Abstract
Purpose
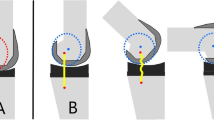
The purpose of this study is to determine whether the flexion first balancing technique, developed in an attempt to solve the dissatisfaction due to instability in total knee arthroplasties, leads to better restoration of joint line height and medial posterior condylar offset. This might result in better knee flexion, compared to the classic extension first gap balancing technique. The secondary objective is to show non-inferiority of the flexion first balancing technique in terms of clinical outcomes as measured by the Patient Reported Outcome Measurements.
Methods
A cohort of 40 patients (46 knee replacements) operated using the flexion first balancing technique was retrospectively analyzed and compared with a cohort of 51 patients (52 knee replacements) operated using the classic gap balancing technique. Radiographic analysis of the coronal alignment, joint line height and posterior condylar offset was performed. Clinical and functional outcome data were analyzed pre- and postoperatively and compared between both groups. The two sample t test, Mann–Whitney U test, Chi-square test and a linear mixed model were used for performing statistical analyses, after normality analyses were executed.
Results
Radiologic evaluation showed a decrease in posterior condylar offset using the classic gap balancing technique (p = 0.040) versus no change using the flexion first balancing technique (p = n.s.). No statistically significant differences were noted for joint line height and coronal alignment. Using the flexion first balancer technique leads to a greater postoperative range of motion with deeper flexion (p = 0.002) and a better Knee injury and Osteoarthritis Outcome Score (KOOS) (p = 0.025).
Conclusion
The Flexion First Balancing technique is a valid and safe technique for TKA, resulting in better preservation of PCO with consequently greater postoperative flexion and better KOOS scores.
Level of evidence
III.




Similar content being viewed by others
Abbreviations
- TKA:
-
Total knee arthroplasty
- ROM:
-
Range of motion
- PCO:
-
Posterior condylar offset
- MCL:
-
Medial collateral ligament
- FFB:
-
Flexion First Balancing
- PROMs:
-
Patient Reported Outcome Measurements
- GAP:
-
Classic extension first gap balancing
- VAS:
-
Visual Analogue Scale
- OKS:
-
Oxford Knee score
- KOOS-PS:
-
Knee injury and Osteoarthritis Outcome Score-Physical Function Short Form
- EQ-5D:
-
EuroQol-5D
- JLH:
-
Joint line height
- (c)ATJL:
-
(Corrected) adductor tubercle joint line distance
- (c)PCO:
-
(Corrected) posterior condylar offset
- PCL:
-
Posterior cruciate ligament
- n.s.:
-
Not significant
- HKA:
-
Hip-knee-ankle
- CWF:
-
Coronal femoral width
- LFW:
-
Lateral femoral width
References
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84:50–53
Chang MJ, Kang SB, Chang CB, Han DH, Park HJ, Hwang K et al (2020) Posterior condylar offset changes and its effect on clinical outcomes after posterior-substituting, fixed-bearing total knee arthroplasty: anterior versus posterior referencing. Knee Surg Relat Res 32:10
Christensen JC, Blackburn B, Browning B, Wilbur C, Trinity JD, Gililland JM et al (2022) Patient-reported outcomes measurement information system physical function and knee injury and osteoarthritis outcome score relationship on performance measures in people undergoing total knee arthroplasty. Disabil Rehabil. https://doi.org/10.1080/09638288.2022.21349341-9
Churchill JL, Khlopas A, Sultan AA, Harwin SF, Mont MA (2018) Gap-balancing versus measured resection technique in total knee arthroplasty: a comparison study. J Knee Surg 31:13–16
Freisinger GM, Hutter EE, Lewis J, Granger JF, Glassman AH, Beal MD et al (2017) Relationships between varus-valgus laxity of the severely osteoarthritic knee and gait, instability, clinical performance, and function. J Orthop Res 35:1644–1652
Goutham GDV, Jain VK, Sinha S, Arya RK (2020) Effect of posterior condylar offset in post operative range of motion in cruciate retaining and sacrificing TKR: a comparative analysis. J Orthop 20:342–346
Han HS, Kang SB (2018) Interactive effect of femoral posterior condylar offset and tibial posterior slope on knee flexion in posterior cruciate ligament-substituting total knee arthroplasty. Knee 25:335–340
Hasebe Y, Akasaka K, Yamamoto M (2021) Factors affecting early knee-flexion range of motion after total knee arthroplasty. J Phys Ther Sci 33:672–675
Kamenaga T, Hiranaka T, Okimura K, Fujishiro T, Okamoto K (2022) Contralateral knee flexion predicts postoperative knee flexion in unilateral total knee arthroplasty: a retrospective study. Orthop Traumatol Surg Res: OTSR 108:103218
Keenan OJF, Holland G, Maempel JF, Keating JF, Scott CEH (2020) Correlations between radiological classification systems and confirmed cartilage loss in severe knee osteoarthritis. Bone Joint J. 102-b:301–309
Koshire S, Mohanty SS, Keny SA, Rai AK, Rathod TN, Kamble P (2022) The influence of joint line restoration on functional outcome after primary total knee arthroplasty: a prospective study. J Clin Orthop Trauma 34:102023
Kwak DS, Kim YD, Cho N, In Y, Kim MS, Lim D et al (2022) Restoration of the joint line configuration reproduces native mid-flexion biomechanics after total knee arthroplasty: a matched-pair cadaveric study. Bioengineering 17:9
Longo UG, Candela V, Pirato F, Hirschmann MT, Becker R, Denaro V (2021) Midflexion instability in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 29:370–380
Luyckx T, Vandenneucker H, Ing LS, Vereecke E, Ing AV, Victor J (2018) Raising the Joint Line in TKA is associated with mid-flexion laxity: a study in cadaver knees. Clin Orthop 476:601–611
Matziolis G, Brodt S, Windisch C, Roehner E (2017) Changes of posterior condylar offset results in midflexion instability in single-radius total knee arthroplasty. Arch Orthop Trauma Surg 137:713–717
Popat R, Albelooshi A, Mahapatra P, Bollars P, Ettinger M, Jennings S et al (2022) Improved joint line and posterior offset restoration in primary total knee replacement using a robotic-assisted surgical technique: an international multi-centre retrospective analysis of matched cohorts. PLoS ONE 17:e0272722
Ramkumar PN, Navarro SM, Haeberle HS, Ng M, Piuzzi NS, Spindler KP (2018) No difference in outcomes 12 and 24 months after lower extremity total joint arthroplasty: a systematic review and meta-analysis. J Arthroplasty 33:2322–2329
Stambough JB, Edwards PK, Mannen EM, Barnes CL, Mears SC (2019) Flexion instability after total knee arthroplasty. J Am Acad Orthop Surg 27:642–651
Tapasvi SR, Shekhar A, Patil SS, Dipane MV, Chowdhry M, McPherson EJ (2020) Comparison of gap balancing vs measured resection technique in patients undergoing simultaneous bilateral total knee arthroplasty: one technique per knee. J Arthroplasty 35:732–740
Vajapey SP, Pettit RJ, Li M, Chen AF, Spitzer AI, Glassman AH (2020) Risk factors for mid-flexion instability after total knee arthroplasty: a systematic review. J Arthroplasty 35:3046–3054
van Lieshout WAM, Duijnisveld BJ, Koenraadt KLM, Elmans L, Kerkhoffs G, van Geenen RCI (2019) Adequate joint line restoration and good preliminary clinical outcomes after total knee arthroplasty using the Flexion First Balancer technique. Knee 26:794–802
van Lieshout WAM, Koenraadt KLM, Elmans L, van Geenen RCI (2020) Flexion First Balancer: description of new technique in TKA to reproduce joint line and pre-disease mechanical alignment. J Exp Orthop 7:23
van Lieshout WAM, van Oost I, Koenraadt KLM, Elmans L, van Geenen RCI (2021) The effect of restored medial knee anatomy in total knee arthroplasty with the flexion first balancer technique on mid-flexion laxity and functional outcome. BMC Musculoskelet Disord 22:1029
Williams HA, Webster J, Teeter MG, Howard JL, Somerville LE, Lanting BA (2021) The impact of a gap balancing or measured resection surgical technique on posterior condylar offset and patient-reported outcome measures. Arthroplast Today 11:64–67
Yang G, Chen W, Chen W, Sun X, Zhou D, Chen S et al (2016) Full-thickness cartilage-based posterior femoral condylar offset. Influence on knee flexion after posterior-stabilized total knee arthroplasty. Orthop Traumatol Surg Res: OTSR 102:441–446
Zhang Y, Wang J, Zhang M, Xu Y (2021) Effect of femoral posterior condyle offset on knee joint function after total knee replacement: a network meta-analysis and a sequential retrospective cohort study. J Orthop Surg Res 16:126
Acknowledgements
None.
Funding
Belgian Society of Orthopedics & Traumatology (BVOT) research grant.
Author information
Authors and Affiliations
Contributions
ASVDK collected the pre- and postoperative data and drafted the manuscript. BV performed the total knee arthroplasties and participated in the design and content of the manuscript. JDS performed the total knee arthroplasties as well and reviewed the final manuscript. The statistical cell of the University of Hasselt conducted the statistical analyses. KDM and JV reviewed the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not necessary as retrospective study design.
Informed consent
Not necessary as retrospective study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Van de Kelft, AS., De Mulder, K., De Schepper, J. et al. Balancing the flexion gap first in total knee arthroplasty leads to better preservation of posterior condylar offset resulting in better knee flexion. Knee Surg Sports Traumatol Arthrosc 31, 3792–3798 (2023). https://doi.org/10.1007/s00167-023-07346-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07346-7