Abstract
Purpose
This study was aimed to compare the clinical, functional, and radiographic outcomes between symmetric and asymmetric extension and mediolateral gap balance after navigation-assisted (NA) total knee arthroplasty (TKA) using ultracongruent (UC) insets and the medial stabilising technique (MST).
Methods
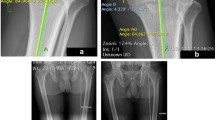
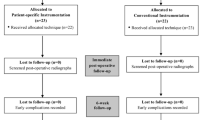
In all, 363 knees of 275 patients who underwent mechanical alignment-target NA TKA with MST between January 2015 and December 2017 were analysed. Patients were divided into balanced (extension mediolateral gap difference ≤ 2 mm) and tight medial (difference ≥ 3 mm) groups. Pre- and postoperative clinical, functional (range of motion, Western Ontario and McMaster University Osteoarthritis [WOMAC] index, Knee Society Knee Score [KSKS], and Knee Society Function Score [KSFS]) and radiographic (hip–knee–ankle [HKA] angle, femoral condylar offset, extension angle [a minus indicates hyperextension], and joint line distance) outcomes were compared between the groups. Student’s t- or Chi-squared test was used to compare the outcomes.
Results
Among the 363 knees analysed, 279 (77%) were assigned to the balanced group and 84 (23%) to the tight medial group. The preoperative HKA angle was significantly greater in the tight medial group than in the balanced group (9.7° ± 4.1° vs 14.3° ± 4.7°, P < 0.001). The postoperative WOMAC index, KSKS, and KSFS were similar between the groups. The change in the joint line distance was not significantly different (1.5 ± 3.7 vs 2.0 ± 3.3; n.s).
Conclusion
The clinical, functional, and radiographic outcomes, including joint line distance, were comparable between the tight medial and balanced group after mechanical alignment-targeted UC TKA with MST.
Level of evidence
Level III, retrospective comparative study.







Similar content being viewed by others
Data availability statement
The data that support the finding of this study are available from the corresponding author, upon reasonable request.
References
An VVG, Twiggs J, Leie M, Fritsch BA (2019) Kinematic alignment is bone and soft tissue preserving compared to mechanical alignment in total knee arthroplasty. Knee 26:466–476
Azukizawa M, Kuriyama S, Nakamura S, Nishitani K, Lyman S, Morita Y et al (2018) Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Arch Orthop Trauma Surg 138:1143–1150
Becker R, Baker K, Hommel H, Bernard M, Kopf S (2019) No correlation between rotation of femoral components in the transverse plane and clinical outcome after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27:1456–1462
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Choi BS, Kim JM, Han HS (2022) Decision-making factors and their thresholds for total knee arthroplasty in lateral tibiofemoral osteoarthritis patients: a retrospective cohort study. Knee Surg Relat Res 34:41
Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ (2018) What is the minimum clinically important difference for the WOMAC index after TKA? Clin Orthop Relat Res 476:2005–2014
Graichen H, Lekkreusuwan K, Eller K, Grau T, Hirschmann MT, Scior W (2022) A single type of varus knee does not exist: morphotyping and gap analysis in varus OA. Knee Surg Sports Traumatol Arthrosc 30:2600–2608
Herschmiller T, Grosso MJ, Cunn GJ, Murtaugh TS, Gardner TR, Geller JA (2018) Step-wise medial collateral ligament needle puncturing in extension leads to a safe and predictable reduction in medial compartment pressure during TKA. Knee Surg Sports Traumatol Arthrosc 26:1759–1766
Hess S, Moser LB, Robertson EL, Behrend H, Amsler F, Iordache E et al (2022) Osteoarthritic and non-osteoarthritic patients show comparable coronal knee joint line orientations in a cross-sectional study based on 3D reconstructed CT images. Knee Surg Sports Traumatol Arthrosc 30:407–418
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Ishibashi K, Sasaki E, Sasaki S, Kimura Y, Yamamoto Y, Ishibashi Y (2020) Medial stabilizing technique preserves anatomical joint line and increases range of motion compared with the gap-balancing technique in navigated total knee arthroplasty. Knee 27:558–564
Kim CW, Lee CR, Gwak HC, Kim JH, Kwon YU, Kim DY (2020) The Effects of surgical technique in total knee arthroplasty for Varus osteoarthritic knee on the rotational alignment of femoral component: gap balancing technique versus measured resection technique. J Knee Surg 33:144–151
Kim JS, Cho CH, Lee MC, Han HS (2021) Risk factors of de novo hyperextension developed after posterior cruciate ligament substituting total knee arthroplasty: a matched case-control study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06618-4
Lee HJ, Kim SH, Park YB (2020) Selective medial release using multiple needle puncturing with a spacer block in situ for correcting severe varus deformity during total knee arthroplasty. Arch Orthop Trauma Surg 140:1523–1531
Lee KJ, Moon JY, Song EK, Lim HA, Seon JK (2012) Minimum two-year results of revision total knee arthroplasty following infectious or non-infectious causes. Knee Surg Relat Res 24:227–234
Lee SS, Kim JH, Heo JW, Moon YW (2019) Gradual change in knee extension following total knee arthroplasty using ultracongruent inserts. Knee 26:905–913
Lee SY, Yang JH, Lee YI, Yoon JR (2016) A novel medial soft tissue release method for Varus deformity during total knee arthroplasty: femoral origin release of the medial collateral ligament. Knee Surg Relat Res 28:153–160
Liu DW, Martinez Martos S, Dai Y, Beller EM (2022) The femoral intercondylar notch is an accurate landmark for the resection depth of the distal femur in total knee arthroplasty. Knee Surg Relat Res 34:32
Migliorini F, Eschweiler J, Mansy YE, Quack V, Schenker H, Tingart M et al (2020) Gap balancing versus measured resection for primary total knee arthroplasty: a meta-analysis study. Arch Orthop Trauma Surg 140:1245–1253
Miralles-Munoz FA, Gonzalez-Parreno S, Martinez-Mendez D, Gonzalez-Navarro B, Ruiz-Lozano M, Lizaur-Utrilla A et al (2022) A validated outcome categorization of the knee society score for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30:1266–1272
Moorthy V, Lai MC, Liow MHL, Chen JY, Pang HN, Chia SL et al (2021) Similar postoperative outcomes after total knee arthroplasty with measured resection and gap balancing techniques using a contemporary knee system: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 29:3178–3185
Nagai K, Muratsu H, Kanda Y, Tsubosaka M, Kamenaga T, Miya H et al (2018) Intraoperative soft tissue balance using novel medial preserving gap technique in posterior-stabilized total knee arthroplasty: comparison to measured resection technique. Knee Surg Sports Traumatol Arthrosc 26:3474–3481
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-Uchi H, Hamai S et al (2014) Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3174–3180
Okamoto Y, Nakajima M, Jotoku T, Otsuki S, Neo M (2016) Capsular release around the intercondylar notch increases the extension gap in posterior-stabilized rotating-platform total knee arthroplasty. Knee 23:730–735
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M et al (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Pawar P, Naik L, Sahu D, Bagaria V (2021) Comparative study of pinless navigation system versus conventional instrumentation in total knee arthroplasty. Clin Orthop Surg 13:358–365
Piovan G, Farinelli L, Screpis D, Iacono V, Povegliano L, Bonomo M et al (2022) Distal femoral osteotomy versus lateral unicompartmental arthroplasty for isolated lateral tibiofemoral osteoarthritis with intra-articular and extra-articular deformity: a propensity score-matched analysis. Knee Surg Relat Res 34:34
Ramappa M (2015) Midflexion instability in primary total knee replacement: a review. SICOT J 1:24
Rossi R, Cottino U, Bruzzone M, Dettoni F, Bonasia DE, Rosso F (2019) Total knee arthroplasty in the varus knee: tips and tricks. Int Orthop 43:151–158
Schelker BL, Moret CS, von Eisenhart-Rothe R, Graichen H, Arnold MP, Leclercq V et al (2022) The impact of different alignment strategies on bone cuts for neutral knee phenotypes in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07209-7
Sekiya H, Takatoku K, Takada H, Sasanuma H, Sugimoto N (2009) Postoperative lateral ligamentous laxity diminishes with time after TKA in the varus knee. Clin Orthop Relat Res 467:1582–1586
Shon OJ, Kim GB (2022) Does the degree of intraoperatively identified cartilage loss affect the outcomes of primary total knee arthroplasty without patella resurfacing? A prospective comparative cohort study. Knee Surg Relat Res 34:36
Sim JA, Na YG, Go JY, Lee BK (2018) Clinical and radiologic evaluation of medial epicondylar osteotomy for varus total knee arthroplasty. Knee 25:177–184
Song EK, Agrawal PR, Kim SK, Seo HY, Seon JK (2016) A randomized controlled clinical and radiological trial about outcomes of navigation-assisted TKA compared to conventional TKA: long-term follow-up. Knee Surg Sports Traumatol Arthrosc 24:3381–3386
Toyooka S, Masuda H, Nishihara N, Miyamoto W, Kobayashi T, Kawano H et al (2022) Assessing the role of minimal medial tissue release during navigation-assisted Varus total knee arthroplasty based on the degree of preoperative Varus deformity. J Knee Surg 35:1236–1241
Tsubosaka M, Muratsu H, Nakano N, Kamenaga T, Kuroda Y, Inokuchi T et al (2021) Knee stability following posterior-stabilized total knee arthroplasty: comparison of medial preserving gap technique and measured resection technique. J Knee Surg. https://doi.org/10.1055/s-0041-1729968
Tsukeoka T, Tsuneizumi Y (2019) Residual medial tightness in extension is corrected spontaneously after total knee arthroplasty in varus knees. Knee Surg Sports Traumatol Arthrosc 27:692–697
Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H et al (2017) Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee 24:1478–1484
Ueyama H, Kanemoto N, Minoda Y, Nakagawa S, Taniguchi Y, Nakamura H (2022) Association of a wider medial gap (medial laxity) in flexion with self-reported knee instability after medial-pivot total knee arthroplasty. J Bone Joint Surg Am 104:910–918
Zambianchi F, Bazzan G, Marcovigi A, Pavesi M, Illuminati A, Ensini A et al (2021) Joint line is restored in robotic-arm-assisted total knee arthroplasty performed with a tibia-based functional alignment. Arch Orthop Trauma Surg 141:2175–2184
Zambianchi F, Giorgini A, Ensini A, Lombari V, Daffara V, Catani F (2021) Navigated, soft tissue-guided total knee arthroplasty restores the distal femoral joint line orientation in a modified mechanically aligned technique. Knee Surg Sports Traumatol Arthrosc 29:966–974
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The protocol used to evaluate radiographic findings and intraoperative navigation data was approved by our institution’s investigational review board (SMC2022-11-045).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, SS., Lee, J., Alharthi, H. et al. Effect of mediolateral gap difference on postoperative outcomes in navigation-assisted total knee arthroplasty using an ultracongruent insert and the medial stabilising technique. Knee Surg Sports Traumatol Arthrosc 31, 3745–3754 (2023). https://doi.org/10.1007/s00167-023-07324-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07324-z