Abstract
Introduction and hypothesis
Prospective studies up to 1 year after repair of obstetric anal sphincter injuries (OASIS) report anal incontinence in 33% of women and up to 92% have a sonographic sphincter defect. The aim of this study is to determine the outcome of repair by doctors who have undergone structured training using a standardized protocol.
Methods
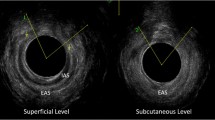
Doctors repaired OASIS after attending a training workshop. The external anal sphincter was repaired by the end-to-end technique when partially divided and the overlap method when completely divided. Endoanal ultrasound was performed prior to suturing and 7 weeks later. A validated bowel symptom questionnaire was completed prior to delivery, at 7 weeks postpartum, and at 1 year postpartum.
Results
Fifty-nine women sustained OASIS. At 7 weeks, six (10%) had a defect on ultrasound. There was no significant deterioration in symptoms of fecal urgency, incontinence, or quality of life at 1 year after delivery.
Conclusions
The 1-year outcome after repair of OASIS appears to be good when repaired by doctors after structured training.


Similar content being viewed by others
References
Snooks SJ, Setchell M, Swash M, Henry MM (1984) Injury to innervations of pelvic floor sphincter musculature in childbirth. Lancet 8(2):546–550
Snooks SJ, Henry MM, Swash M (1985) Faecal incontinence due to external anal sphincter division in childbirth is associated with damage to the innervation of the pelvic floor musculature: a double pathology. Br J Obstet Gynaecol 92(8):824–828
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI (1993) Anal sphincter disruption during vaginal delivery. N Engl J Med 329:1905–1911
Sultan AH, Thakar R (2007) Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner D (eds) Perineal and anal sphincter trauma. Springer, London, pp 33–51
Fitzpatrick M, Cassidy M, O'Connell PR, O'Herlihy C (2002) Experience with an obstetric perineal clinic. Eur J Obstet Gynecol Reprod Biol 100:199–203
Royal College of Obstetricians and Gynaecologists (2007) Third- and fourth-degree perineal tears—management. RCOG guideline no. 29. RCOG Press, London
Thakar R, Sultan AH (2003) Management of obstetric anal sphincter injury. Obstet Gynaecol 5(2):72–78
Andrews V, Thakar R, Sultan AH (2003) Management of third and fourth degree tears. Rev Gynaecol Pract 3:188–195
Andrews V, Sultan AH, Thakar R, Jones PW (2006) Occult anal sphincter injuries—myth or reality. Br J Obstet Gynaecol 113(2):195–200
Sultan AH (1999) Obstetric perineal injury and anal incontinence. Clin Risk 5:193–196
Thakar R, Sultan AH (2004) Anal endosonography and its role in assessing the incontinent patient. Baillieres Best Pract Res Clin Obstet Gynaecol 28(1):157–173
Thakar R, Sultan AH, Fernando R, Monga A, Stanton SL (2001) Can workshops on obstetric anal sphincter rupture change practice? Int Urogynecol J Pelvic Floor Dysfunct 12(3):S5
Bugg GJ, Kiff ES, Hosker G (2001) A new condition-specific health-related quality of life questionnaire for the assessment of women with anal incontinence. Br J Obstet Gynaecol 108:1057–1067
Sander P, Bjarnesen J, Mouritsen L, Fuglsang-Frederiksen A (1999) Anal incontinence after obstetric third-/fourth-degree laceration. One-year follow-up after pelvic floor exercises. Int Urogynecol J Pelvic Floor Dysfunct 10:177–181
Goffeng AR, Andersch B, Andersson M, Berndtsson I, Hulten L, Oresland T (1998) Objective methods cannot predict anal incontinence after primary repair of extensive anal tears. Acta Obstet Gynecol Scand 77:439–443
Sorensen M, Tetzschner T, Rasmussen OO, Bjarnesen J, Christiansen J (1993) Sphincter rupture in childbirth. Br J Surg 80:392–394
Crawford LA, Quint EH, Pearl ML, DeLancey JOL (1993) Incontinence following rupture of the anal sphincter during delivery. Obstet Gynecol 82(4):527–531
Mackenzie N, Parry L, Tasker M, Gowland MR, Michie HR, Hobbiss JH (2003) Anal function following third degree tears. Colorectal Dis 6:92–96
Go PMNYH, Dunselman GAJ (1988) Anatomic and functional results of surgical repair after total perineal rupture at delivery. Surg Gynecol Obstet 166:121–124
Uustal Fornell EK, Berg G, Hallbook O, Matthiesen LS, Sjodahl R (1996) Clinical consequences of anal sphincter rupture during childbirth. J Am Coll Surg 183:553–558
Kammerer-Doak DN, Wesol AB, Rogers RG, Cominguez CE, Dorin MH (1999) A prospective cohort study of women after primary repair of obstetric anal sphincter laceration. Am J Obstet Gynecol 181(6):1317–1322
Haadem K, Ohrlander S, Lingham G (1988) Long-term ailments due to anal sphincter rupture caused by delivery—a hidden problem. Eur J Obstet Gynecol Reprod Biol 27:27–32
Williams A, Adams EJ, Tincello DG, Alfirevic Z, Walkinshaw SA, Richmond DH (2006) How to repair an anal sphincter injury after vaginal delivery: results of a randomized controlled trial. Br J Obstet Gynaecol 113:201–207
Fernando RJ, Sultan AH, Kettle C, Radley S, Jones P, O'Brien PMS (2006) Repair techniques for obstetric anal sphincter injuries. A randomized controlled trial. Obstet Gynecol 107(6):1261–1268
Mahony R, Behan M, O'Herlihy C, O'Connell PR (2004) Randomized, clinical trial of bowel confinement vs laxative use after primary repair of a third-degree obstetric anal sphincter tear. Dis Colon Rectum 47:12–17
Eogan M, Daly L, Behan M, O'Connell PR, O'Herlihy C (2007) Randomised clinical trial of a laxative alone versus a laxative and a bulking agent after primary repair of obstetric anal sphincter injury. Br J Obstet Gynaecol 114(6):736–740
Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY (2008) Antibiotic prophylaxis for prevention of postpartum perineal wound complications: a randomized controlled trial. Obstet Gynecol 111(6):1268–1273
Fernando RJ, Sultan AH, Radley S, Jones PW, Johanson RB (2002) Management of obstetric anal sphincter injury: a systematic review and national practice survey. BMC Health Serv Res 2:9
Sultan AH, Monga AK, Kumar D, Stanton SL (1999) Primary repair of obstetric anal sphincter rupture using the overlap technique. Br J Obstet Gynaecol 106:318–323
Fitzpatrick M, Behan M, O'Connell R, O'Herlihy C (2000) A randomized clinical trial comparing primary overlap with approximation repair of third-degree obstetric tears. Am J Obstet Gynecol 183:1220–1224
Walsh CJ, Mooney CJ, Upton GJ, Motson RW (1996) Incidence of third-degree perineal tears in labour and outcome after primary repair. Br J Surg 83:218–221
Nielsen MB, Hauge C, Rasmussen OO, Pedersen JF, Christiansen (1992) Anal endosonographic findings in the follow-up of primarily sutured sphincteric ruptures. Br J Surg 79:104–106
Sultan AH, Kamm MA, Hudson CN, Bartram CI (1994) Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ 308:887–891
Zetterstrom J, Lopez A, Anzen B, Norman M, Holmstrom B, Mellgren A (1999) Anal sphincter tears at vaginal delivery: risk factors and clinical outcome of primary repair. Obstet Gynecol 94(1):21–28
Belmonte-Montes C, Hagerman G, Vega-Yepez PA, Hernandez-de-Anda E, Fonseca-Morales V (2001) Anal sphincter injury after vaginal delivery in primiparous females. Dis Colon Rectum 44(9):1244–1248
Acknowledgements
We would like to thank the Mayday Childbirth Charity Fund for funding this study.
Disclosure of interest
AS and RT are the directors of the hands-on workshops in the management of third-degree and fourth-degree tears at Mayday University Hospital, and proceeds from these courses are utilized by the Mayday Childbirth Charitable Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andrews, V., Thakar, R. & Sultan, A.H. Outcome of obstetric anal sphincter injuries (OASIS)—role of structured management. Int Urogynecol J 20, 973–978 (2009). https://doi.org/10.1007/s00192-009-0883-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0883-0


