Abstract
The social distancing policy is an effective way to prevent the spread of infectious diseases in the initial phase of their outbreak when medical evidence to support a particular course of treatment is deficient. While studies on the coronavirus disease 2019 (COVID-19) have mainly focused on the effects of specific measures (e.g., school and workplace closures and restrictions on movement), few investigated the characteristics of epidemic trends in response to the intensity of the policy and the amount of time required for policy measures to take effect. This study employs the SIRD (susceptible, infected, recovered, and deceased) model to analyze the COVID-19 epidemic trend according to the intensity of the social distancing policy in South Korea. The model reveals that the reproduction number began at 5.58 and fluctuated between 0.14 and 1.72 during the study period in accordance with different policy intensities. At the beginning of the social distancing policy, restrictions on public facility use were likely to have been effective in preventing the spread of COVID-19. When the intervention was relaxed, the transmission potential increased significantly. According to the reproduction number, social distancing policies prove to be effective after 13–19 days of implementation; however, as the pandemic progressed, this period extended from 13–14 to 18–19 days for the same effect. This suggests that governments need to consider not only the intensity of the social distancing policy, but also people’s low responsiveness as the pandemic remains prevalent over time. It is also recommended they take preemptive action to ensure sufficient time for the policy to achieve its stated goal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
A novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, hereafter COVID-19), emerged from the city of Wuhan, Hubei, China, in early December 2019 (Chan et al. 2020). Chinese health authorities shut down the Huanan Seafood Market, the suspected source of the virus (Hui et al. 2020), and restricted travel to and from the Hubei Province (Chen et al. 2020). Closing workplaces and prohibiting community activities after school as part of the social distancing policy were first implemented in Wuhan in response to the COVID-19 outbreak (Prem et al. 2020). Afterward, social distancing became the most widely used intervention against the spread of COVID-19 in its early stage as no vaccine had been developed (Newbold et al. 2020).
Several studies have shown that social distancing effectively prevents or controls the spread of infectious diseases by reducing physical contact (Abel and McQueen 2020). According to Ahmed et al. (2018), social distancing reduces the cumulative infection rate in the workplace by about 23%. Prem et al. (2020) further argued that premature and sudden lifting of the intervention could lead to another epidemic wave.
To scientifically assess the effectiveness of the social distancing policy, epidemiologists often refer to a reproduction number (R0). It represents how fast an epidemic spreads through the population, and implementing social distancing is known to lower R0. The reproduction number changes depending on the intensity of social distancing measures, which creates different epidemic trends. The intensity of the policy varies by the level of restrictions on travel, restriction on public or private multi-use space operation, and gathering size. These different levels of social distancing measures lead to increased or decreased R0 (Wang et al. 2020).
However, social distancing policies themselves are not a cure-all solution. Because epidemics are not easily suppressed within a short period, people’s willingness to follow recommended measures can decrease as the policy lasts for a longer period of time (Blendon et al. 2004). In addition, other social problems may exist, including physical and psychological adverse effects from decreased social interaction due to restriction of common spaces (Honey-Rosés et al. 2020; Jurblum and Castle 2020). Therefore, a stepwise approach is required to minimize potential COVID-19 risks when implementing social distancing measures, considering the temporal and spatial effects.
A few studies have investigated changes in R0 depending on different intensities of social distancing policies; however, the extent to which R0 varies with policy intensity via spatial distinctions has not been sufficiently researched. The effects of social distancing policies over time have also not been adequately investigated. For instance, since the COVID-19 incubation period is acknowledged as 14 days (Ma et al. 2012), it is considered that the policy effect takes 14 days to manifest. To our knowledge, however, this time lag of the social distancing policy has not been empirically studied.
In this context, this study aims to analyze the R0 depending on different intensities of social distancing measures and spreading patterns of the virus during the initial stage of the pandemic. The study sets the following two research questions:
-
A spatial perspective how does the policy intensity regarding the use of public and private multi-use facilities affect the spread pattern of the epidemic?
-
A temporal perspective how long will it take the social distancing policy to be effective, and how does the epidemic trend differ during the pandemic?
To this end, this study attempts to investigate changes in the reproduction number in accordance with policy measures and the number of days required for the measures to be effective by analyzing the social distancing intervention and epidemic trends in South Korea.
2 Literature review
2.1 Policy interventions for infectious diseases
In response to the impact of the COVID-19 pandemic, countries implemented their anti-contagion policies and systems based on lessons from former epidemics, adopting policies from other countries, and the diffusion of ideas across governments (Anttiroiko 2021). Several studies proved that social distancing policies reduced the transmission potential of the pandemic (Prem et al. 2020) and directly affected the spread to make a flattening curve (Crokidakis 2020). Severe acute respiratory syndrome (SARS), which globally spread from November 2002 to February 2003, had been transmitted through droplets of respiratory fluids between humans in close proximity to one another. Hong Kong, one of the regions substantially affected by the disease, tracked confirmed cases and adopted home quarantine policies to minimize the transmission potential (Law et al. 2020). The Hong Kong government widely encouraged using face masks, sanitizing hands, and other simple hygiene measures and advised postponing all non-essential travel to Hong Kong and Guangdong.
Middle East Respiratory Syndrome (MERS), another viral respiratory disease, had spread significantly in South Korea. Previous studies (Ha 2020; Khan et al. 2015; Petersen et al. 2015) reported that a large number of cases in the country resulted from (1) delayed information share of confirmed cases and close contact lists, (2) lack of detailed information shared, (3) undervaluing its spread at the community level, and (4) inadequate responses to MERS. Considering the lessons from MERS, South Korea has been equipped with a systematic quarantine system and contributed to utilizing relevant information systems. For COVID-19, South Korea has adopted the 3 T (Test, Trace, and Treat) method (Her 2020; Kim 2021) and social distancing measures following the COVID-19 outbreak.
COVID-19 is known to spread easily in urban spaces with 3C conditions, i.e., crowded places, close-contact settings, and confined and enclosed spaces (WHO 2021). As such, people are advised to avoid the “three Cs” places, mandatorily wear face masks, and keep a distance of two meters from others in indoor/outdoor environments. In addition, urban spaces and public transportation were not allowed in highly populated cities and compact urban structures. These measures effectively controlled the transmission in densely populated cities and countries (Ahmed et al. 2018; Anttiroiko 2021; Tian et al. 2020). School closures, work from home, social distancing policies (including canceling public and group events and restrictions on public gatherings), stay at home, lockdown, border closure, and self-quarantine have been widely implemented for COVID-19 prevention (Anttiroiko 2021; Newbold et al. 2020).
The policies controlling SARS and MERS worked more effectively due to their characteristics (i.e., infection rate, fatality rate, and others). For example, R0 of the SARS epidemic in Hong Kong was 2.7 (Riley et al. 2003), meaning one SARS-infected person passes the virus onto an average of 2.7 people, and that of MERS was 0.8–1.3 (Cauchemez et al. 2014). The R0 of COVID-19 has been reported differently, for example, 3.1 by Wang et al. (2020) and 2.2 by Li et al. (2020). In essence, hosts infected with SARS and MERS were unable to travel great distances due to their higher fatality rate, but COVID-19 cases spread readily due to their low fatality rate (Guarner 2020). The difference is the point at which social distancing policies and travel restrictions for COVID-19 became more significant compared to that for prior respiratory diseases.
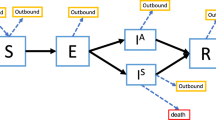
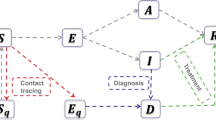
2.2 Modeling studies analyzing the spread of infectious diseases
Studies on the spread of infectious diseases have widely employed deterministic compartment models, statistical models, and deep learning models. In epidemiological studies, the deterministic compartment models, such as SIR (susceptible–infected–recovered), SEIR (susceptible–exposed–infected–removed), and SIRD (susceptible–infected–recovered–deceased) models (Ayodele et al. 2021), have been validated. The models are suitable for predicting the spread rate of infectious disease as they consider the occurrence, infection rate, incubation period, and recovery rate of individuals in an area under the same external conditions. Wu et al. (2020) used the SEIR model to predict the clinical severity of each age group in Wuhan, China, by adjusting the COVID-19 confirmation rate and time from symptom onset to death. Similarly, Wang et al. (2020) used the SEIR model to determine the transmission route within Wuhan, arguing that strong government policies such as movement control effectively prevent infectious disease transmission. As such, the deterministic compartmental model is suitable for macro-prediction of the spread of infectious diseases and aids in implementing appropriate policies.
For the statistical model (e.g., regression model and survival analysis), Kraemer et al. (2020) examined the impact of unprecedented policy interventions, such as travel restrictions, in China using a generalized linear model (GLM). The study used real-time mobility data and travel history of Wuhan and found that China’s drastic control measures effectively halted the spread of COVID-19. Thai et al. (2020) employed survival analysis to examine the median duration of hospitalization in Vietnam. The data gathered from 133 patients showed that the median day of hospitalization was 21 days. Among others, age, residential location, and sources of infection were strongly correlated with a longer hospital stay.
Deep learning models, which have become increasingly popular in recent years, are flexible models outside the constraints of the mathematical model and reflect several variables, including urban and demographic characteristics, using a large amount of observational data. These models outperform others in terms of predictive performance. Hu et al. (2020) developed a real-time deep learning model for short-term forecasting of confirmed cases in 31 Chinese provinces. This model attempted to cluster the patient characteristics using a k-means algorithm and spatially and hierarchically reported the analysis results.
Although statistical models are popular in epidemiology studies, they are limited in their use due to the potential of omitted variable bias (Canning et al. 2020) and an ambiguous start and endpoint for patients (Schober and Vetter 2018). Additionally, survival analysis is particularly irrelevant in examining various phases in relation to different intensities of the policy. Deep learning models have high predictive accuracy, but they require a large amount of data and have the disadvantage of being difficult to explain. Therefore, this study employs the SIRD model, one of the deterministic compartment models. It is suitable as a single macro-model and has been recommended for analyzing the time series effect of the policy as it predicts epidemic trends and infection rates.
3 Analysis
3.1 Data
This study obtained the daily data of South Korean COVID-19 cases from the Korea Centers for Disease Control and Prevention (KCDC) ranging from January 20, 2020, when the first confirmed case was reported, to June 30, 2020. The study analyzed the numbers of daily cases of infection, death, and recovery. The data were spatially divided into 17 major cities and provinces, and the nationwide data were created by combining them.
3.2 Social distancing policy in South Korea
South Korea implemented different levels of social distancing policy. After the first confirmed case was reported on January 20, 2020, the country’s crisis alert was raised to the highest level on February 23rd as local transmission began. Accordingly, a social distancing campaign was initiated on February 29th. The campaign adjusted the intensity levels of the policies according to the changing number of confirmed cases. Specifically, the South Korean government adopted three levels of social distancing policy until mid-June: “enhanced social distancing” (March 22nd–April 19th), “relaxed social distancing” (April 20th–May 5th), and “distancing in daily life” (May 6th–June 27th).
Figure 1 shows the number of patients who received COVID-19 treatment in South Korea, the numbers of deaths and recoveries, and five phases of the South Korean social distancing policy. A general trend and minor fluctuations are presented according to the policy intensity.
3.2.1 Phase 1
South Korea’s social distancing policy began on February 28, 2020, with a campaign by the Korean Medical Association called “Let’s refrain from outdoor activities and stay home like a big snow day.” The campaign officially lasted from February 29 to March 21, 2020, owing to the governmental restrictions on the use of public facilities. As shown in Table 1, professional sports were banned as they attract a large number of spectators, and national parks and public facilities were temporarily closed. Flexible working and telecommuting were generally recommended and implemented for public officials. The reopening of primary and secondary schools was officially postponed for a week, and daycare centers, kindergartens, and extracurricular programs were not allowed to operate.
3.2.2 Phase 2
In Phase 1, the daily number of confirmed COVID-19 cases peaked on March 15, 2020, and then began a downward trend. However, the South Korean government implemented an enforced social distancing policy to prevent the transmission potential of COVID-19 in Seoul and its surrounding areas. The government announced an administrative order to ban all gatherings and events over 50 people (indoor) or 100 people (outdoor) and close social facilities like entertainment bars. Under the administrative order, the local government was forced to place an injunction against any violation of the administrative guidance. Flexible working and telecommuting were expanded to more public and private companies.
3.2.3 Phase 3
After the spread of the infectious disease was alleviated in the capital region through Phase 2, the South Korean government lifted the intensity of the policy on April 20, 2020. First, the government partially resumed operation of public facilities with a relatively low risk (e.g., professional baseball games without spectators and reopening outdoor national parks) under the conditions of disease control standards and encouraging people to keep a safe distance. In the case of the private sector, educational test centers were partially reopened with qualified disease control standards. For those facilities with a high risk of transmission, such as entertainment, sports, and religious facilities, the intensity of the administrative order was relaxed from mandatory to recommended.
3.2.4 Phase 4
The South Korean government eased the policy intensity on May 6, 2020, in consideration of the declining trend in new COVID-19 cases. A limited number of spectators were allowed to enter professional baseball stadiums, and high-risk facilities such as entertainment bars were reopened. Some students were allowed to physically attend classes, and others joined parallel online classes. For workplaces, flexible working hours and telecommuting were not as strongly recommended. However, as soon as Phase 4 measures were effectuated, infected individuals whose disease remained latent in Phase 3 began to show symptoms. The total confirmed COVID-19 cases continually increased since the mass infection and were linked to nightclubs (bars) on May 6th and reached their peak of 1,324 cases on June 23rd.
3.2.5 Phase 5
The government introduced a higher level of social distancing policy on May 29th to mitigate the increasing number of confirmed cases in the capital region. More intensive individual preventive measures were requested at Phase 5. Wearing face masks became mandatory once again on public transportation (subway, buses, and taxis), and passengers without masks were not allowed.
3.3 Method
This study employed SIRD (Susceptible, Infected, Recovered, and Deceased) modeling based on South Korean COVID-19 data to identify the S–R trend. The SIRD model was run in a Python library called CovsirPhy (CovsirPhy 2020), which allows changes to be captured in the spread of COVID-19 at major time points.
3.3.1 SIRD model
The SIRD model is a deterministic mathematical model for describing the spread of infectious diseases. The total population is divided into four groups: susceptible (S), infected (I), recovered (R), and deceased (D) cases. Susceptible cases are calculated by subtracting the infected cases from the population, implying that the remainder has the potential to become newly infected cases through contacts with the infected. The probability of contact with someone infected is determined by the value calculated through the change in the number of infected cases over time in the model. Infected cases include the asymptomatic infections that have been confirmed to be infected. Recovered cases are the number of people who have been infected and then recovered. Deceased cases refer to those who died after infection.
where S: susceptible, I: infected, R: recovered, D: deceased, α: mortality rate [1/min], β: effective contact rate [1/min], and γ: recovery rate [1/min].
The SIRD model estimates the population growth in each stage based on the α, β, and γ parameters. The model is constructed as a function of time, and the ordinary differential equations (ODE) for the four groups are as follows.
where N (= S + I + R + D) refers to the total population and T to elapsed time from the start date.
This study utilized a non-dimensional SIRD model in which the unit of the variable is excluded to simplify the model (CovsirPhy 2020).
3.3.2 Susceptible–recovered (S-R) trend
The S–R trend detects the time point at which there are changes in the trend of the COVID-19 infection, and then assumes the parametric change of the SIRD model at that point (CovsirPhy 2020). The relationship between S and R can be summarized as follows:
then,
where α is the slope of the model, which is determined according to the changes of the β and γ parameters. In the bottom equation, log S is reduced as R increases when the parameters of the model are constants.
3.4 Model analysis process
In comparing the initial five phases of the social distancing policy in South Korea, this study focused on the reproduction number to evaluate the effectiveness of each phase and estimate the elapsed time for the policy to have an effect. The reproduction number is defined as the degree of transmission at time t and the average number of secondary infections caused by an infected patient. Suppose the reproduction number at time t is equal to or greater than 1.0. In that case, it implies that the disease continues to spread, and if it is less than 1.0, the transmission is expected to decrease.
The reproduction number may vary depending on whether pharmaceutical or non-pharmaceutical control measures are implemented. At a point when vaccines have yet to be developed, non-pharmaceutical measures can be viable tools to prevent the spread of infectious diseases. This study investigated time points at which the reproduction number changes and examined how each period between the points overlaps with the five phases of the social distancing policy. Figure 2 shows the analytical process of this study.
4 Results
4.1 Changes in the COVID-19 epidemic trend
Figure 3 shows changes in the S-R trend. It is classified into eight sections, and a linear trend line for each section is a measure of scale for the COVID-19 outbreak. A section with a sharply sloped trend line indicates that there was rapid transmission of COVID-19 in that period.
The dates on the figure are the start date of each section. With the exception of the initial stage, the trend line gently declines. This study identified the epidemic trend with the start and end dates of the period and the time-dependent reproduction number for each period in connection with the COVID-19 policy responses (Phases 1–5), as shown in Table 2.
Rt shows time-dependent changes with the policy phases. The 0th stage has the highest reproduction number (Rt = 5.58) because the number of infected cases increased substantially in selected areas in the early stage of the COVID-19 outbreak in South Korea. However, in the 1st stage, Rt sharply dropped to 0.33 after 14 days of the implementation of Phase 1. The COVID-19 incubation period is commonly defined as 14 days (Ma et al. 2012); therefore, the sharp reduction in Rt indicates that the Phase 1 response was indeed effective in mitigating the COVID-19 spread. Accordingly, in the 4th stage, the Rt fell to 0.14 after the intensive social distancing policies were implemented at Phase 2.
As the government relaxed the social distancing policy at Phase 3, Rt in the 5th stage rose slightly from 0.14 to 0.48, but Rt still remained below 1.0. Consequently, the South Korean government soon implemented the lowest level of the social distancing policy in Phase 4.
In the 6th stage, Rt increased to 1.87, which suggests that the social distancing policy carried out at Phase 4 was insignificant in preventing the spread of COVID-19. Recognizing the severity of the pandemic crisis, the central government decided to restrengthen the social distancing policy at Phase 5. Then, infected cases began to decrease (Rt = 0.79) in the 7th stage due to a more strengthened Phase 5 distancing policy.
4.2 Effectiveness of the social distancing policy
Figure 4 presents COVID-19 cases over time with an overlap of social distancing policies and epidemic trends. The analysis of policy implementation periods and changes in epidemic trends indicates that the transmission trend changes after 13–19 days from the policy implementation; this policy lag is similar to the generally accepted COVID-19 incubation period of 14 days (Ma et al. 2012). That is, social distancing policies may not exert immediate effects, but require a time lag of two weeks. A related study that examined the COVID-19 policy responses of the US government found that 9–12 days are required for the responses to initiate meaningful effects (Badr et al. 2020).
Notably, the period of time required for the policy to initiate its effect differed between the earlier and later phases. The time lag at Phases 1 and 2 was 14 and 13 days, respectively, while the lag at each of the latter three phrases was 19, 18, and 19 days. Compared with the preceding phases, the lag was extended by 5 to 6 days.
4.3 Predictive modeling
Figure 5 shows variations in the number of predicted infected cases based on Rt for 28 days at Phases 3–5: blue line for Rt of the 4th stage (0.14), orange for the 5th (0.48), green for the 6th (1.72), and red for 7th (0.79). As shown, the number of newly infected cases is moderately reduced at the 6th–7th stage and the Rt value remains under 1.0. At the 6th stage, Rt (1.72) shows a sudden increase along with the previous upward curve. These results imply that if social distancing policies of Phase 2 or 3 had been extended, the increase in the number of infected cases after Phase 4 would have been delayed. Additionally, if the transition from Phase 4 to Phase 5 had been delayed in time, the number of confirmed cases might have increased more rapidly.
5 Discussion and conclusion
This study compared different intensities of social distancing measures and the epidemic trend in South Korea from January 20th to June 30th of 2020 and took a spatial and temporal approach to evaluate their effects on the early stage of the COVID-19 pandemic. Based on the findings of this study, several policy implications can be drawn from South Korea’s experience.
First, as a spatial approach, it is vital to restrict public facility operation during the initial stages of the spread of an epidemic and then consider restrictions on the use of private multi-use facilities, such as entertainment and sports facilities in densely populated areas. The vigorous public intervention effectively halted the early spread of COVID-19. In other words, minimized public intervention and advocates for individual preventive measures are ineffective at preventing the spread of infectious disease. An empirical SIRD model presented epidemic trends in association with different intensities of the social distancing policies. The policies and epidemic trends were divided into five phases and eight stages, respectively, from January 20 to June 30, 2020. Accordingly, this study found that highly restrictive social distancing measures for both public and private sectors reduced the spread of COVID-19, and the epidemic spread is facilitated when the intensity of the policies is relaxed.
Phase 1 shows that restrictions on the use of public facilities were quite effective at containing the epidemic (Rt 5.58 → 0.33). However, despite governmental efforts, regional-level infections persisted in densely populated areas like the Seoul metropolitan area (Rt 0.33 → 0.39). The transmission of infectious disease in densely populated areas began to be clearly controlled through an executive order prohibiting public and private gatherings of 50 or more people in indoor spaces and 100 or more people in outdoor spaces for any purpose. It is noteworthy that Rt surged from 0.14 to 0.48 to 1.72 as the policies were loosened.
Second, as a temporal approach, policymakers need to consider that people become unresponsive to the recurrent implementation of similar regulations. The epidemic trends showed changes in the time lag for the distancing policies to be effective. The average time lag was 13–19 days, yet it was 13–14 days in the early stages of COVID-19 and 18–19 days later. The changes in time lag duration may have been attributed to changes in public awareness, as the risk perception that is correlated with people’s willingness and motivation to follow preventive actions (Weinstein 1988) is known to decrease over time (Blendon et al. 2004). In addition, the repeated implementation of intensive social distancing policies due to several mass infections of COVID-19 (at Phases 3 and 4) may have reduced people’s willingness to follow the social distancing policy.
The longer the pandemic period, the longer the time lag for the distancing policies will be effective. This change was witnessed in the third epidemic wave of COVID-19 in South Korea in late 2020 and early 2021. The central government enforced the social distancing policy of level 2.5 (a total of 5 levels from 1 to 3 with 0.5 intervals) on December 8, 2020. Nevertheless, the number of confirmed cases continued to increase, and the daily number of confirmed cases peaked on December 25, 2020 (1241 cases). The reproduction number, which once soared to 1.52, has fallen to less than one since January 3, 2021. At that time, the time lag was recorded as 25 days. In this sense, further research is required to analyze people’s perceptions and behaviors toward social distancing policies to improve the effectiveness of non-pharmaceutical measures.
Third, more preemptive measures are required to keep the reproduction number below 1.0 in densely populated areas. This study predicted how infected cases would change if stronger social distancing measures continued for the 4th to 7th epidemic stages. The distancing policy in Phase 4 lost its effectiveness as the reproduction number exceeded 1.0 and infected cases rapidly increased. This was particularly prominent in densely populated areas. Therefore, in those areas, it is desirable to preemptively take preventive measures prior to the reproduction number exceeding 1.0 in consideration of the rapid increase in the reproduction number.
This study is not without limitations. First, it failed to consider mass infections by super-spreaders. In the early stages of the COVID-19 outbreak in South Korea, massive group infections were present in some areas. However, the epidemic model employed in this study could not reflect the regional explosion of the infections. In this context, planning and geography-specific suggestions might be drawn by conducting follow-up studies on the effect of social distancing policy considering regional-level characteristics. Second, the average value of the reproduction number was taken at each stage, but it dynamically changes at a finer grain (e.g., by day). Therefore, future studies are recommended to examine area-specific infection cases at a micro-temporal unit scale.
Despite the above limitations, this study contributes to the literature by comprehensively examining social distancing measures over six consecutive months to draw policy implications. To effectively prevent the spread of COVID-19, the intensity of the policy and its differential time lag should be carefully considered together for the expected effects of the policy to occur.
References
Abel T, McQueen D (2020) The COVID-19 pandemic calls for spatial distancing and social closeness: not for social distancing! Int J Public Health 65(3):231. https://doi.org/10.1007/s00038-020-01366-7
Ahmed F, Zviedrite N, Uzicanin A (2018) Effectiveness of workplace social distancing measures in reducing influenza transmission: a systematic review. BMC Public Health 18(1):1–13. https://doi.org/10.1186/s12889-018-5446-1
Anttiroiko AV (2021) Successful government responses to the pandemic: contextualizing national and urban responses to the COVID-19 outbreak in east and west. Int J E-Planning Res 10(2):1–17. https://doi.org/10.4018/IJEPR.20210401.oa1
Ayodele KP, Jimoh H, Fagbamigbe AF et al (2021) The dynamics of COVID-19 outbreak in Nigeria: a sub-national analysis. Sci Afr 13(January):e00914. https://doi.org/10.1016/j.sciaf.2021.e00914
Badr HS, Du H, Marshall M et al (2020) Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect Dis 3099(20):1–8. https://doi.org/10.1016/S1473-3099(20)30553-3
Blendon RJ, Benson JM, DesRoches CM et al (2004) The public’s response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis 38(7):925–931. https://doi.org/10.1086/382355
Canning D, Karra M, Dayalu R, Guo M, Bloom DE (2020) The association between age, COVID-19 symptoms, and social distancing behavior in the United States. MedRxiv : The Preprint Server for Health Sciences. https://doi.org/10.1101/2020.04.19.20065219
Cauchemez S, Fraser C, Van Kerkhove MD et al (2014) Middle East respiratory syndrome coronavirus: Quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis 14(1):50–56. https://doi.org/10.1016/S1473-3099(13)70304-9
Chan JFW, Yuan S, Kok KH et al (2020) A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395(10223):514–523. https://doi.org/10.1016/S0140-6736(20)30154-9
Chen S, Yang J, Yang W et al (2020) COVID-19 control in China during mass population movements at New Year. Lancet 395(10226):764–766. https://doi.org/10.1016/S0140-6736(20)30421-9
CovsirPhy Development Team (2020) CovsirPhy, Python package for COVID-19 analysis with SIR-derived ODE models, https://github.com/lisphilar/covid19-sir
Crokidakis N (2020) COVID-19 spreading in Rio de Janeiro, Brazil: do the policies of social isolation really work? Chaos Solitons Fractals 136:109930. https://doi.org/10.1016/j.chaos.2020.109930
Guarner J (2020) Three emerging coronaviruses in two decades: the story of SARS, MERS, and Now COVID-19. Am J Clin Pathol 153(4):420–421. https://doi.org/10.1093/ajcp/aqaa029
Ha KM (2020) A lesson learned from the MERS outbreak in South Korea in 2015. J Hosp Infect 92(3):232
Her M (2020) How Is COVID-19 affecting South Korea? What Is our current strategy? Disast Med Public Health Prep 14(5):684–686. https://doi.org/10.1017/dmp.2020.69
Honey-Rosés J, Anguelovski I, Chireh VK, Daher C, Konijnendijk van den Bosch C, Litt JS, Nieuwenhuijsen MJ (2020) The impact of COVID-19 on public space: an early review of the emerging questions–design, perceptions and inequities. Cities Health. https://doi.org/10.1080/23748834.2020.1780074
Hu Z, Ge Q, Li S et al (2020) Artificial intelligence forecasting of Covid-19 in China. Int J Edu Excell 6(1):71–94. https://doi.org/10.18562/ijee.054
Hui DS, Azhar EI, Madani TA et al (2020) The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health: the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis 91:264–266. https://doi.org/10.1016/j.ijid.2020.01.009
Jurblum M, Ng CH, Castle DJ (2020) Psychological consequences of social isolation and quarantine: issues related to COVID-19 restrictions. Aust J Gener Pract 49(12):778–783. https://doi.org/10.3316/informit.638701007415032
Khan A, Farooqui A, Guan Y et al (2015) lessons to learn from mers-cov outbreak in South Korea. J Infect Dev Ctries 9(6):543–546. https://doi.org/10.3855/jidc.7278
Kim PS (2021) South Korea’s fast response to coronavirus disease: implications on public policy and public management theory. Public Manag Rev 23(12):1736–1747. https://doi.org/10.1080/14719037.2020.1766266
Kraemer MUG, Yang CH, Gutierrez B et al (2020) The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 368(6490):493–497. https://doi.org/10.1126/science.abb4218
Law S, Leung AW, Xu C (2020) Severe acute respiratory syndrome (SARS) and coronavirus disease-2019 (COVID-19): from causes to preventions in Hong Kong. Int J Infect Dis 94:156–163. https://doi.org/10.1016/j.ijid.2020.03.059
Li Q, Guan X, Wu P et al (2020) Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 382(13):1199–1207. https://doi.org/10.1056/NEJMoa2001316
Ma S, Zhang J, Zeng M, et al. (2012) Epidemiological parameters of coronavirus disease 2019: a pooled analysis of publicly reported individual data of 1155 cases from seven countries. medRxiv: 1–21
Newbold SC, Finnoff D, Thunström L et al (2020) Effects of physical distancing to Control COVID-19 on public health, the economy, and the environment. Environ Resource Econ 76(4):705–729. https://doi.org/10.1007/s10640-020-00440-1
Petersen E, Hui DS, Perlman S et al (2015) Middle East Respiratory Syndrome- advancing the public health and research agenda on MERS- lessons from the South Korea outbreak. Int J Infect Dis. https://doi.org/10.1016/j.ijid.2015.06.004
Prem K, Liu Y, Russell TW et al (2020) The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health 5(5):e261–e270. https://doi.org/10.1016/S2468-2667(20)30073-6
Riley S, Fraser C, Donnelly CA et al (2003) Transmission dynamics of the etiological agent of SARS in Hong Kong: impact of public health interventions. Science 300(5627):1961–1966. https://doi.org/10.1126/science.1086478
Schober P, Vetter TR (2018) Survival analysis and interpretation of time-to-event data: the tortoise and the hare. Anesth Analg 127(3):792–798. https://doi.org/10.1213/ANE.0000000000003653
Thai PQ, Toan DTT, Dinh TS, Van Hoang TH, Luu NM, Xuan Hung L, Ngo VT, Luu NH, Duong HL, Luong NK, Nguyen TK, Le TH (2020) Factors associated with the duration of hospitalization among COVID-19 patients in Vietnam: a survival analysis. Epidemiol Infect. https://doi.org/10.1017/S0950268820001259
Tian H, Liu Y, Li Y et al (2020) An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science 368(6491):638–642. https://doi.org/10.1126/science.abb6105
Wang H, Wang Z, Dong Y et al (2020) Phase-adjusted estimation of the number of Coronavirus Disease 2019 cases in Wuhan, China. Cell Discov 6(1):4–11. https://doi.org/10.1038/s41421-020-0148-0
Weinstein ND (1988) The precaution adoption process. Health Psychol 7(4):355–386. https://doi.org/10.1037/0278-6133.7.4.355
World Health Organization (WHO) (2021). Coronavirus disease (COVID-19): How is it transmitted? https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted. Accessed 30 Jan, 2022
Wu JT, Leung K, Bushman M et al (2020) Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med 26(4):506–510. https://doi.org/10.1038/s41591-020-0822-7
Acknowledgements
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2021S1A3A2A01087370).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, MH., Lee, J., Oh, HJ. et al. A modeling study of the effect of social distancing policies on the early spread of coronavirus disease 2019: a case of South Korea. Ann Reg Sci 71, 225–242 (2023). https://doi.org/10.1007/s00168-022-01140-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00168-022-01140-y