Abstract
Purpose
Variations in femoral and tibial bony morphology have been associated with higher clinical grading and increased quantitative tibial translation, but not tibial acceleration, during the pivot shift test following anterior cruciate ligament (ACL) injury. The purpose of this study was to determine the impact of femoral and tibial bony morphology, including a measurement influenced by both parameters (the Lateral Tibiofemoral Articular Distance (LTAD)), on the degree of quantitative tibial acceleration during the pivot shift test and rates of future ACL injury.
Methods
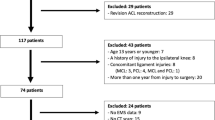
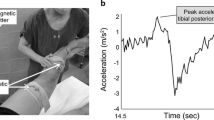
All patients who underwent primary ACL reconstruction from 2014 to 2019 by a senior orthopedic surgeon with available quantitative tibial acceleration data were retrospectively reviewed. All patients underwent a pivot shift examination under anesthesia with a triaxial accelerometer. Measurements of femoral and tibial bony morphology were performed by two fellowship-trained orthopedic surgeons using preoperative magnetic resonance imaging and lateral radiographs.
Results
Fifty-one patients were included at a mean follow-up of 4.4 years. The mean quantitative tibial acceleration during the pivot shift was 13.8 m/s2 (range: 4.9–52.0 m/s2). A larger Posterior Condylar Offset Ratio (r = 0.30, p = 0.045), smaller medial-to-lateral width of the medial tibial plateau (r = − 0.29, p = 0.041), lateral tibial plateau (r = − 0.28, p = 0.042), and lateral femoral condyle (r = − 0.29, p = 0.037), and a decreased LTAD (r = − 0.53, p < 0.001) significantly correlated with increased tibial acceleration during the pivot shift. Linear regression analysis demonstrated an increase in tibial acceleration of 1.24 m/s2 for every 1 mm decrease in LTAD. Nine patients (17.6%) sustained ipsilateral graft rupture and 10 patients (19.6%) sustained contralateral ACL rupture. No morphologic measurements were associated with rates of future ACL injury.
Conclusion
Increased convexity and smaller bony morphology of the lateral femur and tibia were significantly associated with increased tibial acceleration during the pivot shift. Additionally, a measurement, termed the LTAD, was found to have the strongest association with increased tibial acceleration. Based on the results of this study, surgeons can utilize these measurements to preoperatively identify patients at risk of increased rotatory knee instability.
Level of evidence
Level IV.




Similar content being viewed by others
References
Ahlden M, Araujo P, Hoshino Y, Samuelsson K, Middleton KK, Nagamune K et al (2012) Clinical grading of the pivot shift test correlates best with tibial acceleration. Knee Surg Sports Traumatol Arthrosc 20:708–712
Batty LM, Firth A, Moatshe G, Bryant DM, Heard M, McCormack RG et al (2021) Association of ligamentous laxity, male sex, chronicity, meniscal injury, and posterior tibial slope with a high-grade preoperative pivot shift: a post hoc analysis of the stability study. Orthop J Sports Med 9:23259671211000040
Bernholt DL, Dornan GJ, DePhillipo NN (2020) High-grade posterolateral tibial plateau impaction fractures in the setting of a primary anterior cruciate ligament tear are correlated with an increased preoperative pivot shift and inferior postoperative outcomes after anterior cruciate ligament reconstruction. Am J Sports Med 48:2185–2194
Caracciolo G, Yanez R, Silvestre R, De la Fuente C, Zamorano H, Ossio A et al (2021) Intraoperative pivot-shift accelerometry combined with anesthesia improves the measure of rotatory knee instability in anterior cruciate ligament injury. J Exp Orthop 8:80. https://doi.org/10.1186/s40634-021-00396-1
Firth AD, Bryant DM, Litchfield R, McCormack RG, Heard M, MacDonald PB et al (2022) Predictors of graft failure in young active patients undergoing hamstring autograft anterior cruciate ligament reconstruction with or without a lateral extra-articular tenodesis: the stability experience. Am J Sports Med 50:384–395
Friden T, Jonsson A, Erlandsson T, Jonsson K, Lindstrand A (1993) Effect of femoral condyle configuration on disability after an anterior cruciate ligament rupture. 100 patients followed for 5 years. Acta Orthop Scand 64:571–574
Gracia G, Cavaignac M, Marot V, Mouarbes D, Laumonerie PCavaignac E, (2022) Epidemiology of combined injuries of the secondary stabilizers in acl-deficient knees: medial meniscal ramp lesion, lateral meniscus root tear, and all tear: a prospective case series of 602 patients with acl tears from the santi study group. Am J Sports Med 50:1843–1849
Hodel S, Kabelitz M, Tondelli T, Vlachopoulos L, Sutter R, Fucentese SF (2019) Introducing the lateral femoral condyle index as a risk factor for anterior cruciate ligament injury. Am J Sports Med 47:2420–2426
Horvath A, Meredith SJ, Nishida K, Hoshino Y, Musahl V (2020) Objectifying the pivot shift test. Sports Med Arthrosc Rev 28:36–40
Hoshino Y, Araujo P, Ahlden M, Moore CG, Kuroda R, Zaffagnini S et al (2012) Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc 20:732–736
Hoshino Y, Araujo P, Ahlden M, Samuelsson K, Muller B, Hofbauer M et al (2013) Quantitative evaluation of the pivot shift by image analysis using the iPad. Knee Surg Sports Traumatol Arthrosc 21:975–980
Hoshino Y, Miyaji N, Nishida K, Nishizawa Y, Araki D, Kanzaki N et al (2019) The concomitant lateral meniscus injury increased the pivot shift in the anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc 27:646–651
Kawanishi Y, Nozaki M, Kobayashi M, Yasuma S, Fukushima H, Murase A et al (2020) Preoperative knee instability affects residual instability as evaluated by quantitative pivot-shift measurements during double-bundle acl reconstruction. Orthop J Sports Med 8:2325967120959020
Lopomo N, Zaffagnini S, Signorelli C, Bignozzi S, Giordano G, Marcheggiani Muccioli GM et al (2012) An original clinical methodology for non-invasive assessment of pivot-shift test. Comput Methods Biomech Biomed Engin 15:1323–1328
Menzdorf L, Drenck T, Akoto R, Hartel M, Krause M, Guttowski D et al (2020) Clinical results after surgical treatment of posterolateral tibial plateau fractures (“apple bite fracture”) in combination with ACL injuries. Eur J Trauma Emerg Surg 46:1239–1248
Micicoi G, Jacquet C, Khakha R, LiArno S, Faizan A, Seil R et al (2021) Femoral and tibial bony risk factors for anterior cruciate ligament injuries are present in more than 50% of healthy individuals. Am J Sports Med 49:3816–3824
Musahl V, Ayeni OR, Citak M, Irrgang JJ, Pearle AD, Wickiewicz TL (2010) The influence of bony morphology on the magnitude of the pivot shift. Knee Surg Sports Traumatol Arthrosc 18:1232–1238
Musahl V, Griffith C, Irrgang JJ, Hoshino Y, Kuroda R, Lopomo N et al (2016) Validation of quantitative measures of rotatory knee laxity. Am J Sports Med 44:2393–2398
Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y et al (2016) The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med 44:3126–3131
Noyes FR, Grood ES, Cummings JF, Wroble RR (1991) An analysis of the pivot shift phenomenon. the knee motions and subluxations induced by different examiners. Am J Sports Med 19:148–155
Panciera A, Digennaro V, Bogucki BDB, Barile F, Manzetti M, Ferri R et al (2022) The role of posterior condylar offset ratio on clinical and functional outcome of posterior stabilized total knee arthroplasty: a retrospective cohort study. Eur J Orthop Surg Traumatol 11:4435
Pfeiffer TR, Burnham JM, Hughes JD, Kanakamedala AC, Herbst E, Popchak A et al (2018) An increased lateral femoral condyle ratio is a risk factor for anterior cruciate ligament injury. J Bone Joint Surg Am 100:857–864
Pfeiffer TR, Burnham JM, Kanakamedala AC, Hughes JD, Zlotnicki J, Popchak A et al (2019) Distal femur morphology affects rotatory knee instability in patients with anterior cruciate ligament ruptures. Knee Surg Sports Traumatol Arthrosc 27:1514–1519
Polamalu SK, Musahl V, Debski RE (2022) Tibiofemoral bony morphology features associated with ACL injury and sex utilizing three-dimensional statistical shape modeling. J Orthop Res 40:87–94
Song GY, Hong L, Zhang H (2016) Clinical outcomes of combined lateral extra-articular tenodesis and intra-articular anterior cruciate ligament reconstruction in addressing high-grade pivot-shift phenomenon. Arthroscopy 32:898–905
Vaidya RK, Yoo CW, Lee J, Han HS, Lee MC, Ro DH (2020) Quantitative assessment of the pivot shift test with smartphone accelerometer. Knee Surg Sports Traumatol Arthrosc 28:2494–2501
van Diek FM, Wolf MR, Murawski CD, van Eck CF, Fu FH (2014) Knee morphology and risk factors for developing an anterior cruciate ligament rupture: an MRI comparison between ACL-ruptured and non-injured knees. Knee Surg Sports Traumatol Arthrosc 22:987–994
van Kuijk KSR, Reijman M, Bierma-Zeinstra SMA, Meuffels DE (2023) Smaller intercondylar notch size and smaller ACL volume increase posterior cruciate ligament rupture risk. Knee Surg Sports Traumatol Arthrosc 31:449–454
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No Disclosure: Sahil Dadoo, B.S., Emre Anil Ozbek, M.D., Koji Nukuto, M.D., Ph.D., Armin Runer, M.D., Laura E. Keeling, M.D., Camila Grandberg, M.D., Ryosuke Kuroda, M.D., Ph.D., Stefano Zaffagnini, M.D., Jonathan D. Hughes, M.D. JK is editor-in-chief of Knee Surgery, Sports Traumatology, Arthroscopy (KSSTA). JJI will become President-Elect of the Board of Directors for the Journal of Orthopaedic and Sports Physical Therapy on 27 February 2023. VM reports educational grants, consulting fees and speaking fees from Smith & Nephew plc, educational grants from Arthrex and DePuy/Synthes, is a board member of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS), and deputy editor-in-chief of Knee Surgery, Sports Traumatology, Arthroscopy (KSSTA).
Ethical approval
Ethical approval for this study was granted by the Institutional Review Board of the home institution (No: STUDY19030196).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dadoo, S., Ozbek, E.A., Nukuto, K. et al. What it takes to have a high-grade pivot shift—focus on bony morphology. Knee Surg Sports Traumatol Arthrosc 31, 4080–4089 (2023). https://doi.org/10.1007/s00167-023-07472-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07472-2