients with a combined anterior and posterior Prolift™ procedure was 79% for the anterior compartment, 91% for the posterior compartment, and 76% for the apical compartment (Table 2). In Table 3, deterioration and improvement of the apical compartment is shown. In only two patients (6%), a deterioration of the apical compartment was detected, though these patients were still classified as having POP stage I, which, by definition, is not regarded as a failure. Despite an improvement in centimeters compared to baseline, however, eight patients (24%) were still diagnosed with POP stage ≥II of the apical compartment, of which two had additional surgery within 1 year; one laparoscopic cervicosacropexy, and one vaginal hysterectomy with a high Mc Call procedure. In all these eight patients, it was the uterus that had descended, not a vaginal vault.
In conclusion, none of the 35 patients with a combined anterior and posterior Prolift™ developed a de novo prolapse. However, in eight patients (24%), the improvement of the apical compartment prolapse was insufficient.
In all patients that underwent an anterior + posterior Prolift™, the UDI score on the domain genital prolapse improved significantly (Table 4). Patients who were still diagnosed with POP ≥II showed a higher bother score as compared to patients with a POP <II. The difference, however, was not statistically significant (p = 0.06).
In summary, 28 patients (23%) who underwent a Prolift™ procedure (anterior, posterior or combined) were diagnosed with de novo POP stage ≥II in the untreated compartment, and they all had higher bother scores on the UDI domain genital prolapse compared to patients without de novo prolapse. Six patients (4%) had to undergo repeat surgery in the previously non-mesh-treated compartment within the first year of follow-up.
Discussion
The symptomatic de novo POP rate in the non-mesh-treated compartment appeared to be alarmingly high, particularly after an isolated anterior Prolift™. Our de novo POP rate in the non-treated compartment (23%) appeared higher than previously reported by Raalte et al. (15.5%) [3]. One explanation for this difference could be that our study population consisted of a higher number of patients with prior prolapse surgery compared to the population described by Raalte et al. (63% vs. 45%) [3]. The study of Clark et al. on conventional vaginal prolapse surgery demonstrated a repeat surgery rate in the untreated compartment in only 5.3% of patients after 5 years, whereas in our study, this rate was already 4% within the first year [4].
De novo POP in the non-mesh-treated compartment was diagnosed less common after a posterior Prolift™ than after an anterior Prolift™ (25% vs. 46%). Previous studies demonstrated that restoration of DeLancey’s level I support diminishes the rate of anterior and posterior wall prolapse [9, 10]. The position of the arms of the posterior Prolift™ through the sacrospinous ligaments ensures level I support, which potentially results in less de novo POP after a posterior Prolift™ compared to an anterior Prolift™. A recent study, using three-dimensional models generated from magnetic resonance pelvic imaging in women with normal pelvic support, demonstrated that an anterior mesh mainly offers level II support and not enough level I support, since the upper part of the vagina lies well above and posterior to the distal suspension points of the anterior mesh [11]. Since the posterior Prolift™ procedure does provide adequate level I support and the anterior Prolift™ mainly provides level II support, this could explain why we detected an almost twofold higher de novo POP rate after an isolated anterior compared to an isolated posterior Prolift™.
We found no de novo POP in the apical compartment after a combined anterior and posterior Prolift™. However, if the uterus was left in situ, the improvement of the apical compartment was still insufficient (POP stage II or III) in eight cases (24%). Our previously published results, after a total Prolift™ procedure with one continuous mesh for post-hysterectomy vaginal vault prolapse, were significantly better (failure rate 9%) [12]. In order to prevent possible descent of the uterus, the French Tension-free Vaginal Mesh group advised us, during the study, to remove a little part of the mesh at the level where this is fixated to the uterus to ensure a more adequate and, thus, higher suspension of the uterus.
In the mesh-treated compartments, the success rates of 89% (95% CI 78–99) after an anterior mesh and 90% (95% CI 83–97) after a posterior mesh were comparable with other reports on Prolift™ with 1 year follow-up [3, 13]. In the present study, the number of complications was comparable as well with previous reports [3, 5, 13]. Although Raalte et al. reported no patients with mesh exposure, our incidence of mesh exposure (10%) was comparable with an exposure rate of 11% described by Elmer [3, 13]. Despite the fact that mesh exposures rarely caused severe complaints and could be easily excised and covered with vaginal mucosa, it remains an important concern for the future, since the follow-up in this study of 1 year is still relatively short, and the exposure rate might still rise.
The high success rates in the mesh-treated compartments and the high rates of (de novo) symptomatic prolapse in the unaffected/untreated compartments could indicate that we have to change our surgical strategies. Urogynecologists have to realize that placing a mesh in one compartment can provoke or deteriorate a prolapse in any other compartment. It seems logical to be "more liberal" in using mesh, also, in none or minor affected compartments. Whether such a strategy will improve results without an increase in morbidity, such as mesh exposure, mesh retraction and dyspareunia remains to be seen. Providing adequate level I support without the use of more mesh is another surgical strategy, for example adding a sacrospinous hysteropexy or a sacrospinous fixation as a preventive measure of de novo POP to an anterior Prolift™ procedure. Other effective surgical alternatives are the modified Manchester procedure or vaginal hysterectomy with high Mc Call procedure to restore or prevent apical compartment prolapse and, thus, ensuring adequate level I support [14].
In our opinion, the strengths of this study are the high number of patients with adequate follow-up of 12 months, the prospective data collection, and the use of validated instruments of measurement, such as POP-Q and urogynecological questionnaires. A relative drawback is the lack of a control group. A control group with conventional non-mesh surgery might answer the question whether prolapse in the previously unaffected compartments is more often provoked by mesh surgery than by conventional surgery.
Conclusion
Our data suggest that mesh treatment of only one vaginal compartment does provoke the development of POP in other initially unaffected compartments. The development of de novo POP stage ≥II in previously unaffected compartments is almost twice as high after an isolated anterior Prolift™ than after an isolated posterior Prolift™. In case of a POP stage ≥II of the anterior compartment and a stage I of the posterior and/or apical compartment, we suggest to add level I support by a conventional sacrospinous hysteropexy. If there is no uterus in situ, we would suggest considering a total Prolift™ procedure since the results of this treatment are highly effective as reported earlier by us [12]. We feel that patients should be counseled about this strategy and about the pros and cons of additional mesh surgery. They should also be made aware of the potential risk on secondary surgery if no additional treatment is performed initially.
Abbreviations
- POP:
-
pelvic organ prolapse
- POP-Q:
-
pelvic organ prolapse quantification system
- ICS:
-
International Continence Society
- UDI:
-
Urogenital Distress Inventory
References
Beck RP, McCormick S, Nordstrom L (1991) A 25-year experience with 519 anterior colporrhaphy procedures. Obstet Gynecol 78.6:1011–1018
Huebner M, Hsu Y, Fenner DE (2006) The use of graft materials in vaginal pelvic floor surgery. Int J Gynaecol Obstet 92.3:279–288
Raalte HM, Lucente VR, Molden SM, Haff R, Murphy M (2008) One-year anatomic and quality-of-life outcomes after the prolift procedure for treatment of posthysterectomy prolapse. Am J Obstet Gynecol 199:e691–e696
Clark AL, Gregory T, Smith VJ, Edwards R (2003) Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189:1261–1267
Fatton B, Amblard J, Debodinance P, Cosson M, Jacqutin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)—a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct 18.7:743–752
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175.1:10–17
van der Vaart CH, de Leeuw JR, Roovers JP, Heintz AP (2003) Measuring health-related quality of life in women with urogenital dysfunction: the urogenital distress inventory and incontinence impact questionnaire revisited. Neurourol Urodyn 22.2:97–104
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369:1027–1038
Summers A, Winkel LA, Hussain HK, DeLancey JO (2006) The relationship between anterior and apical compartment support. Am J Obstet Gynecol 194:1438–1443
Lowder JL, Park AJ, Ellison R, Ghetti C, Moalli P, Zyczynski H, Weber AM (2008) The role of apical vaginal support in the appearance of anterior and posterior vaginal prolapse. Obstet Gynecol 111:152–157
Larson KA, Hsu Y, DeLancey JOL (2009) The relationship between superior attachment points for anterior wall mesh operations and the upper vagina using a 3-dimensional magnetic resonance model in women with normal support. Am J Obstet Gynecol 200(5):554.e1–554.e6
Milani AL, Withagen MIJ, Vierhout ME (2009) Trocar-guided total tension free vaginal mesh repair of post hysterectomy vaginal vault prolapse. Int Urogynecol J Pelvic Floor Dysfunct. doi:10.1007/s00192-009-0924-8
Elmér E, Altman D, Ellström Engh M, Axelsen S, Väyrynen T, Falconer C (2009) Trocar-guided transvaginal mesh repair of pelvic organ prolapse. Obstet Gynecol 113.1:117–126
de Boer TA, Milani AL, Kluivers KB, Withagen MIJ, Vierhout ME (2009) The effectiveness of surgical correction of uterine prolapse: cervical amputation with uterosacral ligament plication (Modified Manchester) versus vaginal hysterectomy with high uterosacral ligament placation. Int Urogynecol J Pelvic Floor Dysfunct. doi:10.1007/s00192-009-0945-3
Conflicts of interest
A. M. occasionally performs sponsored educational activities for Gynecare Benelux. M. W. and M. V. received an educational grant and are occasionally involved in educational activities for Gynecare Benelux. This study, however, was entirely instigated by the responsible researchers and funded by university-administered research funds. Gynecare was not involved in the study set-up, study design, data collection, or whatsoever.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Withagen, M.I.J., Vierhout, M.E. & Milani, A.L. Does trocar-guided tension-free vaginal mesh (Prolift™) repair provoke prolapse of the unaffected compartments?. Int Urogynecol J 21, 271–278 (2010). https://doi.org/10.1007/s00192-009-1028-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-1028-1