Abstract
Introduction
The postoperative effect of arthroscopy in the treatment of symptomatic discoid lateral meniscus (DLM) varies greatly among individuals. Therefore, this study aims to investigate the factors affecting the postoperative outcomes of symptomatic DLM.
Materials and methods
According to the inclusion and exclusion criteria, patients with symptomatic single-knee DLM who underwent arthroscopic surgery at our hospital from 9/2008 to 9/2015 were included. Retrospectively collected 16 factors probably affecting postoperative outcomes. The Ikeuchi grade system was used to evaluate the knee joint function. Univariate analysis was performed by Kruskal–Wallis rank-sum test or Mann–Whitney U test, and multivariate analysis by ordered logistic regression. P < 0.05 was considered statistically significant.
Results
A sum of 502 patients was included, including 353 females (70.3%) and 149 males (29.7%). Difference between preoperative and postoperative Ikeuchi grade was statistically significant (P < 0.001). Female was bad to obtain a good Ikeuchi grade (P = 0.009, OR 0.458). Outerbridge grade (P = 0.018, OR 0.638) was negatively correlated with Ikeuchi grade. BMI (P = 0.001, OR 0.875) and work intensity (P = 0.020, OR 0.611) were inversely correlated with Ikeuchi grade. Age of onset (P < 0.001, OR 0.956) and symptoms duration (P < 0.001, OR 0.988) were negatively correlated with Ikeuchi grade. Besides, compared to total meniscectomy, meniscoplasty with a repair was an unfavourable factor for Ikeuchi grade (P = 0.044, OR 0.245).
Conclusions
With the increase of BMI, work intensity, age of onset, duration of symptoms, and the severity of cartilage lesion, the postoperative results become worse. Moreover, female and meniscoplasty with repair are risk factors for the postoperative outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
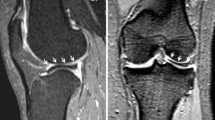
The discoid meniscus has an abnormal shape and structure. The disintegration of the circular collagen fibre system in the discoid meniscus matrix may be responsible for the higher tear rate and higher degeneration of the discoid meniscus compared to the normal meniscus [1]. Clinically, compared with the discoid medial meniscus, discoid lateral meniscus (DLM) is the most common, with a high prevalence in Asian populations (16–20%) [2, 3]; and bilateral DLM accounts for 79–97% [4]. Symptomatic DLM is characterized by pain, swelling, snapping, locking, knee instability and limited mobility [5], which is mainly diagnosed by magnetic resonance imaging (MRI) and treated by arthroscopic surgery [3, 6]. Although the overall postoperative outcomes of symptomatic DLM are acceptable [1, 5, 7, 8], the outcomes between individuals are still largely different, which may result from diversity in patient’s characteristics and treatments [6]. Currently, studies have reported the influencing factors of postoperative arthroscopy for symptomatic DLM, but the results are inconsistent possibly resulted from differences in sample size, studied factors, and knee function evaluation system, etc. [9,10,11]. Therefore, the present research aims to investigate the influential factors of arthroscopic treatment for symptomatic DLM by retrospectively analysing more samples and factors and evaluating the knee function with Ikeuchi grade system that is simple and practical, hoping to provide theoretical basis and clinical guidance for individualized treatment and prediction of postoperative efficacy. The hypothesis is that individual variations and inconsistent treatments of different patients, such as sex, body mass index (BMI), surgical mode, etc., would influence the outcomes of arthroscopic surgery for symptomatic DLM.
Materials and methods
According to the inclusion and exclusion criteria, patients with symptomatic single-knee DLM who underwent arthroscopic surgery at our hospital from 9/2008 to 9/2015 were included. The inclusion criteria, exclusion criteria and flow chart of the study were detailly shown in Fig. 1.
Patients with third-degree DLM lesion classified by Stoller MRI classification [6] and with symptoms such as pain, lock-up, and flexion and extension disorders need arthroscopic surgery. Method of arthroscopic surgery comprises meniscoplasty, meniscoplasty with repair, and total meniscectomy. Meniscoplasty is applied to the patients with continuous circular fibers in DLM, in which the broken part of the white area or red-white area in the free edge of the meniscus is removed, and about a width of 6–8 mm discoid meniscus is retained with a smooth and crescent shape. Meniscoplasty with repair is suitable for the patients with continuous circular fibers in DLM and accompanied by instability or longitudinal tear (< 10 mm) of the synovial margin, in which the torn DLM in synovial margin is repaired by total intraarticular suture method based on the meniscoplasty. Total meniscectomy is appropriate for the patients with discontinuous circular fibers in DLM (e.g. radial tear from synovial margin to free edge), in which the damaged meniscus tissue is removed as the posterior root, body, and anterior root of the meniscus tissue are not continuous, and some unfunctional residual meniscus tissue is retained. The surgical procedures for all patients were performed by the same senior surgeon whose surgical technique was reliable and stable.
The following 16 factors potentially affecting postoperative efficacy were collected from the medical records including imaging data (knee X-ray and MRI), patient history and arthroscopic surgery videos: sex; BMI; work intensity (according to the REFA daily life and work intensity classification [12], Schedule 1); trauma history (DLM lesion because of sports, falls, sprains, etc.); age of onset (years); symptoms duration (months); involved knee joint (left or right); K–L grade (according to the Kellgren–Lawrence Classification of Osteoarthritis [13], Schedule 2); DLM type (according to the Watanabe classification [9], Schedule 3); site of the meniscus tear; type of DLM tear (according to meniscus tear O'Connor classification [14], Schedule 4); combined medial meniscus tear; site of the articular cartilage lesion [including the lateral compartment (lateral femoral condyle and lateral tibial plateau), medial compartment (medial femoral condyle and medial tibial plateau), and patellofemoral joint (patella and trochlea)] [8]; severity of cartilage lesion (according to the Outerbridge grade [15], Schedule 5); mode of arthroscopic surgery (including meniscoplasty, meniscoplasty with repair, and total meniscectomy) and final follow-up time (months). Among the above factors, the intra-articular lesions such as DLM type, DLM tear, cartilage lesion, etc. were judged by arthroscopy. Postoperative efficacy was evaluated by Ikeuchi grade [16], (Schedule 6), the score of which was obtained through regular follow-up by the outpatient visit. The basic characteristics of the included subjects were shown in Table 1. The assignment of 16 factors to be studied and Ikeuchi grade were displayed in Table 2.
The data were statistically analysed by SPSS 25.0. The normality test and homogeneity test of variance revealed that the measurement data does not satisfy the normal distribution and the homogeneity of variance. The measurement data and enumeration data were described by the median (M) and interquartile range (IQR), and the number of cases (percentage), respectively. The difference between the preoperative and postoperative functional assessments was analysed by the Wilcoxon rank-sum test. Univariate analysis: Kruskal–Wallis rank-sum test was used for measurement data among multiple groups; Mann–Whitney U test was applied to different analysis of two-category data, and Kruskal–Wallis rank-sum test to different analysis of rank data between multiple groups. Multivariate analysis: The model meets the parallelism by parallel test, and multivariate analysis was performed by ordinal logistic regression. P < 0.05 was considered statistically significant.
Results
General characteristics of the subjects
In this study, a sum of 502 patients was included, including 353 females (70.3%) and 149 males (29.7%); 252 (50.2%) left knees and 250 (49.8%) right knees. The median age of onset and symptoms duration were 32.0 years (range 3 ~ 80 years; IQR 26.3) and 10.0 months (range 0.05 ~ 246 months; IQR 21.0), respectively. The average follow-up was 75.4 months (range 41.0 ~ 123.3 months). There were 83 patients lost to follow up among 585 subjects, and the lost rate of follow up is 14.2%. According to Ikeuchi grade, preoperatively, 437 patients (87.1%) were rated as fair and 65 (12.9%) as poor; postoperatively, 340 patients (67.7%) were judged as excellent, 105 (20.9%) as good, 44 (8.8%) as fair and 13 (2.6%) as poor. Difference between preoperative and postoperative Ikeuchi grade was statistically significant (P < 0.001). (Table 3) The other features are shown in Table 1. In the follow-up after surgery, none of the patients required reoperation or had complications.
Univariate analysis of the 16 research factors and Ikeuchi grade
Factors such as sex, BMI, work intensity, trauma history, age of onset, symptoms duration, Watanabe type of DLM, combined medial meniscus tear, the site and Outerbridge grade of articular cartilage lesion, K–L grade and surgical method may be associated with Ikeuchi grade (P < 0.05). However, involved side of knee joint, site and O'Connor type of DLM tear, and follow-up time may not be correlated with Ikeuchi grade (P > 0.05) (Table 4).
Multivariate analysis of the 16 research factors and Ikeuchi grade
Female was an adverse factor for obtaining the higher Ikeuchi grade [P = 0.009, odds ratio (OR) 0.45, 95% confidence interval (CI) 0.255–0.822]. Outerbridge grade of articular cartilage lesion (P = 0.018, OR 0.638, 95% CI 0.438–0.927) was negatively correlated with Ikeuchi grade. BMI and work intensity were inversely correlated with Ikeuchi grade (P = 0.001, OR 0.875, 95% CI 0.808–0.948 and P = 0.020, OR 0.611, 95% CI 0.404–0.926, respectively). Age of onset (P < 0.001, OR 0.956, 95% CI 0.933–0.979) and symptoms duration (P < 0.001, OR 0.988, 95% CI 0.983–0.994) were negatively correlated with Ikeuchi grade. Besides, compared to total meniscectomy, meniscoplasty with repair was an unfavourable factor for getting good Ikeuchi grade (P = 0.044, OR 0.245, 95% CI 0.062–0.963). Nevertheless, no significant difference was found between total meniscectomy and meniscoplasty. In addition, K–L grade, history of trauma, Watanabe type of DLM, combined medial meniscus tear and site of articular cartilage lesion did not affect Ikeuchi grade (Table 5).
Discussion
In this study, we found that sex, BMI, work intensity, age of onset, duration of symptoms, the severity of cartilage lesion and surgical mode are correlated with postoperative outcomes of symptomatic DLM, while K–L grade, history of trauma, Watanabe type of DLM, combined medial meniscus tear and site of articular cartilage lesion did not correlate with Ikeuchi grade.
Female is a risk factor for many orthopaedic diseases, but its correlation with postoperative efficacy of symptomatic DLM is unclear. Chen [17], Kose [9] and Higuchi [18] all found that sex exerts no significant effect on the postoperative outcomes by analysing, respectively, 39 patients, 48 patients and 67 patients with DLM. However, Ahn et al. [19], by evaluating 260 DLM patients, believed that sex could affect postoperative outcomes and that male is a protective factor. This study found that sex can influence Ikeuchi grade (P < 0.05) and that female is a risk factor. Studies have shown that the knee articular cartilage volume of women is significantly smaller than that of men and that the female Q angle is greater than that of male, leading to increased patellofemoral joint pressure; thus, women are more prone to suffer cartilage lesions and osteoarthritis than men [8, 20,21,22]. This may be the reason for poor postoperative clinical outcomes in women.
Overweight negatively impacts musculoskeletal health [23]. Fu et al. [8] observed that patients with BMIs > 23.0 kg/m2 are more likely to suffer from articular cartilage lesions than patients with low BMIs. However, Ahn et al. [24] believed that BMI is not a risk factor for radiographic progression of postoperative osteoarthritis of DLM tear. This study found that BMI is negatively correlated with Ikeuchi grade. The higher the BMI, the lower the Ikeuchi grade is. Reportedly, obesity can lead to meniscus compression, and pathological change and loss of articular cartilage, which ultimately results in knee osteoarthritis [25,26,27]. Besides, we detected that work intensity is inversely related to Ikeuchi grade, which may be because knee joint activity, load-bearing capacity and cartilage lesions are positively correlated with work intensity.
Symptoms of DLM can be onset at any age. Younger age of onset may be related to a lower risk of postoperative chondromalacia and a better outcome because of the earlier diagnosis and treatment [7, 28]. Chen [17] and Lee [6] believed that a longer duration of symptoms is associated with a worse efficacy of arthroscopic surgery. Most studies have shown that a longer duration of symptoms, especially > 6 months, may be more prone to make lateral cartilage and residual meniscus injured and degenerated [6,7,8, 24, 29]. This study found that age of onset (P < 0.001, OR 0.956, 95% CI 0.933–0.979) and duration of symptoms (P < 0.001, OR 0.988, 95% CI 0.983–0.994) are negatively correlated with the postoperative outcomes. Therefore, earlier diagnosis and treatment of symptomatic DLM would lead to a better postoperative outcome.
Similar to Kose et al. [9], for postoperative outcomes of DLM patients, we found that Outerbridge grade of the cartilage lesion was negatively correlated with Ikeuchi grade, and that site of the cartilage lesion did not affect Ikeuchi grade. Outerbridge grade can directly reflect the severity of the knee cartilage lesions. Articular cartilage lesions are rarely self-healing. Although the clinical manifestations of an articular cartilage lesion may not be obvious in the short term, most patients will eventually deteriorate to irreversible knee osteoarthritis, thus drastically affecting knee function [30, 31]. In addition, even if K–L grade is associated with the Outerbridge grade, we did not find the significant effect of K–L grade on the postoperative outcome. A higher K–L grade is associated with a more severe cartilage lesion in MRI [32]. However, some studies have found that X-rays are less sensitive in detecting cartilage lesions and articular cartilage loss as early narrowing in joint space is not secondary to articular cartilage thinning but is secondary to meniscal compression [33, 34].
Treating symptomatic DLM by arthroscopic surgery, meniscoplasty is the first choice [3, 24, 28, 35], and meniscoplasty with repair and total meniscectomy are also options. In terms of the postoperative outcomes of these three surgical methods, the opinion is inconsistent. Wong et al. [28] concluded that there was no significant difference in the postoperative outcomes among these three surgical methods. Some studies have found no difference between meniscoplasty and total meniscectomy as to short-term clinical outcomes [36,37,38], but the clinical efficacy of meniscoplasty is better than that of total meniscectomy in the long-term follow-up [3, 24, 38,39,40,41,42]. Other studies have shown that the long-term outcomes of meniscoplasty with or without repair are satisfactory, without statistical difference [9, 38, 39, 41, 43, 44]. Moreover, Perkins et al. [45] founded that, for meniscocapsular tears, meniscoplasty with repair is related to low rates of revision surgery and good intermediate-term outcomes. Geffroy [46] observed that the results of meniscoplasty with repair in children with DLM are very satisfactory in general, whatever the type or site of the lesion. Conversely, Lee et al. [6] believe that residual discoid meniscus tissue is prone to degeneration and re-injury due to abnormally fibrous structure, which may lead to adverse clinical effects. Besides, considering the high cost and uncertain effective of the repair, Smuin et al. [38] do not recommend the repair of the abnormal anatomy in a torn DLM. In the present study, compared with the postoperative efficacy of total meniscectomy, meniscoplasty seems to be no different, but meniscoplasty with repair seems worse (P = 0.044, OR 0.245). This result, however, seems to be inconsistent with the results of statistical description that percentage of “excellent" and "good" in meniscoplasty with repair group is higher than that in total meniscectomy group (87.5% vs 57.9%), which may be attributed to the characteristics of multivariate analysis model and small sample size. Compared with statistical description, the multivariate analysis model can independently reflect the effect of the surgical method on Ikeuchi grade by controlling the influence of other factors. Besides, the small sample size in meniscoplasty with repair and total meniscectomy may reduce the power of the test to some extent. Therefore, the influence of surgical methods on the postoperative efficacy of DLM needs to be further verified by extending the follow-up time, expanding the sample size, and increasing the postoperative imaging evaluation.
So far, there are few studies on the effects of the site of DLM tear on postoperative outcomes. Hede et al. [47] found that when the amount of meniscal tissue removed is less than 30%, the site of the lesion does not affect the postoperative outcome; but more than 30%, the postoperative outcome of tears in anterior and posterior horn is worse than that of meniscal body tears. Moreover, studies have shown that tear type does not affect the postoperative outcome [8, 9, 19]. However, Chen [17] and Badlani [48] considered that radial tears in the discoid meniscus led to poor postoperative outcome. Ahn et al. [26] found that horizontal tears in the discoid meniscus were an important risk factor for the radiological progression of postoperative osteoarthritis with K–L grade 3/4. In our study, the site and O'Connor type of the DLM tear do not affect the postoperative outcomes, which may be because patients with DLM tears often diagnosed and treated early for their clinical symptoms. Besides, consistent with the result of Lee [6] and Kose [9], this study also showed that the Watanabe type of DLM is not an influencing factor for the postoperative outcomes, which probably because the incidence of a cartilage lesion is not correlated with the DLM type [8, 29]. Although a longer follow-up period is believed to be associated with a bad knee function score [6, 40]. our study did not demonstrate that the final follow-up time (75.4, 41 ~ 123 months) is an influencing factor for the postoperative efficacy, which may be due to the small number of patients with follow-up periods over 120 months.
We acknowledge that there are some limitations to our study. First, the postoperative efficacy evaluation in this study did not assess the objective imaging changes at the final follow-up and instead only evaluated the subjective functional parameters. Second, the lost rate of follow-up is 14.2%, which may be a potential source of bias. Third, comparatively small sample size, and multi-categorized factors and Ikeuchi grade result in a few patients in some categories, which may lower the power of the test. Finally, this study is a retrospective multivariate analysis, and the conclusions need to be further confirmed by prospective studies.
Conclusion
With the increase of BMI, work intensity, age of onset, duration of symptoms, and the severity of cartilage lesion, the postoperative results become worse. Moreover, female and meniscoplasty with repair are risk factors for the postoperative outcomes.
Data availability
The patient's personal information and imaging data obtained at following-up were stored on the disc. The data are available from the corresponding author upon request. GC should be contacted with requests for data and materials.
References
Kim JH, Ahn JH, Kim JH, Wang JH (2020) Discoid lateral meniscus: importance, diagnosis, and treatment. J Exp Orthop 7(1):81. https://doi.org/10.1186/s40634-020-00294-y
Yang SJ, Zhang MZ, Li J, Xue Y, Chen G (2020) A reliable, ultrasound-based method for the diagnosis of discoid lateral meniscus. Arthroscopy. https://doi.org/10.1016/j.arthro.2020.09.034
Ng YH, Tan SHS, Lim AKS, Hui JH (2020) Meniscoplasty leads to good mid-term to long-term outcomes for children and adolescents with discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-05929-2
Lee SH (2019) Editorial commentary: why should the contralateral side be examined in patients with symptomatic discoid lateral meniscus? Arthroscopy 35(2):507–510. https://doi.org/10.1016/j.arthro.2018.11.067
Kocher MS, Logan CA, Kramer DE (2017) Discoid lateral meniscus in children: diagnosis, management, and outcomes. J Am Acad Orthop Surg 25(11):736–743. https://doi.org/10.5435/jaaos-d-15-00491
Lee CR, Bin SI, Kim JM, Lee BS, Kim NK (2018) Arthroscopic partial meniscectomy in young patients with symptomatic discoid lateral meniscus: an average 10-year follow-up study. Arch Orthop Trauma Surg 138(3):369–376. https://doi.org/10.1007/s00402-017-2853-1
Persiani P, Mariani M, Crostelli M, Mascello D, Mazza O, Ranaldi FM, Martini L, Villani C (2013) Can early diagnosis and partial meniscectomy improve quality of life in patients with lateral discoid meniscus? Clin Ter 164(5):e359-364. https://doi.org/10.7417/ct.2013.1613
Fu D, Guo L, Yang L, Chen G, Duan X (2014) Discoid lateral meniscus tears and concomitant articular cartilage lesions in the knee. Arthroscopy 30(3):311–318. https://doi.org/10.1016/j.arthro.2013.11.029
Kose O, Celiktas M, Egerci OF, Guler F, Ozyurek S, Sarpel Y (2015) Prognostic factors affecting the outcome of arthroscopic saucerization in discoid lateral meniscus: a retrospective analysis of 48 cases. Musculoskelet Surg 99(2):165–170. https://doi.org/10.1007/s12306-015-0376-x
Yang SJ, Ding ZJ, Li J, Xue Y, Chen G (2020) Factors influencing postoperative outcomes in patients with symptomatic discoid lateral meniscus. BMC Musculoskelet Disord 21 (1):551. https://doi.org/10.1186/s12891-020-03573-y
Habata T, Uematsu K, Kasanami R, Hattori K, Takakura Y, Tohma Y, Fujisawa Y (2006) Long-term clinical and radiographic follow-up of total resection for discoid lateral meniscus. Arthroscopy 22(12):1339–1343. https://doi.org/10.1016/j.arthro.2006.07.039
Kraus TM, Abele C, Freude T, Ateschrang A, Stöckle U, Stuby FM, Schröter S (2018) Duration of incapacity of work after tibial plateau fracture is affected by work intensity. BMC Musculoskelet Disord 19(1):281. https://doi.org/10.1186/s12891-018-2209-1
Patel R, Eltgroth M, Souza R, Zhang CA, Majumdar S, Link TM, Motamedi D (2016) Loaded versus unloaded magnetic resonance imaging (MRI) of the knee: effect on meniscus extrusion in healthy volunteers and patients with osteoarthritis. Eur J Radiol Open 3:100–107. https://doi.org/10.1016/j.ejro.2016.05.002
Kim YG, Ihn JC, Park SK, Kyung HS (2006) An arthroscopic analysis of lateral meniscal variants and a comparison with MRI findings. Knee Surg Sports Traumatol Arthrosc 14(1):20–26. https://doi.org/10.1007/s00167-005-0629-6
Slattery C, Kweon CY (2018) Classifications in brief: outerbridge classification of chondral lesions. Clin Orthop Relat Res 476(10):2101–2104. https://doi.org/10.1007/s11999.0000000000000255
Ikeuchi H (1982) Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res 167:19–28
Chen HC, Yang CB, Tsai CF, Ma HL, Liu CL, Huang TF (2011) Management and outcome of discoid meniscus tears. Formosan J Musculoskelet Disord 2(2):45–48. https://doi.org/10.1016/j.fjmd.2011.03.002
Higuchi H, Kimura M, Shirakura K, Terauchi M, Takagishi K (2000) Factors affecting long-term results after arthroscopic partial meniscectomy. Clin Orthop Relat Res 377:161–168. https://doi.org/10.1097/00003086-200008000-00022
Ahn JY, Kim TH, Jung BS, Ha SH, Lee BS, Chung JW, Kim JM, Bin SI (2012) Clinical results and prognostic factors of arthroscopic surgeries for discoid lateral menisci tear: analysis of 179 cases with minimum 2 years follow-up. Knee Surg Relat Res 24(2):108–112. https://doi.org/10.5792/ksrr.2012.24.2.108
Cicuttini F, Forbes A, Morris K, Darling S, Bailey M, Stuckey S (1999) Gender differences in knee cartilage volume as measured by magnetic resonance imaging. Osteoarthr Cartil 7(3):265–271. https://doi.org/10.1053/joca.1998.0200
Hanna FS, Teichtahl AJ, Wluka AE, Wang Y, Urquhart DM, English DR, Giles GG, Cicuttini FM (2009) Women have increased rates of cartilage loss and progression of cartilage defects at the knee than men: a gender study of adults without clinical knee osteoarthritis. Menopause 16(4):666–670. https://doi.org/10.1097/gme.0b013e318198e30e
Cho HJ, Chang CB, Yoo JH, Kim SJ, Kim TK (2010) Gender differences in the correlation between symptom and radiographic severity in patients with knee osteoarthritis. Clin Orthop Relat Res 468(7):1749–1758. https://doi.org/10.1007/s11999-010-1282-z
Hozumi J, Sumitani M, Matsubayashi Y, Abe H, Oshima Y, Chikuda H, Takeshita K, Yamada Y (2016) Relationship between neuropathic pain and obesity. Pain Res Manag 2016:2487924. https://doi.org/10.1155/2016/2487924
Ahn JH, Kang DM, Choi KJ (2017) Risk factors for radiographic progression of osteoarthritis after partial meniscectomy of discoid lateral meniscus tear. Orthop Traumatol Surg Res 103(8):1183–1188. https://doi.org/10.1016/j.otsr.2017.09.013
Englund M, Felson DT, Guermazi A, Roemer FW, Wang K, Crema MD, Lynch JA, Sharma L, Segal NA, Lewis CE, Nevitt MC (2011) Risk factors for medial meniscal pathology on knee MRI in older US adults: a multicentre prospective cohort study. Ann Rheum Dis 70(10):1733–1739. https://doi.org/10.1136/ard.2011.150052
Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, Guermazi A, Grigorian M, Gale D, Felson DT (2006) The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum 54(3):795–801. https://doi.org/10.1002/art.21724
Sowers MR, Karvonen-Gutierrez CA (2010) The evolving role of obesity in knee osteoarthritis. Curr Opin Rheumatol 22(5):533–537. https://doi.org/10.1097/BOR.0b013e32833b4682
Wong T, Wang CJ (2011) Functional analysis on the treatment of torn discoid lateral meniscus. Knee 18(6):369–372. https://doi.org/10.1016/j.knee.2010.07.002
Ding J, Zhao J, He Y, Huangfu X, Zeng B (2009) Risk factors for articular cartilage lesions in symptomatic discoid lateral meniscus. Arthroscopy 25(12):1423–1426. https://doi.org/10.1016/j.arthro.2009.06.024
Redondo ML, Beer AJ, Yanke AB (2018) Cartilage restoration: microfracture and osteochondral autograft transplantation. J Knee Surg 31(3):231–238. https://doi.org/10.1055/s-0037-1618592
Logerstedt DS, Scalzitti DA, Bennell KL, Hinman RS, Silvers-Granelli H, Ebert J, Hambly K, Carey JL, Snyder-Mackler L, Axe MJ, McDonough CM (2018) Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther 48(2):A1-a50. https://doi.org/10.2519/jospt.2018.0301
Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N, Majumdar S (2003) Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology 226(2):373–381. https://doi.org/10.1148/radiol.2262012190
Amin S, LaValley MP, Guermazi A, Grigoryan M, Hunter DJ, Clancy M, Niu J, Gale DR, Felson DT (2005) The relationship between cartilage loss on magnetic resonance imaging and radiographic progression in men and women with knee osteoarthritis. Arthritis Rheum 52(10):3152–3159. https://doi.org/10.1002/art.21296
Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S (1999) Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol 54(8):502–506. https://doi.org/10.1016/s0009-9260(99)90846-2
Saavedra M, Sepulveda M, Jesus Tuca M, Birrer E (2020) Discoid meniscus: current concepts. EFORT Open Rev 5(7):371–379. https://doi.org/10.1302/2058-5241.5.190023
Zhang P, Zhao Q, Shang X, Wang Y (2018) Effect of arthroscopic resection for discoid lateral meniscus on the axial alignment of the lower limb. Int Orthop 42(8):1897–1903. https://doi.org/10.1007/s00264-018-3944-5
Kim SJ, Chun YM, Jeong JH, Ryu SW, Oh KS, Lubis AM (2007) Effects of arthroscopic meniscectomy on the long-term prognosis for the discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc 15(11):1315–1320. https://doi.org/10.1007/s00167-007-0391-z
Smuin DM, Swenson RD, Dhawan A (2017) Saucerization versus complete resection of a symptomatic discoid lateral meniscus at short- and long-term follow-up: a systematic review. Arthroscopy 33(9):1733–1742. https://doi.org/10.1016/j.arthro.2017.03.028
Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH (2015) Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy 31(5):867–873. https://doi.org/10.1016/j.arthro.2014.12.012
Lee YS, Teo SH, Ahn JH, Lee OS, Lee SH, Lee JH (2017) Systematic review of the long-term surgical outcomes of discoid lateral meniscus. Arthroscopy 33(10):1884–1895. https://doi.org/10.1016/j.arthro.2017.04.006
Hashimoto Y, Nishino K, Reid JB 3rd, Yamasaki S, Takigami J, Tomihara T, Takahashi S, Shimada N, Nakamura H (2020) Factors related to postoperative osteochondritis dissecans of the lateral femoral condyle after meniscal surgery in juvenile patients with a discoid lateral meniscus. J Pediatr Orthop 40(9):e853–e859. https://doi.org/10.1097/bpo.0000000000001636
Lee DH, D’Lima DD, Lee SH (2019) Clinical and radiographic results of partial versus total meniscectomy in patients with symptomatic discoid lateral meniscus: a systematic review and meta-analysis. Orthop Traumatol Surg Res 105(4):669–675. https://doi.org/10.1016/j.otsr.2019.02.023
Ohnishi Y, Nakashima H, Suzuki H, Nakamura E, Sakai A, Uchida S (2018) Arthroscopic treatment for symptomatic lateral discoid meniscus: the effects of different ages, groups and procedures on surgical outcomes. Knee 25(6):1083–1090. https://doi.org/10.1016/j.knee.2018.06.003
Chedal-Bornu B, Morin V, Saragaglia D (2015) Meniscoplasty for lateral discoid meniscus tears: long-term results of 14 cases. Orthop Traumatol Surg Res 101(6):699–702. https://doi.org/10.1016/j.otsr.2015.06.017
Perkins CA, Busch MT, Christino MA, Willimon SC (2021) Saucerization and repair of discoid lateral menisci with peripheral rim instability: intermediate-term outcomes in children and adolescents. J Pediatr Orthop 41(1):23–27. https://doi.org/10.1097/bpo.0000000000001695
Geffroy L (2020) Meniscal pathology in children and adolescents. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2020.102775
Hede A, Larsen E, Sandberg H (1992) The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop 16(2):122–125. https://doi.org/10.1007/bf00180200
Stilli S, Marchesini Reggiani L, Marcheggiani Muccioli GM, Cappella M, Donzelli O (2011) Arthroscopic treatment for symptomatic discoid lateral meniscus during childhood. Knee Surg Sports Traumatol Arthrosc 19(8):1337–1342. https://doi.org/10.1007/s00167-011-1440-1
Acknowledgements
The authors gratefully acknowledge the patient shown in the article.
Funding
This work was supported by Sichuan Provincial Department of Science and Technology Project (No. 2017SZ0017, No. 2018FZ0040).
Author information
Authors and Affiliations
Contributions
SJY participated in the surgery, collected clinical data, and made major contributions to the writing and editing of the manuscript. JL performed surgery and was responsible for the screening of the patients and for postoperative follow-up. YX and ZZ initiated the work and collected clinical data. GC participated in the entire process, including surgery, follow-up of the patients, data collection, and writing and revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest for with respect to the research, authorship and/or publication of this article.
Ethical approval
This study was approved by the Local Ethical Committee [2016(226)], and it was performed byin accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2000. The patients received a thorough explanation of this study and gave their written informed consent to be included in this analysis.
Informed consent
The patients gave their written informed consent to the publication of their anonymous and clustered data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, SJ., Li, J., Xue, Y. et al. Multivariate ordered logistic regression analysis of the postoperative effect of symptomatic discoid lateral meniscus. Arch Orthop Trauma Surg 141, 1935–1944 (2021). https://doi.org/10.1007/s00402-021-03821-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03821-3