Abstract
Purpose
This study aimed to identify the risk factors for meniscal repair failure following concurrent primary anterior cruciate ligament (ACL) reconstruction.
Methods
Prospective data recorded by the New Zealand ACL Registry and the Accident Compensation Corporation were reviewed. Meniscal repairs performed during concurrent primary ACL reconstruction were included. Repair failure was defined as a subsequent reoperation involving meniscectomy of the repaired meniscus. Multivariate survival analysis was performed to identify the risk factors for failure.
Results
A total of 3,024 meniscal repairs were analysed with an overall failure rate of 6.6% (n = 201) at a mean follow-up of 2.9 years (SD 1.5). The risk of medial meniscal repair failure was higher with hamstring tendon autografts (adjusted HR [aHR] = 2.20, 95% CI 1.36–3.56, p = 0.001), patients aged 21–30 years (aHR = 1.60, 95% CI 1.30–2.48, p = 0.037) and in patients with cartilage injury in the medial compartment (aHR = 1.75, 95% CI 1.23–2.48, p = 0.002). The risk of lateral meniscal repair failure was higher in patients aged ≤ 20 years (aHR = 2.79, 95% CI 1.17–6.67, p = 0.021), when the procedure was performed by a low case volume surgeon (aHR = 1.84, 95% CI 1.08–3.13, p = 0.026) and when a transtibial technique was used to drill the femoral graft tunnel (aHR = 2.30, 95% CI 1.03–5.15, p = 0.042).
Conclusion
The use of a hamstring tendon autograft, younger age and the presence of medial compartment cartilage injury are risk factors for medial meniscal repair failure, whereas younger age, low surgeon volume and a transtibial drilling technique are risk factors for lateral meniscal repair failure.
Level of evidence
Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rupture of the anterior cruciate ligament (ACL) is a devastating injury for athletes and is often accompanied by injury to the menisci in up to 80% of patients [2, 9, 17, 27, 30, 33, 36, 41]. When reconstructing the ACL, meniscal injuries may be managed by resection, repair or no treatment, depending on the location, stability and extent of injury. Success rates of meniscal repair vary considerably, with up to 44% of patients undergoing subsequent meniscectomy for reasons including a nonhealing repair or new trauma [13, 15, 22, 29, 32, 34]. To reduce the risk of subsequent failure of meniscal repair, it is important to establish the rates of failure, as well as the patient and surgical factors that increase the risk of failure.
Studies from national ACL reconstruction registries have risen in prominence due to the availability of large patient populations and the ability to provide direct feedback to surgeons [6]. In addition to ACL reconstruction data, the New Zealand ACL Registry collects data on the presence of meniscal injury at the time of surgery and the type of meniscal treatment undertaken [24]. Following surgery, patient outcomes are collected by the New Zealand ACL Registry and cross-referenced with the Accident Compensation Corporation (ACC) claims data. The ACC is the Government funder of nearly all ACL reconstructions performed in New Zealand, as well as any related subsequent reoperations [37]. This allows for accurate capture of any patient undergoing subsequent meniscectomy following a meniscal repair in concurrent ACL reconstruction.
This study aimed to combine data recorded from the New Zealand ACL Registry with the ACC reoperations dataset to identify the rate and risk factors for meniscal repair failure following concurrent primary ACL reconstruction. It was hypothesised that medial repairs would have a higher failure rate when compared to lateral repairs with different patient and surgical factors influencing the risk of meniscal repair failure. The results of this study will provide feedback to surgeons of any techniques that may increase meniscal repair failure during concurrent ACL reconstruction and may inform patients of their risk of requiring further surgery.
Materials and methods
This study and collaboration was approved by the ACC Research Ethics Committee. All patients recorded in the registry have signed consent forms for their data to be used and shared between the New Zealand ACL Registry and ACC for the purpose of research. Lastly, the operation of the registry has been declared as a protected quality assurance activity by the New Zealand Government’s Ministry of Health.
The New Zealand ACL Registry
The New Zealand ACL Registry is a nation-wide registry that was established in 2014 to prospectively capture data on patient, surgical and follow-up variables. Since 2017, it is mandatory for all orthopaedic surgeons who perform ACL reconstructions to actively participate in the registry in order to achieve recertification [46]. As of 2018, based on comparisons to Government healthcare data, it is estimated that approximately 85% of all ACL reconstructions performed in New Zealand are captured by the registry [47].
Patient demographic data is collected through a pre-operative patient questionnaire. An operative data form detailing each reconstruction procedure is completed by the surgeon. This includes the presence of any injury to the menisci and any subsequent meniscal surgery (resection or repair) performed. Subsequently, patients and surgeons can report post-operative complications, including reoperations, and this is recorded in the Registry database. Any reoperation reported to the registry is reviewed by the Registry Administrator who contacts the operating surgeon for the operation note. The operation note is manually reviewed with details of the procedure retrieved and documented in the Registry database.
Accident Compensation Corporation (ACC)
The ACC is the New Zealand Government’s sole provider of accident insurance for all injuries. As nearly all ACL injuries are accidental, patients who undergo ACL reconstruction are fully funded. Any subsequent treatment related to the reconstruction, such as a reoperation, is also funded. Every procedure funded by the ACC is recorded in a database which includes other details such as the injury mechanism, date, side, location of injury as well as the cost of treatment. Although the ACC lacks the in-depth intraoperative data that is recorded by the New Zealand ACL Registry, it is able to identify whether a patient who has undergone an ACL reconstruction has had any subsequent reoperations.
Patient population and inclusion criteria
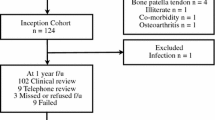
Meniscal repairs performed during a primary isolated single-bundle ACL reconstruction were retrospectively reviewed. The study period was April 2014 to May 2020, allowing for a minimum follow-up of six months. Patients who underwent multi-ligament reconstruction, osteotomy or unicompartmental knee replacement were excluded. Meniscal repairs performed for root tears were excluded (n = 24 medial root tears and n = 134 lateral root tears).
Outcome of interest
The primary outcome of interest was meniscal repair failure, defined as a repair that underwent subsequent meniscectomy. In this study, a reoperation for meniscectomy was recorded in two ways:
-
(1)
Reoperations reported to the Registry through the post-operative complication form
-
(2)
Reoperations recorded by the ACC database
In New Zealand, every patient who uses healthcare services has a National Health Index (NHI) number that allows them to be uniquely identified within the healthcare system. In this study, the NHI of every patient was used to match their records from the Registry to the ACC database. Any reoperation that was recorded in the ACC database was retrieved. For every reoperation identified, the operation note was reviewed by the Registry Administrator. The exact details of the reoperation were retrieved, including any subsequent meniscectomy and the side (medial versus lateral). There were five cases where both menisci were repaired and underwent a subsequent meniscectomy but the side(s) that was resected was not specified on the reoperation note. In these cases, we included this as a failure of both repairs.
Predictor variables
The predictor variables of interest were recorded by the New Zealand ACL Registry through the pre-operative patient questionnaire and the operative data form completed by the surgeon. This included patient age, sex, time from injury-to-surgery, history of previous knee surgery, examination under anaesthesia findings, graft type, graft diameter, femoral tunnel drilling technique, the location and degree of cartilage injury, graded according to the International Cartilage Injury Repair Society (ICRS) scale, and any treatment of a cartilage injury. Meniscal repair technique, implant or suture choice was also recorded. Surgeon volume was calculated as the average number of primary ACL reconstructions recorded annually in the Registry.
Statistical analyses
Descriptive statistics were provided as mean values with standard deviation (SD) or median values with interquartile ranges (IQR). Continuous variables were assessed for normality through visualisation of Q-Q plots and histograms. Univariate analysis of the rate of meniscal repair failure was performed using Chi-Square Test for categorical variables and Student t-test or Mann–Whitney U Test for continuous variables. Multivariate survival analysis of the risk of meniscal repair failure was performed via a Cox proportional hazards regression model. The assumption of proportional hazards was assessed via log(-log) plots. Hazard ratios (HR) with 95% confidence intervals (CI) were computed to identify independent risk factors for meniscal repair failure. Results were considered statistically significant at p < 0.05. All analyses were performed using IBM SPSS Statistics version 25.
Results
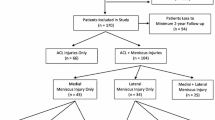
Between April 2014 and May 2020, a total of 6125 out of 10,288 primary ACL reconstructions (60%) involved concurrent meniscal surgery (resection or repair) of either the medial or lateral meniscus. Patient demographics are described in Table 1. Concurrent surgery was performed in both menisci in 1381 patients (13%). There were 3024 meniscal repairs performed in 2699 patients, of which 1814 were a medial repair (60%) and 1210 were a lateral repair (40%). Both menisci were repaired in 325 patients (12%). Of the 1814 medial repairs, 1640 were performed using an all inside suture device (90%), 159 using an outside in or inside out suture (9%) and 15 using both techniques (1%). Of the 1210 lateral repairs, 1074 were performed using an all inside suture device (89%), 125 using an outside in or inside out suture (10%) and 11 using both (1%). The overall failure rate of a meniscal repair was 6.6% (n = 201) at a mean follow-up of 2.9 years (SD ± 1.5 years).
Medial meniscal repair failure
One-hundred and forty-two out of 1814 medial meniscal repairs failed and underwent a subsequent meniscectomy (7.8%, Table 2).
On univariate analysis, a higher failure rate was associated with the hamstring tendon autograft, an ICRS Grade 1–4 injury in the medial compartment, and when the repair was performed by a low volume surgeon who performs < 30 ACL reconstructions per year.
On multivariate survival analysis, failure of a medial meniscal repair was over two times more likely in patients with a hamstring tendon autograft (adjusted HR = 2.20, 95% CI 1.36–3.56, p = 0.001), 1.6 times more likely in patients aged 21–30 years (adjusted HR = 1.60, 95% CI 1.30–2.48, p = 0.037) and 1.8 times more likely in patients with cartilage injury in the medial compartment (adjusted HR = 1.75, 95% CI 1.23–2.48, p = 0.002, Table 3). Surgeon volume was not a risk factor for medial repair failure.
Lateral meniscal repair failure
Fifty-nine out of 1210 lateral meniscal repairs failed and underwent a subsequent meniscectomy (4.9%, Table 2).
On univariate analysis, a higher failure rate was associated with younger age, low volume surgeons and a transtibial technique when drilling the femoral graft tunnel.
On multivariate survival analysis, the risk of failure was nearly three times higher in patients aged ≤ 20 years when compared to patients older than 30 years (adjusted HR = 2.79, 95% CI 1.17–6.67, p = 0.021, Table 4). Low volume surgeons had a 1.8 times higher risk of failure compared to high volume surgeons (adjusted HR = 1.84, 95% CI 1.08–3.13, p = 0.026). The transtibial femoral tunnel drilling technique was over two times more likely to result in a failure when compared to the anteromedial portal technique (adjusted HR = 2.30, 95% CI 1.03 – 5.15, p = 0.042).
Other factors
Patient sex, time from injury-to-surgery, a history of previous knee surgery and graft diameter did not influence the rate of meniscal repair failure.
Discussion
The most important findings of this study are that the use of a hamstring tendon autograft, younger age and concomitant cartilage injury in the medial compartment are risk factors for medial meniscal repair failure, whereas younger age, low surgeon volume and a transtibial femoral tunnel drilling technique are risk factors for lateral meniscal repair failure. The overall meniscal repair failure rate was 6.6%, with medial repairs demonstrating a higher failure rate (7.8%) when compared to lateral repairs (4.9%).
The medial and lateral menisci are commonly injured structures in patients who have ruptured their ACL [2, 8, 9, 41]. In 16,192 ACL reconstructions recorded in the Kaiser Permanente Registry, meniscal injuries were reported in 61% and 53% of primary and revision ACL reconstructions respectively [17]. In New Zealand, a meniscal injury is reported in 60% and 58% of primary and revision ACL reconstructions respectively [25]. Repairing the meniscus can protect against post-traumatic osteoarthritis, improve return to activity and decrease the force on the ACL graft when compared to resection [4, 14, 21, 38, 45]. However, meniscal repair is associated with a higher rate of reoperation compared to resection [22]. In this study, 8% of medial and 5% of lateral meniscal repairs resulted in a subsequent meniscectomy. A similar rate is reported by Toman et al. who performed a study of 77 meniscal repairs in concurrent primary ACL reconstruction, and found that three patients underwent subsequent meniscectomy (4%) [38]. Rodríguez-Roiz et al. analysed 49 amateur athletes who underwent concurrent meniscal repair and primary ACL reconstruction and found that 8% underwent subsequent partial meniscectomy [28]. However, in a systematic review of 95 studies performed by Paxton et al., 148 out of 1044 meniscal repairs performed in primary ACL reconstruction underwent a reoperation (14%) [22].
The present study found a higher failure rate in repairs of the medial meniscus compared to the lateral meniscus which supports the current literature [15, 22, 29, 38]. This may be explained by structural differences between the menisci, as the medial meniscus is securely attached to the medial collateral ligament and tibial plateau and is therefore less mobile and may face higher strain under loading [15, 22, 28]. Interestingly, the use of a hamstring tendon autograft was the most significant risk factor for medial repair failure. The use of the hamstring tendon autograft is associated with a higher risk of residual laxity following ACL reconstruction when compared to the BTB autograft [19]. As the medial meniscus plays an important role as a secondary knee stabilizer that helps control anterior tibial translation and joint laxity [4, 15, 20], any residual laxity following ACL reconstruction may further increase the strain through the medial meniscus and increase the risk of reinjury [15, 22].
The effect of residual laxity on outcomes of meniscal repair may also be demonstrated by the finding of a higher lateral repair failure rate when a transtibial technique was used to drill the femoral graft tunnel when compared to an anteromedial portal technique. When using the transtibial drilling technique, the position of the femoral graft tunnel is limited and restricted to the angle of the tibial tunnel. It is therefore more likely to result in a vertical graft orientation and a non-anatomical ACL reconstruction [39]. As a result, the transtibial technique may lead to greater residual laxity and rotational instability which may explain the higher rate of meniscal repair failure [1, 12, 35].
In the present study, younger age was associated with a higher risk of both medial and lateral meniscal repair failure. Younger age is also the most commonly reported risk factor for ACL graft rupture [7, 11, 16, 25, 26, 44]. The association between younger age and repeat injury is likely to be related to their return to activity as younger patients are more likely to return to high-contact pivoting sports [5, 42,43,44]. Other possible explanations are related to low adherence to rehabilitation protocols and premature return to activity in young athletes [15, 23, 40].
Surgeon volume is a commonly analysed variable in outcomes of knee surgery, with some studies suggesting poorer outcomes in low volume surgeons [3, 10, 18]. In a study of 77,899 ACL reconstructions performed in New York State hospitals, a 29% decreased risk of ipsilateral knee surgery was reported in procedures performed by surgeons with a volume of > 35 cases per year [31]. Lyman et al. performed a study of 9,609 meniscal repairs and found that a surgeon volume of ≥ 24 cases a year decreased the risk of failure in isolated repairs, but not in concurrent ACL reconstruction [15]. In contrast, our study of meniscal repair in concurrent ACL reconstruction found an almost two times higher risk of lateral meniscal repair failure when the procedure was performed by a surgeon with an average volume of < 30 cases per year, but no difference in medial meniscal repair failure rates. Interestingly, this study demonstrated that nearly 50% of primary ACL reconstructions are being performed by surgeons who do less than 30 reconstructions a year. These findings support previous literature suggesting higher volume surgeons have lower reoperation rates following ACL reconstruction with concurrent meniscal repair [15].
This study is limited to analysing the rate of subsequent meniscectomy as a proxy measure for repair failure. As not all patients who reinjure their meniscus will proceed to a second surgical procedure, this will underestimate the true rate of repair failure. However, subsequent meniscectomy is the standard outcome measure that is most frequently used in the literature to define a meniscal repair failure [15, 22]. Using this outcome therefore allows for comparisons with other studies and may assist future meta-analyses. Another strength of the present study was the combination of data from two national databases, the New Zealand ACL Registry and the ACC. The operation note for each reoperation was manually reviewed which ensured accurate identification of whether a meniscectomy was performed and the side of the meniscus (medial or lateral) that was resected. Another limitation of this study is the mean follow-up of three years, which therefore represents early results. However, this study focused on analysing surgical risk factors which are likely to contribute to early rather than late failures. Furthermore, the Cox proportional hazards regression model was used to adjust for differences in follow-up between patients. Lastly, details related to size and classification of the meniscal tear, the number of sutures implanted when repairing the meniscus and differences in rehabilitation protocol are not recorded by the Registry, and are limitations of such retrospective analyses. Although Registry studies can offer large patient numbers and demonstrate associations, they are unable to investigate the cause of the association and do not infer causality. Future prospective studies should aim to analyse these factors.
The clinical relevance of this study is that surgeons should be aware of the effect of graft choice when repairing a meniscal tear during concurrent ACL reconstruction. Patients can be advised of the higher failure rate of medial versus lateral repairs, as well as the effect of patient age, concomitant cartilage injury and surgeon case volume on meniscal repair outcomes.
Conclusion
In over 3000 meniscal repairs performed concurrently with primary ACL reconstruction at a mean follow-up of 3 years, the overall rate of subsequent meniscectomy was 6.6%. The use of hamstring tendon autografts, younger age and concomitant cartilage injury in the medial compartment were associated with medial meniscal repair failure. Younger age, surgeons who performed an annual average case volume of less than 30 primary ACL reconstructions and a transtibial femoral tunnel drilling technique were risk factors for lateral meniscal repair failure.
Data availability
Data not available.
References
Bedi A, Musahl V, Steuber V, Kendoff D, Choi D, Allen AA et al (2011) Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy 27:380–390
Brambilla L, Pulici L, Carimati G, Quaglia A, Prospero E, Bait C et al (2015) Prevalence of associated lesions in anterior cruciate ligament reconstruction. Am J Sports Med 43:2966–2973
Capogna BM, Mahure SA, Mollon B, Duenes ML, Rokito AS (2020) Young age, female gender, Caucasian race, and workers’ compensation claim are risk factors for reoperation following arthroscopic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc Springer 28:2213–2223
Cristiani R, Rönnblad E, Engström B, Forssblad M, Stålman A (2018) Medial meniscus resection increases and medial meniscus repair preserves anterior knee laxity: a cohort study of 4497 patients with primary anterior cruciate ligament reconstruction. Am J Sports Med 46:357–362
Edwards PK, Ebert JR, Joss B, Ackland T, Annear P, Buelow JU et al (2018) Patient characteristics and predictors of return to sport at 12 months after anterior cruciate ligament reconstruction: the importance of patient age and postoperative rehabilitation. Orthop J Sport Med 6:1–8. https://doi.org/10.1177/2325967118797575
Engebretsen L, Forssblad M, Lind M (2015) Why registries analysing cruciate ligament surgery are important. Br J Sports Med 49:636–637
Faunø P, Rahr-Wagner L, Lind M (2014) Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the danish registry of knee ligament reconstruction. Orthop J Sport Med 2:1–7. https://doi.org/10.1177/2325967114552405
Granan LP, Baste V, Engebretsen L, Inacio MCS (2015) Associations between inadequate knee function detected by KOOS and prospective graft failure in an anterior cruciate ligament-reconstructed knee. Knee Surg Sports Traumatol Arthrosc 23:1135–1140
Hagino T, Ochiai S, Senga S, Yamashita T, Wako M, Ando T et al (2015) Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg 135:1701–1706
Jain N, Pietrobon R, Guller U, Shankar A, Ahluwalia AS, Higgins LD (2005) Effect of provider volume on resource utilization for surgical procedures of the knee. Knee Surg Sports Traumatol Arthrosc 13:302–312
Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP (2015) Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med 43:1583–1590
Lee MC, Seong SC, Lee S, Chang CB, Park YK, Jo H et al (2007) Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy 23:771–778
Lozano J, Ma CB, Cannon WD (2007) All-inside meniscus repair: a systematic review. Clin Orthop Relat Res 455:134–141
Lutz C, Dalmay F, Ehkirch FP, Cucurulo T, Laporte C, Le Henaff G et al (2015) Meniscectomy versus meniscal repair: 10 years radiological and clinical results in vertical lesions in stable knee. Orthop Traumatol Surg Res 101:S327–S331
Lyman S, Hidaka C, Valdez AS, Hetsroni I, Pan TJ, Do H et al (2013) Risk factors for meniscectomy after meniscal repair. Am J Sports Med 41:2772–2778
Maletis GB, Chen J, Inacio MCS, Funahashi TT (2016) Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the kaiser permanente anterior cruciate ligament registry. Am J Sports Med 44:331–336
Maletis GB, Inacio MCS, Funahashi TT (2013) Analysis of 16,192 anterior cruciate ligament reconstructions from a community-based registry. Am J Sports Med 41:2090–2098
Meyer E, Weitzel-Kage D, Sohr D, Gastmeier P (2011) Impact of department volume on surgical site infections following arthroscopy, knee replacement or hip replacement. BMJ Qual Saf 20:1069–1074
Mohtadi NG, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 2011:CD005960
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38:1591–1597
Nakayama H, Kanto R, Kambara S, Kurosaka K, Onishi S, Yoshiya S et al (2017) Clinical outcome of meniscus repair for isolated meniscus tear in athletes. Asia-Pacific J Sport Med Arthrosc Rehabil Technol 10:4–7. https://doi.org/10.1016/j.asmart.2017.05.299
Paxton ES, Stock MV, Brophy RH (2011) Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy 27:1275–1288
Rahardja R, Love H, Clatworthy MG, Monk AP, Young SW (2021) Higher rate of return to preinjury activity levels after anterior cruciate ligament reconstruction with a bone-patellar tendon–bone versus hamstring tendon autograft in high-activity patients: results from the New Zealand ACL registry. Am J Sports Med 49:3488–3494
Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW (2020) Effect of graft choice on revision and contralateral anterior cruciate ligament reconstruction: results from the New Zealand ACL registry. Am J Sports Med 48:63–69
Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW (2020) Rates of revision and surgeon-reported graft rupture following ACL reconstruction: early results from the New Zealand ACL registry. Knee Surg Sports Traumatol Arthrosc 28:2194–2202
Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW (2020) Factors associated with revision following anterior cruciate ligament reconstruction: a systematic review of registry data. Knee 27:287–299
Ralles S, Agel J, Obermeier M, Tompkins M (2015) Incidence of secondary intra-articular injuries with time to anterior cruciate ligament reconstruction. Am J Sports Med 43:1373–1379
Rodríguez-Roiz JM, Sastre-Solsona S, Popescu D, Montañana-Burillo J, Combalia-Aleu A (2020) The relationship between ACL reconstruction and meniscal repair: quality of life, sports return, and meniscal failure rate - 2- To 12-year follow-up. J Orthop Surg Res 15:361
Ronnblad E, Barenius B, Engstrom B, Eriksson K (2020) Predictive factors for failure of meniscal repair: a retrospective dual-center analysis of 918 consecutive cases. Orthop J Sport Med 8:1–7
Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Årøen A (2013) Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from norway and sweden of 8476 patients with 2-year follow-up. Am J Sports Med 41:535–543
Schairer WW, Marx RG, Dempsey B, Ge Y, Lyman S (2017) The relation between volume of ACL reconstruction and future knee surgery. Orthop J Sport Med 5:232596711S0029
Schweizer C, Hanreich C, Tscholl PM, Ristl R, Apprich S, Windhager R et al (2022) Nineteen percent of meniscus repairs are being revised and failures frequently occur after the second postoperative year: a systematic review and meta-analysis with a minimum follow-up of 5 years. Knee Surg Sports Traumatol Arthrosc 30:2267–2276
Sri-Ram K, Salmon LJ, Pinczewski LA, Roe JP (2013) The incidence of secondary pathology after anterior cruciate ligament rupture in 5086 patients requiring ligament reconstruction. Bone Joint J. 95-B:59–64
Stein T, Mehling AP, Welsch F, Von Eisenhart-Rothe R, Jäger A (2010) Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med 38:1542–1548
Steiner ME, Battaglia TC, Heming JF, Rand JD, Festa A, Baria M (2009) Independent drilling outperforms conventional transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med 37:1912–1919
Stone JA, Perrone GS, Nezwek TA, Cui Q, Vlad SC, Richmond JC et al (2019) Delayed ACL reconstruction in patients ≥40 years of age is associated with increased risk of medial meniscal injury at 1 year. Am J Sports Med 47:584–589
Sutherland K, Clatworthy M, Chang K, Rahardja R, Young SW (2019) Risk factors for revision anterior cruciate ligament reconstruction and frequency with which patients change surgeons. Orthop J Sport Med 7:1–7. https://doi.org/10.1177/2325967119880487
Toman CV, Dunn WR, Spindler KP, Amendola A, Andrish JT, Bergfeld JA et al (2009) Success of meniscal repair at anterior cruciate ligament reconstruction. Am J Sports Med 37:1111–1115
Tompkins M, Milewski MD, Brockmeier SF, Gaskin CM, Hart JM, Miller MD (2012) Anatomic femoral tunnel drilling in anterior cruciate ligament reconstruction. Am J Sports Med 40:1313–1321
De Valk EJ, Moen MH, Winters M, Bakker EWP, Tamminga R, Van Der Hoeven H (2013) Preoperative patient and injury factors of successful rehabilitation after anterior cruciate ligament reconstruction with single-bundle techniques. Arthroscopy 29:1879–1895
Vavken P, Tepolt FA, Kocher MS (2018) Concurrent meniscal and chondral injuries in pediatric and adolescent patients undergoing ACL reconstruction. J Pediatr Orthop 38:105–109
Webster KE, Feller JA (2018) Return to level i sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Orthop J Sport Med 6:1–6
Webster KE, Feller JA, Whitehead TS, Myer GD, Merory PB (2017) Return to sport in the younger patient with anterior cruciate ligament reconstruction. Orthop J Sport Med 5:1–4
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD (2016) Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction. Am J Sports Med 44:1861–1876
Xu C, Zhao J (2015) A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc 23:164–170
New Zealand ACL Registry Annual Report 2017.
New Zealand ACL Registry Annual Report 2018.
Acknowledgements
The authors acknowledge Charlotte Smith, the database administrator from the New Zealand ACL Registry, for her ongoing support, assistance, and data quality assurance.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this study.
Ethical approval
Exempt from Health and Disability Ethics Committee review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rahardja, R., Love, H., Clatworthy, M.G. et al. Meniscal repair failure following concurrent primary anterior cruciate ligament reconstruction: results from the New Zealand ACL Registry. Knee Surg Sports Traumatol Arthrosc 31, 4142–4150 (2023). https://doi.org/10.1007/s00167-023-07424-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07424-w