Abstract
Purpose
The treatment for symptomatic intact discoid lateral meniscus (DLM) is controversial and the long-term clinical outcome remains unknown. The purpose of this study was to analyze the overall failure rate of nonsurgical treatment for symptomatic intact DLM and identify the risk factors for nonoperative management failure.
Methods
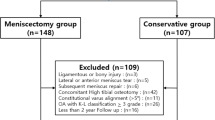
Consecutive patients who underwent nonsurgical treatment for symptomatic intact DLM at our hospital from 2014 to 2017 were retrospectively reviewed. Patients were divided into Group A (failure group) and Group B (nonfailure group) based on overall failure criteria: conversion to surgery, progression of a tear on MRI re-examination, or severely abnormal International Knee Documentation Committee (IKDC) scores. Statistical analyses between the two groups were performed for demographic and radiographic characteristics. Multivariate regression analysis was used to determine the risk factors associated with worse outcomes.
Results
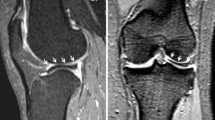
One-hundred and four knees in 96 patients were included in this study. After a mean follow-up of 76.9 ± 11.1 months, 25 knees (24.0%) met the overall failure criteria. Multivariate regression analysis demonstrated that age and the presence of intrameniscus signals increased the risk of nonoperative management failure. The clinical criterion of age > 37.5 years combined with the imaging criterion of the presence of intrameniscal signals predicted conservative treatment failure of symptomatic intact DLM with a sensitivity of 0.87 and a specificity of 0.91.
Conclusion
Twenty-five (24.0%) knees that underwent nonsurgical treatment met the overall failure criteria after a mean follow-up of 76.9 months. With increased age and the presence of intrameniscal signals, the nonoperative results become worse.
Level of evidence
III.




Similar content being viewed by others
Data availability
The data of this study are not openly available due to the protection of patients’ privacy and are available from the corresponding author upon reasonable request.
Abbreviations
- DLM:
-
Discoid lateral meniscus
- BMI:
-
Body mass index
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating characteristic
- IKDC:
-
International Knee Documentation Committee
- CI:
-
Confidence interval
- ICC:
-
Intraclass correlation coefficient
References
Araki Y, Yamamoto H, Nakamura H, Tsukaguchi I (1994) MR diagnosis of discoid lateral menisci of the knee. Eur J Radiol 18:92–95. https://doi.org/10.1016/0720-048x(94)90271-2
Bisicchia S, Botti F, Tudisco C (2018) Discoid lateral meniscus in children and adolescents: a histological study. J Exp Orthop 5:39. https://doi.org/10.1186/s40634-018-0153-5
Campbell AL, Pace JL, Mandelbaum BR (2023) Discoid lateral meniscus. Curr Rev Musculoskelet Med 16:154–161. https://doi.org/10.1007/s12178-023-09824-4
Chen L, Zheng JJY, Li G, Yuan J, Ebert JR, Li H, Papadimitriou J, Wang Q, Wood D, Jones CW, Zheng M (2020) Pathogenesis and clinical management of obesity-related knee osteoarthritis: impact of mechanical loading. J Orthop Translat 24:66–75. https://doi.org/10.1016/j.jot.2020.05.001
Fu D, Guo L, Yang L, Chen G, Duan X (2014) Discoid lateral meniscus tears and concomitant articular cartilage lesions in the knee. Arthroscopy 30:311–318. https://doi.org/10.1016/j.arthro.2013.11.029
Hesse DG, Finlayson CJ, Gladstein AZ, Samet JD (2021) Pediatric discoid meniscus: can magnetic resonance imaging features coupled with clinical symptoms predict the need for surgery? Pediatr Radiol 51:1696–1704. https://doi.org/10.1007/s00247-021-05063-2
Irrgang JJ, Ho H, Harner CD, Fu FH (1998) Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:107–114. https://doi.org/10.1007/s001670050082
Jeon SW, Choi CH, Jung M, Chun YM, Kim SJ, Jin S, Kim SH (2019) The fate of the contralateral knee in patients with a lateral discoid meniscus. Arthroscopy 35:500–506. https://doi.org/10.1016/j.arthro.2018.07.045
Kleinhans KL, Jackson AR (2018) Hydraulic permeability of meniscus fibrocartilage measured via direct permeation: effects of tissue anisotropy, water volume content, and compressive strain. J Biomech 72:215–221. https://doi.org/10.1016/j.jbiomech.2018.03.011
Kocher MS, Logan CA, Kramer DE (2017) Discoid lateral meniscus in children: diagnosis, management, and outcomes. J Am Acad Orthop Surg 25:736–743. https://doi.org/10.5435/jaaos-d-15-00491
Kose O, Celiktas M, Egerci OF, Guler F, Ozyurek S, Sarpel Y (2015) Prognostic factors affecting the outcome of arthroscopic saucerization in discoid lateral meniscus: a retrospective analysis of 48 cases. Musculoskelet Surg 99:165–170. https://doi.org/10.1007/s12306-015-0376-x
Laberge MA, Baum T, Virayavanich W, Nardo L, Nevitt MC, Lynch J, McCulloch CE, Link TM (2012) Obesity increases the prevalence and severity of focal knee abnormalities diagnosed using 3T MRI in middle-aged subjects–data from the osteoarthritis initiative. Skeletal Radiol 41:633–641. https://doi.org/10.1007/s00256-011-1259-3
Lee CR, Bin SI, Kim JM, Kim NK (2016) Magnetic resonance imaging findings in symptomatic patients after arthroscopic partial meniscectomy for torn discoid lateral meniscus. Arthroscopy 32:2366–2372. https://doi.org/10.1016/j.arthro.2016.04.012
Logan CA, Tepolt FA, Kocher SD, Feroe AG, Micheli LJ, Kocher MS (2021) Symptomatic discoid meniscus in children and adolescents: a review of 470 cases. J Pediatr Orthop 41:496–501. https://doi.org/10.1097/bpo.0000000000001907
Masquijo JJ, Bernocco F, Porta J (2019) Discoid meniscus in children and adolescents: correlation between morphology and meniscal tears. Rev Esp Cir Ortop Traumatol (Engl Ed) 63:24–28. https://doi.org/10.1016/j.recot.2018.08.002
Mochizuki T, Tanifuji O, Sato T, Watanabe S, Endo N (2021) Predictive factors for developing osteochondritis dissecans after surgery for discoid lateral meniscus are younger age and shorter meniscal width. Knee Surg Sports Traumatol Arthrosc 29:100–108. https://doi.org/10.1007/s00167-019-05750-6
Nesbitt DQ, Siegel DN, Nelson SJ, Lujan TJ (2021) Effect of age on the failure properties of human meniscus: high-speed strain mapping of tissue tears. J Biomech 115:110126. https://doi.org/10.1016/j.jbiomech.2020.110126
Papadopoulos A, Kirkos JM, Kapetanos GA (2009) Histomorphologic study of discoid meniscus. Arthroscopy 25:262–268. https://doi.org/10.1016/j.arthro.2008.10.006
Rai MF, Patra D, Sandell LJ, Brophy RH (2014) Relationship of gene expression in the injured human meniscus to body mass index: a biologic connection between obesity and osteoarthritis. Arthritis Rheumatol 66:2152–2164. https://doi.org/10.1002/art.38643
Sasho T, Tsuruoka H, Saito M, Akagi R, Muramatsu Y, Mukoyama S, Yamaguchi S (2014) Time interval from initial surgery for torn discoid lateral meniscus to the contralateral knee surgery. Asia Pac J Sports Med Arthrosc Rehabil Technol 1:38–41. https://doi.org/10.1016/j.asmart.2013.12.007
Stoller DW, Martin C, Crues JV 3rd, Kaplan L, Mink JH (1987) Meniscal tears: pathologic correlation with MR imaging. Radiology 163:731–735. https://doi.org/10.1148/radiology.163.3.3575724
Sun H, Zhang W, Liu F, Li D, Cai Z, Huang Z, Chen M, Lin Z, Xu J, Ma R (2022) Single-cell RNA sequencing reveals the cell types heterogenicity of human discoid lateral meniscus cells. J Cell Physiol 237:2469–2477. https://doi.org/10.1002/jcp.30704
Tapasvi S, Shekhar A, Eriksson K (2021) Discoid lateral meniscus: current concepts. J ISAKOS 6:14–21. https://doi.org/10.1136/jisakos-2017-000162
Tudisco C, Botti F, Bisicchia S (2021) Histological study of discoid lateral meniscus in children and adolescents: morphogenetic considerations. Joints 7:155–158. https://doi.org/10.1055/s-0041-1730979
Watanabe M, Takeda S, Ikeuchi H (1974) Atlas of arthroscopy, 2nd edn. Igaku-Shoin Ltd, Tokyo
Yamaguchi N, Chosa E, Tajima T, Morita Y, Yokoe T (2022) Symptomatic discoid lateral meniscus shows a relationship between types and tear patterns, and between causes of clinical symptom onset and the age distribution. Knee Surg Sports Traumatol Arthrosc 30:1436–1442. https://doi.org/10.1007/s00167-021-06635-3
Yang S, Zhang S, Li R et al (2023) Chinese experts consensus and practice guideline on discoid lateral meniscus. Orthop Surg 15:915–929. https://doi.org/10.1111/os.13687
Yang SJ, Li J, Xue Y, Zhang Z, Chen G (2021) Multivariate ordered logistic regression analysis of the postoperative effect of symptomatic discoid lateral meniscus. Arch Orthop Trauma Surg 141:1935–1944. https://doi.org/10.1007/s00402-021-03821-3
Young RB (1889) The external semilunar cartilage as a complete disc. Mem Memo Anat 24:613
Zhang F, Bierma-Zeinstra SM, Oei EHG, Turkiewicz A, Englund M, Runhaar J (2017) Factors associated with meniscal body extrusion on knee MRI in overweight and obese women. Osteoarthr Cartil 25:694–699. https://doi.org/10.1016/j.joca.2016.12.001
Zhang Z, Shang XK, Mao BN, Li J, Chen G (2019) Torn discoid lateral meniscus is associated with increased medial meniscal extrusion and worse articular cartilage status in older patients. Knee Surg Sports Traumatol Arthrosc 27:2624–2631. https://doi.org/10.1007/s00167-018-5287-6
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. The database was provided by BJ. Experimental design, data collection, and analysis were performed by ZL, JQ, and XL. MRI image review was performed by XL, YF, and XC. The first draft of the manuscript was written by ZL and ML. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Ethical approval was obtained from the ethics review committee of the Peking Union Medical College Hospital (ID: K23C2228).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, Z., Qian, J., Lu, X. et al. Older age and the presence of intrameniscal signs are risk factors for nonsurgical treatment failure of symptomatic intact discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc 31, 5154–5161 (2023). https://doi.org/10.1007/s00167-023-07586-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07586-7