Abstract
Purpose
The purpose of this study was to synthesize and quantitatively assess the outcomes of ACL Revision using a quadriceps tendon (QT) graft and to compare them with those of ACL Revisions performed with hamstring tendons (HT) graft.
Methods
A comprehensive search based on the PRISMA protocol was performed across PubMed, Scopus, Embase, and Cochrane Library from inception until February 2022. Clinical studies reporting the outcomes of ACL Revision with QT autograft were included. Subjective and Objective IKDC, Tegner activity level, Lysholm knee score, KOOS score, VAS for pain, knee laxity (KT-1000/2000 arthrometer, Lachman test, and pivot-shift test), and graft failure were assessed. A systematic review and meta-analysis were performed and a quality assessment of the included studies was carried out with the MINORS score.
Results
Seven studies met the selection criteria and were included in the systematic review for the qualitative synthesis of data. A pooled mean of all the variables was provided for the 7 studies, while 3 studies included a control group of ACL Revision with HT and were included in a meta-analysis. A total of 420 participants with a mean age of 28.9 ± 10.5 years and a mean postoperative follow-up of 39.3 ± 16.4 months were assessed. Of these, 277 patients underwent ACL Revision with QT and 143 patients underwent ACL Revision with HT. In the QT group, average graft failure was 9.8% compared to 17.4% in the HT group. KOOS Sport and pivot-shift test showed better postoperative outcomes in QT than HT, although it was not statistically significant (p = 0.052).
Conclusion
The QT autograft was associated with an improved trend of rotatory laxity, PROMs and failure rate compared to HT autograft after revision ACL reconstruction. The QT autograft for revision ACL reconstruction is supported by the current literature. It is a viable graft that should be considered for both primary and revision ACL reconstruction.
Level of evidence
Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The increasing rates of Anterior Cruciate Ligament (ACL) reconstructions lead to an increased burden of failures which will subsequently need revision surgery [1,2,3]. Revision reconstruction is technically more challenging due to the removal of prior implants, appropriate tunnel positioning, muscle weakness following the primary reconstruction, and higher concomitant injuries [4, 5]. As techniques have improved so have the outcomes following revision surgery, however, inferior results were reported with a revision surgery than with primary ACL surgery [4, 6]. A higher failure rate has been reported with revision ACL reconstruction compared to primary reconstruction, highlighting the clinical relevance of revision surgery for failed ACL reconstruction [1, 7].
In primary ACL reconstruction, hamstring tendon (HT) and bone–patellar tendon–bone (BPTB) autografts are the most commonly used graft, [8]. However, in a revision case where the ipsilateral graft has already been used, it will be difficult to convince the patient to undergo a procedure on the contralateral uninjured limb, for graft harvesting [9].
In recent years, the quadriceps tendon (QT) autograft has gained popularity for ACL reconstruction [10]. The QT graft has been reported to provide a broader base for anatomic insertion of the reconstructed ACL to the tibia [11], has a greater mean cross-sectional area compared to the BPTB and HT [12], and has a greater load to failure than other grafts. Harvesting of QT autograft has lower donor-site morbidity than BPTB and HT harvesting [13] and preservation of muscle strength in knee flexion compared to the HT graft [14]. Despite these potential benefits that can translate into better clinical outcomes, the QT graft has been studied less extensively, particularly in the revision setting. Of the few studies available, some are retrospective reviews of data with relatively small sample sizes that do not allow generalization of the findings [5, 15, 16].
To the best of the authors’ knowledge, no systematic review or meta-analysis is available in the literature on the QT autograft used in revision ACL reconstruction. Therefore, the purpose of this study was to synthesize and qualitatively assess the evidence available currently in the literature on the QT graft for revision ACL reconstruction. The hypothesis was that better functional outcomes and lesser graft failure will be found in the QT group compared to HT graft for revision ACL reconstruction.
Materials and methods
This meta-analysis followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to identify and extract eligible articles [17] and was registered on the PROSPERO International Prospective Register of Systematic Reviews (ID: CRD42022308299).
Search strategy
Two independent authors (A.M. and S.D.P.) conducted a comprehensive search across multi-databases (PubMed, Scopus, Embase, and Cochrane Library) and reviewed each article’s title and abstract for studies available until February 2022. The search terms used were (ACL OR “anterior cruciate ligament”) AND (“quad*” OR “QT”) AND (“revision“Z” OR “reoperation”). The full texts of the studies were evaluated when eligibility could not be assessed from the title and abstract. Both of these two authors independently assessed the eligibility of studies and any disagreements were resolved by discussion if disagreement could not be resolved, then the senior author (C.F.) was consulted.
Inclusion and exclusion criteria
Clinical studies of any study design reporting on outcomes following revision ACLR with QT autograft were considered for inclusion. The following outcomes were looked at in the studies: IKDC score, Tegner activity level, Lysholm knee score, KOOS score, VAS for pain; knee laxity measured with KT-1000/2000 arthrometer, Lachman test, and pivot-shift test. Non-English studies, review articles, non-peer-reviewed studies, surgical techniques, case reports, conference abstracts, biomechanical studies, as well as studies solely focused on primary ACL reconstruction, use of graft other than QT autograft, sample size less than 15 patients, and minimum follow-up less than 2 years were excluded.
Methodological quality assessment
Quality assessment of the included studies was performed using the methodological index for non-randomized studies (MINORS) criteria (Table 1) [18]. Two authors (A.M. and S.D.P.) independently assessed the quality of each article. The senior author (C.F.) was consulted in case of disagreement.
Data extraction
Demographic data including age at surgery, sex, and follow-up duration were extracted to provide an overview of the cohort. For each study, the following data were extracted: IKDC score, Tegner activity level, Lysholm knee score, KOOS score, VAS for pain; knee laxity measured with KT-1000/2000 arthrometer, Lachman test, pivot-shift test, pivoting sports, and graft failure rates (Table 2).
Statistical analysis
The continuous variables were extracted and analyzed as mean and standard deviation (SD) using an Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA). When median and interquartile ranges were reported, these were converted into mean and SD. If it was not possible to calculate the SD from the available data, the highest SD was used. The categorical variables were reported as sum and percentage over the total.
A meta-mean weighted over the number of patients was computed separately for QT and HT groups for each clinical outcome and laxity measurement. The studies reporting data for both the HT and QT groups were included in a meta-analysis (Fig. 1). The standardized mean difference (SMD) and 95% confidence interval (CI) were calculated for continuous variables referring to the same clinical outcome or laxity measure. The Odds Ratio (OR) and 95% CI were instead computed for the categorical variables. The Higgins’ I2 statistics were calculated to determine the heterogeneity. The pooled estimates of the effect size were presented as forest plots per each variable. The Mantel–Haenszel random-effects model was used to pool the data if statistically significant heterogeneity was reached; the fixed-effects model was used otherwise. Statistical significance was set at P < 0.05. All the analyses were conducted in MedCalc Statistical Software version 19.2.6 (MedCalc Software Ltd, Ostend, Belgium).
Results
Search results
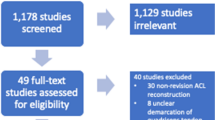
For this study, 394 potentially relevant articles were identified in the initial comprehensive search. Following the deletion of duplicate titles, 203 abstracts were yielded for screening. A further 179 articles were excluded based on abstract screening; 24 articles were obtained in full text and the inclusion and exclusion criteria were applied. Seventeen articles were removed after full-text screening due to various reasons. Finally, 7 studies met the selection criterion, but only 3 studies had a control group (HT graft) which underwent metanalysis. All 7 studies were included in the systematic review and for the qualitative synthesis of data (Fig. 1).
Study design and characteristics
Among the 7 included studies, 1 was a prospective case–control study, 2 were prospective cohorts, and 4 were retrospective studies. All studies reported the use of a single-staged revision procedure except the study by Eggeling et al. [16] where a two-staged revision was reported. According to the MINORS scale, 4 studies were rated as “high quality” (score 11 or more), while 3 as “low quality” (score < 11), mostly due to a lack of unbiased outcomes assessment and prospective size calculation (Table 1).
Systematic review of outcomes of ACL Revision with QT
A total of 277 patients with a mean age of 30.6 ± 7.1 and a mean postoperative follow-up of 40.2 months underwent ACL Revision with QT and were included in the quantitative synthesis.
Patient-reported outcome measures
The Lysholm knee score was reported in 156 patients from 5 studies [9, 15, 16, 19, 20], showing an average postoperative value of 86.4 points. Significant improvement was reported in both the groups with QT and HT grafts. However, pooled averages of Lysholm scores show a higher functional score with QT (86.1) than with HT (82.2) grafts postoperatively. The Subjective IKDC score was reported in patients from 2 studies, showing an average postoperative value of 82.1 points. The KOOS score was reported in 2 studies as well, including 68 patients and showing an average postoperative value of 86.9 points for the Pain subscale, 82.1 for the Symptoms subscale, 92.8 for the ADL subscale, 79.6 for Sports subscale, and 61.5 for Qol subscale. The Subjective IKDC score was reported in 184 patients from 3 studies, showing an average postoperative value of 81.9 points (Table 3).
Laxity assessment
Clinical measures of laxity used were the KT-1000 arthrometer side-to-side difference (SSD), in 4 studies [5, 9, 15, 19]. Pooled average of postoperative KT-1000 SSD measurement was 1.8 mm for QT and 2.4 mm for HT grafts, and thus, QT grafts showed lesser laxity (Table 3). The manual antero-posterior laxity with the Lachman test was reported in 71 patients from 2 studies, showing negative tests in 56 (78.8%) and grade 1 in 15 (19.7%) of patients. Similarly, the pivot-shift test was reported in 133 patients from 4 studies, showing negative tests in 107 (80.5%) and grade 1 in 21 (15.8%) of patients. Instrumental antero-posterior laxity was reported in 258 patients from 6 studies, showing an average postoperative value of 1.9 mm.
Complications and graft failures
A complication was reported in 27 out of 277 patients (9.7%), hypersensitive scars in 5 patients, infection in two cases, donor-site morbidity in two cases, and cyclops syndrome in 1 patient. Graft failure was reported in 15 out of 277 patients, for an overall rate of 5.4%. Failure of revision ACL reconstruction was reported in 4 studies [5, 9, 15, 16]. In the QT group, graft failure was 12 (9.8%) compared to 8 (17.4%) in the HT group.
Rehabilitation protocol
The postoperative protocol, reported in all except one study [16], varied among the included studies regarding brace use, weightbearing, and range of motion (Table 4).
Return to sports activity
Return to sports activity was assessed in five of the seven studies [5, 15, 19,20,21]. Running was allowed at 3 months except in one study [21] where running was allowed at 6 months. In all of the five studies, return to sports was allowed at 6–9 months.
Meta-analysis of outcomes of ACL Revision with QT versus HT
A total of 109 patients with a mean age at surgery of 34.3 years underwent Revision ACL with QT, while 109 patients with a mean age at surgery of 30.1 years underwent Revision ACL with HT. The follow-up ranged from 24 to 83 months.
Patient-reported outcome measures
The results of the meta-analysis are depicted in Fig. 2 and Fig. 3. The Lysholm knee score used in 3 studies [9, 15, 16] was used for the meta-analysis (on a restricted cohort), which showed that the difference was not statistically significant (p > 0.05). The IKDC score, used in 2 studies [15, 16], showed conflicting findings. In the study by Eggeling et al. [16], postoperative IKDC with QT graft was 83.8 ± 12.2 and with HT graft was 78.6 ± 16.8, while in the study by Barie et al. [15], postoperative IKDC with QT graft was 79 ± 15 and with HT graft was 82 ± 12 (Table 2).
Meta-analysis (part 2), forest plots showing laxity and functional outcomes between QT and HT autografts. The standardized mean difference (SMD) and standard error (SE) or odds ratio (OR) were reported for continuous and categorical variables, respectively. A 95% confidence interval (CI) was reported
The KOOS scale was used in 2 studies [9, 16]. Among the five subscales of the KOOS, pooled average scores were higher for the QT graft for QoL (Quality of life), Sport and Symptom subscales (Table 3). KOOS Sport showed an SMD = 0.33 [0.00–0.66] (n.s., Fig. 2). The KOOS were similar in the ADL and Pain subscales. The Tegner Activity scale was used in 3 studies [15, 16, 19]. The pooled average postoperative Tegner activity levels were higher for QT than for HT (5.9 vs 5.6, n.s.). In the study by Eggeling et al. [16], the postoperative VAS score for pain significantly improved in the QT group compared to the HT group (p < 0.05).
Laxity assessment
Postoperative KT-1000 SSD measurement showed lower laxity for QT than HT, although it was not significant (n.s., Fig. 3). Similarly, lower (non-significant) laxity was found in Rollimeter SSD in the QT group compared to the HT group [16] and lower (non-significant) pivoting was reported in the QT group compared to the HT group [15, 16].
Discussion
The most important findings of this study are that the quadriceps tendon graft has good results in revision ACL setting, being similar to the results of ACL revision with hamstring tendon grafts and that there is a trend of better results for certain outcome measures such as the Lysholm knee score, KOOS subscales for Quality of life, Sports activity and symptoms, the Tegner activity levels, and VAS for pain postoperatively. The QT group was also associated with lesser postoperative laxity, quantified using KT-1000 SSD, pivot-shift test, Lachman test, and Rollimeter. Moreover, QT autograft had lesser failure compared to HT graft for revision ACL reconstruction. However, the meta-analysis showed no significant differences between the group for all the variables.
Various studies found equal or better outcomes with QT graft than HT and BPTB autograft in primary ACL reconstruction [13, 14, 22,23,24]. Runner et al. [23] and Cavaignac et al. [22] compared the functional outcomes between QT and HT groups, and they found better results in the QT group. Similarly, a recent meta-analysis reported higher functional scores in the QT than in the HT group [13]. The findings of the previous studies are similar to the current study; however, these previous studies focused on primary ACL reconstruction, whereas, in the current metanalysis, only revision studies were included. In a recent revision ACL study, the QT group showed small increases in IKDC scores and Tegner activity levels than the HT group [16]. Similarly, in another included study, authors found higher Lysholm, IKDC, and KOOS scores in the QT group compared to the HT group [9]. This suggests that QT autograft is a viable option in both the primary and revision ACL reconstruction than the HT autograft.
In the present study, the QT graft was associated with lesser postoperative laxity compared to the HT graft. In the QT group, no cases of grade 3 laxity were found. Although both graft choices give good results with respect to postoperative laxity, the quadriceps tendon graft seems to edge out the hamstring graft. Lesser postoperative laxity may be a possible reason for better postoperative KOOS sports subscale in the QT group than in the HT group. Similar findings were reported by Cavaignac et al. [22] in their primary ACL reconstruction. They found lower pivot-shift grade, Lachman grade, and side-to-side difference measured by KT-1000 arthrometer in the QT group than HT group. In another study, the QT graft showed lesser laxity on pivot-shift testing and also lower failure rates when compared to the HT graft, in the setting of primary ACL reconstruction surgery [25]. The present study suggests lesser postoperative laxity in the QT group than in the HT group and these findings are similar to previous literature.
In the current study, Tegner activity was better in the QT group than in the HT group (5.9 vs. 5.6). Similarly, KOOS sport was also better in the QT group than in the HT group (79.7 vs. 70.9). These findings indicate a better return to sports after revision ACL reconstruction with QT autograft. In revision ACL reconstruction, majority of surgeons prolong the time for a return to sports. This fact was also verified in the current study where return to sporting activity was allowed at around 6–9 months in the 5 studies [5, 15, 19,20,21]. Only the study by Barie et al. [15] compared sporting activity participation postoperatively between the QT and HT groups. They found that the proportion of patients participating postoperatively in pivoting sports was significantly higher in the HT group. However, this could be partly explained by the fact that the HT group had a higher Tegner activity level preoperatively than the QT group which would reflect not only better knee health among this group but would also reflect a better overall general physical condition among this group which would influence postoperative rehabilitation and level of activity attained.
The selection of graft is an important factor in revision ACL reconstruction as the rate of graft failure can be directly correlated with the type of graft. Higher graft failure was reported in revision ACL reconstruction with allograft compared to autograft [1, 26]. QT autograft has good anatomical characteristics with respect to graft volume, graft thickness, and graft length; these characteristics are comparable to HT and BPTB autografts [23, 24, 27]. Previous studies showed superior biomechanical properties with QT compared to BPTB with respect to load to failure, strain at failure, and Young’s modulus of elasticity [28, 29]. In the present meta-analysis, a lower graft failure rate was found in the QT group than in the HT group. Eggeking et al. [16] reported significantly higher failures with HT graft than with QT (1 QT failure compared to 8 HT graft failures). Similarly, in a recent meta-analysis, graft failure was significantly higher in the HT group than QT group for primary ACL reconstruction [25].
Despite these promising biomechanical and clinical studies, QT autografts are not widely used. One of the major factors responsible for its lesser use is historical harvesting techniques, where extensive dissection of extensor apparatus leads to quadriceps weakness and graft harvested by older techniques was biomechanically weaker and associated with residual rotatory knee laxity [29]. Moreover, the paucity of long-term clinical trials and large cohort studies makes the QT autograft a difficult choice for surgeons, who are more convenient with conventional BPTB and HT considering their satisfactory long-term results. However, with the increasing number of revision ACLs and the highly active patient population, it is necessary to study other graft options beyond the conventional HT and BPTB. Recently improvements in harvest techniques allow the surgeon to reliably yield a robust volume of QT graft without hampering the quadriceps strength and lesser donor-site morbidity [3, 8, 13, 30, 31]. The finding of this meta-analysis is quite promising for surgeons who are dealing with revision ACL reconstruction and are not sure about graft choice. To the best of the authors’ knowledge, this is the first systematic review and meta-analysis on revision ACL reconstruction using QT autograft.
The present study has some limitations. Revision ACL reconstruction is a less frequently performed procedure than primary reconstruction. Therefore, the authors were limited in the current study by the paucity of studies with high levels of evidence. The available studies were mostly retrospective with limited sample sizes and there was only one prospective comparative study available on revision ACL surgery comparing quadriceps and hamstring tendon grafts. Further hurdles were the non-uniformity of the techniques used heterogeneous nature of the tools and scores used for reporting outcomes. High-quality randomized controlled trials or large cohort prospective studies with homogeneous populations, especially regarding surgical techniques and outcome scores, could provide better evidence for the use of QT autograft for revision ACL reconstruction.
The clinical relevance of the present study lies in the fact that the QT autograft is the least studied and least used graft compared to other grafts, especially for revision ACL reconstruction. Many surgeons do not even consider the QT as a possible graft option when discussing with the patients. However, it is a very suitable and versatile graft option for revision ACL reconstruction with distinct advantages. The contribution of this study to the existing literature is meaningful as it delineates the deficiencies in current literature and shows that QT grafts are a viable graft choice in primary and revision situations.
Conclusion
The QT autograft was associated with an improved trend of rotatory laxity, PROMs, and failure rate compared to HT autograft after revision ACL reconstruction. The QT autograft for revision ACL reconstruction is supported by the current literature. It is a viable graft that should be considered for both primary and revision ACL reconstruction.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Erickson BJ, Cvetanovich GL, Frank RM, Riff AJ, Bach BR (2017) Revision ACL reconstruction: a critical analysis review. JBJS Rev 5:e1–e1
Longo UG, Nagai K, Salvatore G, Cella E, Candela V, Cappelli F, Ciccozzi M, Denaro V (2021) Epidemiology of anterior cruciate ligament reconstruction surgery in italy: a 15-year nationwide registry study. J Clin Med 10:223. https://doi.org/10.3390/jcm10020223
Meena A, Farinelli L, Hoser C, Abermann E, Raj A, Hepperger C, Herbort M, Fink C (2022) Revision ACL reconstruction using quadriceps, hamstring and patellar tendon autografts leads to similar functional outcomes but hamstring graft has a higher tendency of graft failure. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07200-2
D’Ambrosi R, Meena A, Raj A, Ursino N, Formica M, Herbort M, Fink C (2022) Multiple revision anterior cruciate ligament reconstruction: not the best but still good. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07197-8
Hunnicutt JL, Haynes WB, Slone HS, Prince JA, Boden SA, Xerogeanes JW (2021) Revision anterior cruciate ligament reconstruction with the all-soft tissue quadriceps tendon autograft has acceptable early and intermediate-term outcomes. Arthroscopy 37:2848–2857
Grassi A, Ardern CL, Marcheggiani Muccioli GM, Neri MP, Marcacci M, Zaffagnini S (2016) Does revision ACL reconstruction measure up to primary surgery? A meta-analysis comparing patient-reported and clinician-reported outcomes, and radiographic results. Br J Sports Med 50:716–724
Vap AR, Persson A, Fenstad AM, Moatshe G, LaPrade RF, Engebretsen L (2019) Re-revision anterior cruciate ligament reconstruction: an evaluation from the norwegian knee ligament registry. Arthroscopy 35:1695–1701
Lind M, Strauss MJ, Nielsen T, Engebretsen L (2021) Low surgical routine increases revision rates after quadriceps tendon autograft for anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Registry. Knee Surg Sports Traumatol Arthrosc 29:1880–1886
Häner M, Bierke S, Petersen W (2016) Anterior cruciate ligament revision surgery: ipsilateral quadriceps versus contralateral semitendinosus-gracilis autografts. Arthroscopy 32:2308–2317
Belk JW, Kraeutler MJ, Marshall HA, Goodrich JA, McCarty EC (2018) Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction: a systematic review of comparative studies with minimum 2-year follow-up. Arthroscopy 34:1699–1707
Siegel L, Vandenakker-Albanese C, Siegel D (2012) Anterior cruciate ligament injuries: anatomy, physiology, biomechanics, and management. Clin J Sport Med 22:349–355
Shani RH, Umpierez E, Nasert M, Hiza EA, Xerogeanes J (2016) Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthroscopy 32:71–75
Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E (2019) Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon–bone and hamstring-tendon autografts. Am J Sports Med 47:3531–3540
Lind M, Nielsen TG, Soerensen OG, Mygind-Klavsen B, Faunø P (2020) Quadriceps tendon grafts does not cause patients to have inferior subjective outcome after anterior cruciate ligament (ACL) reconstruction than do hamstring grafts: a 2-year prospective randomised controlled trial. Br J Sports Med 54:183–187
Barié A, Ehmann Y, Jaber A, Huber J, Streich NA (2019) Revision ACL reconstruction using quadriceps or hamstring autografts leads to similar results after 4 years: good objective stability but low rate of return to pre-injury sport level. Knee Surg Sports Traumatol Arthrosc 27:3527–3535
Eggeling L, Breer S, Drenck TC, Frosch K-H, Akoto R (2021) Double-layered quadriceps tendon autografts provide lower failure rates and improved clinical results compared with hamstring tendon grafts in Revision ACL reconstruction. Orthop J Sports Med 9:232596712110469
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Garofalo R, Djahangiri A, Siegrist O (2006) Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy 22:205–214
Supreeth S, Ghanami SA, Riyami MA, Habsi SA, Murthi PS, Kalbani WA, Saqri HA, Haddad SN, Abdelmasih SR (2022) Revision anterior cruciate ligament reconstruction and outcomes with different autografts in a population with kneeling customs. Musculoskelet Surg. https://doi.org/10.1007/s12306-022-00739-w
Noyes FR, Barber-Westin SD (2006) Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am J Sports Med 34:553–564
Cavaignac E, Coulin B, Tscholl P, Nik Mohd Fatmy N, Duthon V, Menetrey J (2017) Is Quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am J Sports Med 45:1326–1332
Runer A, Csapo R, Hepperger C, Herbort M, Hoser C, Fink C (2020) Anterior cruciate ligament reconstructions with quadriceps tendon autograft result in lower graft rupture rates but similar patient-reported outcomes as compared with hamstring tendon autograft: a comparison of 875 patients. Am J Sports Med 48:2195–2204
Runer A, Wierer G, Herbst E, Hepperger C, Herbort M, Gföller P, Hoser C, Fink C (2018) There is no difference between quadriceps- and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee Surg Sports Traumatol Arthrosc 26:605–614
Nyland J, Collis P, Huffstutler A, Sachdeva S, Spears JR, Greene J, Caborn DNM (2020) Quadriceps tendon autograft ACL reconstruction has less pivot shift laxity and lower failure rates than hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 28:509–518
The MARS Group, Wright RW, Huston LJ, Haas AK, Spindler KP, Nwosu SK, Allen CR (2014) Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the multicenter ACL revision study (MARS) cohort. Am J Sports Med 42:2301–2310
Diermeier T, Tisherman R, Hughes J, Tulman M, Baum Coffey E, Fink C, Lynch A, Fu FH, Musahl V (2020) Quadriceps tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 28:2644–2656
D’Ambrosi R, Meena A, Raj A, Ursino N, Hewett TE (2022) Anterior knee pain: state of the art. Sports Med - Open 8:98. https://doi.org/10.1186/s40798-022-00488-x
Sheean AJ, Musahl V, Slone HS, Xerogeanes JW, Milinkovic D, Fink C, Hoser C (2018) Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: use it now, use it often. Br J Sports Med 52:698–701
Meena A, D’Ambrosi R, Runer A, Raj A, Attri M, Abermann E, Hoser C, Fink C (2022) Quadriceps tendon autograft with or without bone block have comparable clinical outcomes, complications and revision rate for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07281-z
Winkler PW, Vivacqua T, Thomassen S, Lovse L, Lesniak BP, Getgood AMJ, Musahl V (2022) Quadriceps tendon autograft is becoming increasingly popular in revision ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 30:149–160
Funding
Open access funding provided by UMIT TIROL-Private Universität für Gesundheitswissenschaften und -technologie GmbH.
Author information
Authors and Affiliations
Contributions
Conceptualization, AM, SDP, AG, ST, SZ, and CF; methodology, AM, SDP, AG, AR, LF, CH, ST, SZ, and CF; data curation and synthesis, AM, SDP, AG, AR, LF, CH, ST, SZ, and CF; writing—original draft preparation, AM, SDP, AG, AR, LF, CH, ST, SZ, and CF; writing—review and editing, AM, SDP, AG, AR, LF, CH, ST, SZ, and CF; supervision, CH, ST, SZ, and CF; all authors interpreted the data, critically reviewed the work, made important contributions to the manuscript with their suggestions for improvement, approved the published version, and agreed to be responsible for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest related to this study.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meena, A., Di Paolo, S., Grassi, A. et al. No difference in patient reported outcomes, laxity, and failure rate after revision ACL reconstruction with quadriceps tendon compared to hamstring tendon graft: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 31, 3316–3329 (2023). https://doi.org/10.1007/s00167-023-07380-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07380-5