Abstract
Purpose
This study's goal is to propose a straightforward classification system based on the MEI (Meniscal Extrusion Index), a measure of meniscal extrusion, that relates to various meniscal lesion patterns and has clinical and biomechanical significance. The study's secondary goal is to determine whether the standard 3 mm meniscal extrusion parameter still has value by correlating the MEI with it.
Methods
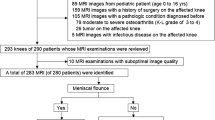
1350 knee MRIs that were performed over the course of 2 years made up the study cohort. Following the application of inclusion and exclusion criteria, 200 of those patients were qualified to participate in the study. All the measurements examined for this study underwent an interobserver reliability test.
Results
In the 1350 MRIs that were examined for this study, meniscal extrusion of any grade was present 18.9% of the time. The use of the MEI revealed three groups of patients: those with a MEI < 20%, who are likely para-physiological; those with a MEY between 20% and 40%, who are in a grey area; and those with a MEY > 40%, who have lesions that are impairing the proper meniscal function. According to the authors' findings, the percentage of meniscal extrusion did not correlate with the finite number (3 mm), making the 3 mm parameter an unreliable evaluation method.
Conclusions
This study is clinically relevant, because it proposes a simple and reproducible classification of meniscal extrusion that may aid in evaluating the severity of an extrusion and help in the diagnosis of lesions that might be difficult to identify on MRI.
Level of evidence
Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal extrusions (ME) refer to the complete or partial displacement of the meniscus beyond the tibial plateau and the tibial articular cartilage [15]. The biomechanical forces exerted on the knee during weight-bearing primarily impact the medial meniscus, resulting in extrusion forces or circumferential hoop stresses [12, 24]. Several anatomical structures play a crucial role in facilitating efficient medial meniscal function and preventing its extrusion [10, 21]. The most relevant structures are the meniscal roots, inter-meniscal ligaments, medial collateral ligament, and coronary ligament, which attaches to the medial side of the tibial plateau periphery [1, 25].
Meniscal posterior root tears (MPRT) and radial tears can result in the detachment of the meniscus from the tibial plateau, as well as the disruption of the circumferential fibers. These conditions compromise normal meniscus function and can lead to meniscal extrusion [6, 14].
The loss of functional capacity in an extruded meniscus can contribute to the progressive deterioration of osteoarthritis and the development of bone edema syndrome over time [2, 3, 13].
Degenerative meniscus lesions (DMLs) and complex tears, common in the over 50-year-old population, entail the degradation of collagen fibers in the meniscus. These conditions arise as a result of a complex interplay involving excessive use, mechanical overload, and impaired biological repair mechanisms [20].
Meniscal extrusions are evaluated with magnetic resonance imaging (MRI) and many categorizations have been proposed [22]; however, the most used classification distinguishes lesions as major (> 3 mm) and minor (< 3 mm) [4]. In addition, instead of a single value, other authors use in this study ranges of meniscal extrusion rates. Crema et al. classified medial and lateral meniscal extrusion as follows: no extrusion (grade 0), extrusion of 50% of the body (grade 1), and extrusion of > 50% of the body (grade 2) [5].
Miller et al. utilized a cutoff value of 25%, since this was the smallest amount they could confidently discern. They concluded that meniscal extrusion exceeding 25% of meniscal width was not significantly associated with a meniscal tear [19].
The aim of this study is to determine whether a percentage of meniscal extrusion, known as the Meniscal Extrusion Index (MEI), correlates with a specific pattern of meniscal lesion. This study introduces the MEI as a novel parameter that can aid clinicians in accurately assessing the degree of meniscal extrusion and help diagnose lesions that may not be easily identifiable on MRI.
The hypothesis of this study is that there is a correlation between the MEI and the severity of the underlying meniscal lesion.
Materials and methods
The study was performed at Istituto Ortopedico Gaetano Pini and approved by the local ethical committee (authorization number: Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico–Milano Area 2, Lombardia, Milan (n°394_2019bis, Milan, 08.05.2019). The study was conducted in two distinct phases. The first phase was a literature review in March 2023 using the Pubmed/Medline and Cochrane databases. The objective was to identify all existing classifications of meniscal extrusion that had been described in the literature. In the second phase, a retrospective evaluation was carried out using imaging data obtained at the study hospital. The evaluations were performed using the same 1.5 Tesla MRI machine and study protocol. The exclusion criteria for this study were age under 18 or sign of incomplete growth, signs of previous surgery, malignancies or local expanding lesions or fractures. All knee MRI performed between July 2021 and June 2022 were analyzed and only those eligible for the study were included.
The MRI images were evaluated by two different researchers who assessed the inclusion and exclusion criteria. In case of any doubts or uncertainties, a third, more experienced researcher was involved in the decision-making process. PD, STIR and T2 Fat-Sat sequences were analyzed on the coronal plane. The level considered was the plane that presented the biggest with of the tibial spines as described by Costa et al. [4].
A meniscal extrusion (ME) was defined as any overhanging of the medial meniscal body over the tibial plateau on the analyzed plane. Osteophytes were not considered in this evaluation as that could alter the real tibial plateau width. The total medial meniscal width and the overhanging portion of the meniscus were measured, as described in Fig. 1.
The Meniscal Extrusion Index (MEI) was calculated by determining the ratio between the extruded portion of the meniscus and the total width of the meniscus. In the same imaging plane, the width of the medial tibial plateau and the width of the medial femoral condyle were also measured.
The medial tibial plateau width was measured from the apex of the medial tibial spine parallel the tibial plateau up to the perpendicular to the medial tibial border, as shown in Fig. 2.
The medial femoral condyle width was performed in the same fashion between the lateral border of the medial condyle and the medial cortical bone. The level of the measured was selected as the end of the condyle curvature on the lateral side of the medial condyle.
The program used for the measurement was Xero Viewer, which allowed for the use of one decimal. The authors tried a different program that did not have this feature, but the results were unreliable due to the excessive approximation of the measurements.
The measurements of the meniscus, extrusion, tibial plate, and femoral condyle were recorded with one decimal place accuracy. For all other data, calculations were rounded to one decimal place.
Based on reports in the literature, all associated meniscal lesions were gathered and subdivided into four categories: lesions leading to extrusion, lesions that can lead to extrusion, lesions not leading to extrusion, and no lesions at all.
All evaluations were performed by two independent researchers and the interobserver reliability was then tested.
The inter-observer reliability and ICC analysis was interpreted according to Landis and Koch [17].
Statistical analysis
Data were reported as median and interquartile range (IQR) when quantitative, and as counts and percentages when qualitative. Differences between quantitative data distributions were evaluated with the Wilcoxon test.
For both medial meniscal width, extruded meniscus, medial tibial plateau, and medial femoral condyle width inter-reader reproducibility were appraised via Bland–Altman analyses and reported as bias and coefficient of repeatability (CoR). Statistical analyses were conducted using Python 3.7.6, and p values < 0.05 were chosen as a threshold for statistical significance.
The sample size was calculated setting a significance level (threshold for α, or type 1, error) of 5% or 0.05, a desired power (1-β) of 80%, and estimating an effect size (d) of (M1–M2)/SD as per Cohen’s d, and a standard deviation of 0.05. As such, the d estimate would be 0.60, and according to the formula n = (Z * (sqrt(n1 + n2 + 1) + sqrt(n1)))2/(d2), the required sample size would have been 120 patients. All knee MRI performed between July 2021 and June 2022 were retrospectively retrieved.
Results
A total of 1350 patients were eligible for MRI examinations, from 07/13/2021 to 05/30/2022. Meniscal extrusion was identified in 255 patients. A prevalence of 18.9% was, therefore, found in the population examined. After application of exclusions criteria, 55 exams were excluded from this study due to the presence of fractures, signs of previous surgery, tumors, low quality images or because the patients were under the age of 18. Two hundred medial meniscal extrusions were found to match the inclusion criteria.
Demographic data of the group of patients who received MRI assessment are reported in Table 1.
For each MRI was calculated the meniscal width (mm), the meniscal extrusion width (mm), the medial tibial plateau width (mm), and the medial femoral condyle width (mm). Results are reported in Table 2.
The variability of the meniscus’s width was 11.1 ± 2.6 Mean ± SD; 10.8 [12.4–9.4] Median [Q1–Q3].
Considering the meniscal extrusions of 3 ± 0.2 mm, their distribution was compared with the respective extrusion in % (MEI), as shown in Fig. 3.
All the MRI were categorized, based on the meniscal injury, in 4 groups: tears leading to extrusion (including Root lesions and radial tears), tears that might result in extrusion (complex tears and meniscal degeneration), tears not leading to extrusion (horizontal and longitudinal tears), no injuries (when no meniscal tear was found). The extrusion index was calculated for each group; the results are reported in Table 3.
In particular, the distribution of groups “tears leading to extrusion” and “no injuries” was reported and compared in Fig. 4.
Inter-observer reliability found an ICC of 0.996 which translate to an “almost perfect agreement”.
Discussion
The most important finding of the present study was that the Meniscal Extrusion Index (MEI)-based classification of medial meniscal extrusion in the study showed a correlation with the severity of the underlying lesion. This classification system is simple, reproducible, and useful in clinical settings.
Abnormal medial meniscus extrusion is defined as protrusion of the body of the medial meniscus beyond the tibial plateau [15]. In literature the presence of a meniscal lesion is often associated with meniscal extrusion [7, 8, 23].
Due to the anatomy of the medial meniscus, various lesions are described as more or less responsible for meniscal extrusion [9, 11, 18].
Based on the available literature, the authors identified four distinct categories for meniscal lesions. The first group encompasses lesions that result in extrusion, such as root lesions and radial lesions. The second group consists of lesions that have the potential to cause extrusion, including complex tears and degenerative meniscal lesions. Group 3 comprises all lesions that do not lead to extrusion, such as horizontal and longitudinal tears. Finally, group 4 comprises patients without any meniscal lesions.
This study mainly focused on two groups: meniscal extrusions without any type of associated meniscal tear (group 4) and extrusions associated with lesions typically lead to extrusion (group 1).
The distribution of the two groups is illustrated in graph 2. Based on those data is evident that there are two very clear groups: patients with a MEI under 20% and patients with MEI over 40%.
In the first sub-group of patients, those with a MEI < 20%, there were no case of lesion known to be responsible for extrusion.
In the second sub-group (MEI > 40%) all patients presented an underlying lesion leading to extrusion.
Based on these data, a new classification of meniscal extrusions could be proposed, based on the MEI parameter:
-
MEI smaller than 20%: slightly extruded, no underlying meniscal lesion causing functional insufficiency of the meniscus, probably para-physiological imaging feature.
-
MEI between 20% and 40%: moderate extrusion, a gray area, high suspicion of an underlying lesion, unclear functional impairment.
-
MEI higher than 40%: severely extruded menisci, always related to an underlying lesion that impairs the mechanical function of the meniscus.
The secondary outcome of this study was to evaluate if the standard 3 mm cut off proposed by Costa et al. was still viable. In their study, Costa et al. classified the degree of meniscal extrusion observed on imaging as major (> 3 mm) and minor (< 3 mm) [4].
In their research, they concluded that medial meniscus extrusion greater than 3 mm is significantly associated with extent of meniscal degeneration, extent of tear, complex tear, large radial tear, and tear involving the meniscal root.
In this study the authors analyze the measurement in mm of meniscal width, meniscal extrusion width, medial tibial plateau width, medial femoral condyle width. Results show that there is an individual variability of each parameter.
The authors found that there was no relationship between the finite number and the percentage of extrusion. The menisci extruded 3 ± 0.2 mm corresponded in the series analyzed to an extremely variable percentage of extrusion ranging from 52.8% to 16.5%.
The variability of the meniscus’s width found in this study makes the cutoff calculated in mm a limit.
For this reason, it would be more reliable to identify the extrusion as a percentage, expressed as mm of extruded meniscus compared to the total width of the meniscus.
Inter-observer reliability analysis performed confirms how this methodology is reproducible and how the MEI is easily calculated.
This study has some limitations, first being based on a retrospective sample.
The study group had a mean age of 54.8 years, so extrapolated data might not apply to a population that is young and athletic.
Moreover, while it can be assumed that all patients included in the MRI scans were experiencing symptoms, such as knee pain, the authors did not establish a correlation between the imaging findings and the patients' medical history or reported symptoms.
Basing data on MRI images, without arthroscopic confirmation, may be a limitation, although knee MRI has a documented high accuracy for diagnosis of medial meniscal tear, with sensitivities of 91.8% and specificities of 80.8% [9, 16].
The authors did not investigate additional extra-articular causes of meniscal extrusion mentioned in the literature. Factors such as knee misalignment, female sex, and high BMI were not considered in this study, as they are more likely to lead to intra-articular damage to the meniscus rather than being direct causes of extrusion.
Indeed, this study holds clinical relevance as it proposes a simple and reproducible classification system for meniscal extrusion. This classification can be valuable in assessing the severity of an extrusion and aiding in the diagnosis of lesions that may not be easily identifiable. By providing clinicians with a practical tool, this study contributes to improving the evaluation and understanding of meniscal extrusion in clinical practice.
Conclusion
The study's classification of medial meniscal extrusion, based on the Meniscal Extrusion Index (MEI), demonstrates a correlation with the severity of the underlying lesion. This classification system is considered simple, reproducible, and applicable in clinical settings.
The study also highlights the potential for incorrect interpretation of the significance of meniscal extrusion when relying solely on the measurement in millimeters (mm). It demonstrates that the entity of meniscal extrusion can be over or underestimated using this approach.
Data availability
In accordance with the Italian d.lgs. 101/2018, data supporting Tables 1–3 and Figures 1–4 are not publicly available to preserve patient privacy. These datasets are available upon request from the corresponding author.
References
Banovetz MT, Roethke LC, Rodriguez AN, LaPrade RF (2022) Meniscal root tears: a decade of research on their relevant anatomy, biomechanics, diagnosis, and treatment. Arch Bone Joint Surg 10(5):366–380
Compagnoni R, Lesman J, Ferrua P, Menon A, Minoli C, Gallazzi M, Domżalski M, Randelli P (2021) Validation of a new topographic classification of bone marrow lesions in the knee: the six-letter system. Knee Surg Sports Traumatol Arthrosc 29(2):333–341
Compagnoni R, Lesman J, Minoli C, Ferrua P, Trissino M, da Lodi C, Domżalski M, Menon A, Randelli PS (2023) Bone marrow lesions in the knee are associated with meniscal lesions and cartilage pathologies according to the six-letter system. Knee Surg Sports Traumatol Arthrosc 31(1):286–291. https://doi.org/10.1007/s00167-022-07089-x
Costa CR, Morrison WB, Carrino JA (2012) Medial Meniscus Extrusion on Knee MRI: Is Extent Associated with Severity of Degeneration or Type of Tear? Surg Sport 183(1):17–23
Crema MD, Roemer FW, Felson DT, Englund M, Wang K, Jarraya M, Nevitt MC, Marra MD, Torner JC, Lewis CE, Guermazi A (2012) Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the Multicenter Osteoarthritis study. Radiology 264(2):494–503
Eseonu KC, Neale J, Lyons A, Kluzek S (2022) Are outcomes of acute meniscus root tear repair better than debridement or nonoperative management? a systematic review. Am J Sports Med 50(11):3130–3139
Falkowski AL, Jacobson JA, Cresswell M, Bedi A, Kalia V, Zhang B (2022) Medial meniscal extrusion evaluation with weight-bearing ultrasound: correlation with MR imaging findings and reported symptoms: correlation with MR imaging findings and reported symptoms. J Ultrasound Med 41(11):2867–2875
Farivar D, Hevesi M, Fortier LM, Azua E, LaPrade RF, Chahla J (2022) Meniscal extrusion measurements after posterior medial meniscus root tears: a systematic review and meta-analysis. Am J Sports Med. https://doi.org/10.1177/03635465221131005
Fong FJY, Ong BWL, Lee YHD (2023) Medial meniscal extrusion in patients with medial meniscus root tears: a systematic review and meta-analysis. Orthop J Sports Med 11(3):232596712311516
Foreman SC, Liu Y, Nevitt MC, Neumann J, Joseph GB, Lane NE, McCulloch CE, Link TM (2021) Meniscal root tears and extrusion are significantly associated with the development of accelerated knee osteoarthritis: data from the osteoarthritis initiative. Cartilage 13(1 Suppl):239S https://doi.org/10.1177/1947603520934525
Gajjar SM, Solanki KP, Shanmugasundaram S, Kambhampati SBS (2021) Meniscal extrusion: a narrative review. Orthop J Sports Med. https://doi.org/10.1177/23259671211043797
Gee SM, Posner M (2021) Meniscus anatomy and basic science. Sports Med Arthrosc Rev 29(3):E18–E23
Ghouri A, Muzumdar S, Barr AJ, Robinson E, Murdoch C, Kingsbury SR, Conaghan PG (2022) The relationship between meniscal pathologies, cartilage loss, joint replacement and pain in knee osteoarthritis: a systematic review. Osteoarthritis Cartilage 30(10):1287–1327
Hirose T, Mae T, Ogasawara I, Yamakawa S, Nakata K, Ohori T, Tsujii A, Okada S (2022) Meniscal displacement and loss of load-transmission function after radial tear of the lateral meniscus in a porcine model: new insights into the functional dynamics of the injured meniscus. Am J Sports Med 50(7):1850–1857
Kaiser JT, Damodar D, Udine MJ, Meeker ZD, McCormick JR, Wagner KR, Krych AJ, Chahla JA, Cole BJ (2022) Meniscal extrusion: a critical analysis review. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.22.00019
Kim SH, Lee HJ, Jang YH, Chun KJ, Park YB (2021) Diagnostic accuracy of magnetic resonance imaging in the detection of type and location of meniscus tears: comparison with arthroscopic findings. J Clin Med 10(4):606 https://doi.org/10.3390/jcm10040606
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159 https://doi.org/10.2307/2529310
Makiev KG, Vasios IS, Georgoulas P, Tilkeridis K, Drosos G, Ververidis A (2022) Clinical significance and management of meniscal extrusion in different knee pathologies: a comprehensive review of the literature and treatment algorithm. Knee Surg Relat Res. https://doi.org/10.1186/S43019-022-00163-1
Miller TT, Staron RB, Feldman F, Çepel E (1997) Meniscal position on routine MR imaging of the knee. Skeletal Radiol 26(7):424–427
Ozeki N, Koga H, Sekiya I (2022) Degenerative meniscus in knee osteoarthritis: from pathology to treatment. Life (Basel). https://doi.org/10.3390/LIFE12040603
Randazzo E, Duerr R, Baria MR (2022) Meniscus root tears: a clinical review. Curr Sports Med Rep 21(5):155–158
Stensby JD, Pringle LC, Crim J (2021) MRI of the Meniscus. Clin Sports Med 40(4):641–655
Sundararajan SR, Ramakanth R, Sethuraman AS, Kannan M, Rajasekaran S (2022) Correlation of factors affecting correction of meniscal extrusion and outcome after medial meniscus root repair. Arch Orthop Trauma Surg 142(5):823–834
van der Voet JA, Schiphof D, Vroegindeweij D, Oei EH, Bierma-Zeinstra SMA, Runhaar J (2023) Association between baseline meniscal extrusion and long-term incident knee osteoarthritis in two different cohorts. Semin Arthritis Rheum 59:152170 https://doi.org/10.1016/j.semarthrit.2023.152170
Yoon SJ, Ahn JM, Kang Y, Kim BR, Kang HS (2022) Morphological changes in the superficial medial collateral ligament on knee MR imaging: association with medial meniscal extrusion and posterior root medial meniscus abnormality. Skeletal Radiol 51(7):1399–1405
Acknowledgements
No Acknowledgements.
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. There were no funding.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the article.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflict of interest.
Ethical approval
Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico—Milano Area 2, Lombardia, Milan (n°394_2019bis, Milan, 08.05.2019).
Informed consent
All data used for this study were obtained under informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Compagnoni, R., Ferrua, P., Minoli, C. et al. The meniscal extrusion index is a reliable indirect sign of different meniscal lesion patterns: a classification based on percentage of meniscal extrusion. Knee Surg Sports Traumatol Arthrosc 31, 5005–5011 (2023). https://doi.org/10.1007/s00167-023-07525-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07525-6