Abstract
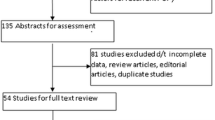
This study evaluated the influence of age and smoking on the occurrence of vaginal erosions after transvaginal mesh repair of pelvic organ prolapses. We recruited all patients that underwent mesh correction of prolapses and excluded those with stress urinary incontinence, ongoing clinical infections, with a complete antibiotic course in the last 6 months, and with systemic diseases affecting tissue oxygenation. We enrolled 325 patients. Postoperative erosions were present in 6%. Age conferred a 1.6-fold increase in the risk to develop erosions while smoking a threefold increase. Patients with deep erosions had the highest values of pack years, and 6.85 pack years conferred a risk similar to advanced age. Age and smoking are important factors also after pelvic organ prolapse surgery. Our data could be used to stratify patients according to their estimated risk and to dedicate them to specific cares for prevention.

Similar content being viewed by others
References
Huebner M, Hsu Y, Fenner DE (2006) The use of graft materials in vaginal pelvic floor surgery. Int J Gynaecol Obstet 92(3):279–88
Deval B, Haab F (2006) Management of the complications of the synthetic slings. Curr Opin Urol 16(4):240–243
Cervigni M, Natale F (2001) The use of synthetics in the treatment of pelvic organ prolapse. Curr Opin Urol 11(4):429–435
Belot F, Collinet P, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2005) Risk factors for prosthesis exposure in treatment of genital prolapse via the vaginal approach. Gynecol Obstet Fertil 33(12):970–974
DeNouy PL (1916) Cicatrization of wounds. J Exp Med 24:461–470
Gilchrest BA (1983) In vitro assessment of keratinocyte aging. J Invest Dermatol 81:184s–189s
Swift ME, Burns AL, Gray KL, DiPietro LA (2001) Age-related alterations in the inflammatory response to dermal injury. J Invest Dermatol 117(5):1027–1035
Ashcroft GS, Horan MA, Ferguson MW (1997) Aging is associated with reduced deposition of specific extracellular matrix components, an upregulation of angiogenesis, and an altered inflammatory response in a murine incisional wound healing model. J Invest Dermatol 108:430–437
Ashcroft GS, Herrick SE, Tarnuzzer RW, Horan MA, Schultz GS, Ferguson MW (1997) Human ageing impairs injury-induced in vivo expression of tissue inhibitor of matrix metalloproteinases (TIMP) -1 and -2 proteins and mRNA. J Pathol 183:169–176
Ashcroft GS, Horan MA, Herrick SE, Tarnuzzer RW, Schultz GS, Ferguson MW (1997) Age-related differences in the temporal and spatial regulation of matrix metalloproteinases (MMP) in normal skin and acute cutaneous wounds of healthy humans. Cell Tissue Res 290:581–591
Reed MJ, Corsa A, Pendergrass W, Penn P, Sage EH, Abrass IB (1998) Neovascularization in aged mice: delayed angiogenesis is coincident with decreased levels of transforming growth factor beta1 and type I collagen. Am J Pathol 152:113–123
Arthur WT, Vernon RB, Sage EH, Reed MJ (1998) Growth factors reverse the impaired sprouting of microvessels from aged mice. Microvasc Res 55:260–270
Mosely LH, Finseth F (1977) Cigarette smoking: impairment of digital blood flow and wound healing in the hand. Hand 9(2):97–101
Mosely LH, Finseth F, Goody M (1978) Nicotine and its effect on wound healing. Plast Reconstr Surg 61(4):570–575
Rees TD, Liverett DM, Guy CL (1984) The effect of cigarette smoking on skin-flap survival in the face lift patient. Plast Reconstr Surg 73(6):911–915
Krueger JK, Rohrich RJ (2001) Clearing the smoke: the scientific rationale for tobacco abstention with plastic surgery. Plast Reconstr Surg 108(4):1063–73
Chan LK, Withey S, Butler PE (2006) Smoking and wound healing problems in reduction mammaplasty: is the introduction of urine nicotine testing justified? Ann Plast Surg 56(2):111–115
Manassa EH, Hertl CH, Olbrisch RR (2003) Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plast Reconstr Surg 111(6):2082–2087
Rogliani M, Labardi L, Silvi E, Maggiulli F, Grimaldi M, Cervelli V (2006) Smokers: risks and complications in abdominal dermolipectomy. Aesthetic Plast Surg 30(4):422–424
Pittet B, Montandon D, Pittet D (2005) Infection in breast implants. Lancet Infect Dis 5(2):94–106
WHO MONICA Project (1992) WHO MONICA Manual: Smoking questionnaire. Available at: URL:http://www.ktl.fi/publications/monica/manual/part3/iii-1.htm
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift trade mark technique)—a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct 18(7):743–752
Belot F, Collinet P, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2005) Prosthetic reinforcement by the vaginal approach after surgical repair of pelvic prolapse. J Gynecol Obstet Biol Reprod 34(8):763–767
Debodinance P, Berrocal J, Clave H, Cosson M, Garbin O, Jacquetin B et al (2004) Changing attitudes on the surgical treatment of urogenital prolapse: birth of the tension-free vaginal mesh. J Gynecol Obstet Biol Reprod 33(7):577–588
Deffieux X, Huel C, de Tayrac R, Bottero J, Porcher R, Gervaise A et al (2006) Vaginal mesh extrusion after transvaginal repair of cystocele using a prosthetic mesh: treatment and functional outcomes. J Gynecol Obstet Biol Reprod 35(7):678–684
Moher D, Schulz KF, Altman DG (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 357:1191–1194
Theadom A, Cropley M (2006) Effects of preoperative smoking cessation on the incidence and risk of intraoperative and postoperative complications in adult smokers: a systematic review. Tob Control 15(5):352–358
Rees TD, Liverett DM, Guy CL (1984) The effect of cigarette smoking on skin-flap survival in the face lift patient. Plast Reconstr Surg 73(6):911–915
Krueger JK, Rohrich RJ (2001) Clearing the smoke: the scientific rationale for tobacco abstention with plastic surgery. Plast Reconstr Surg 108(4):1063–1073
Chan LK, Withey S, Butler PE (2006) Smoking and wound healing problems in reduction mammaplasty: is the introduction of urine nicotine testing justified? Ann Plast Surg 56(2):111–115
Kryger ZB, Fine NA, Mustoe TA (2004) The outcome of abdominoplasty performed under conscious sedation: six-year experience in 153 consecutive cases. Plast Reconstr Surg 113(6):1807–1817
Spiegelman JI, Levine RH (2006) Abdominoplasty: a comparison of outpatient and inpatient procedures shows that it is a safe and effective procedure for outpatients in an office-based surgery clinic. Plast Reconstr Surg 118(2):517–522
Kaufman T, Eichenlaub EH, Levin M, Hurwitz DJ, Klain M (1984) Tobacco smoking: Impairment of experimental flap survival. Ann Plast Surg 13(6):468–472
Lawrence WT, Murphy RC, Robson MC et al (1984) The detrimental effect of cigarette smoking on flap survival: an experimental study in the rat. Br J Plast Surg 37(2):216–219
Van Adrichem LN, Hoegen R, Hovius SE, Kort WJ, van Strik R, Vuzevski VD et al (1996) The effect of cigarette smoking on the survival of free vascularized and pedicled epigastric flaps in the rat. Plast Reconstr Surg 97(1):86–96
Chang LD, Buncke G, Slezak S, Buncke HJ (1996) Cigarette smoking, plastic surgery, and microsurgery. J Reconstr Microsurg 12(7):467–474
Black CE, Huang N, Neligan PC, Levine RH, Lipa JE, Lintlop S et al (2001) Effect of nicotine on vasoconstrictor and vasodilator responses in human skin vasculature. Am J Physiol Regul Integr Comp Physiol 281(4):R1097–104
Astrup P, Kjeldsen K (1974) Carbon monoxide, smoking, and atherosclerosis. Med Clin North Am 58(2):323–350
Birnstingl MA, Brinson K, Chakrabarti BK (1971) The effect of short-term exposure to carbon monoxide on platelet stickiness. Br J Surg 58(11):837–839
Dintenfass L (1975) Elevation of blood viscosity, aggregation of red cells, haematocrit values and fibrinogen levels with cigarette smokers. Med J Aust 1(20):617–620
Meade TW, Chakrabarti R, Haines AP, North WR, Stirling Y (1979) Characteristics affecting fibrinolytic activity and plasma fibrinogen concentrations. Br Med J 1(6157):153–156
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors did not receive any sources of financial support for the study, including provision of supplies or services from a commercial organization.
Rights and permissions
About this article
Cite this article
Araco, F., Gravante, G., Sorge, R. et al. Risk evaluation of smoking and age on the occurrence of postoperative erosions after transvaginal mesh repair for pelvic organ prolapses. Int Urogynecol J 19, 473–479 (2008). https://doi.org/10.1007/s00192-007-0476-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-007-0476-8