Abstract
Purpose
To characterise patients who had returned to their pre-injury physical activity (PA) or higher at 18 months and maintained that level of PA 3–5 years after the primary ACL reconstruction and to describe the level, frequency, and type of PA participation during the first 5 years after ACL reconstruction
Method
Data, from follow-ups at 18 months and 3–5 years after an ACL reconstruction, were extracted from a rehabilitation-specific register. Patients, 15–65 years of age, were included. The data comprised patient-reported outcomes and the results from two questions with respect to the level, frequency, and type of PA. Comparisons were made between patients who had and had not maintained their pre-injury level of PA at the follow-up 3–5 years after an ACL reconstruction.
Results
A total of 272 patients met the inclusion criteria. The mean follow-up time was 3.8 years (min–max: 2.9–5.1) after the ACL reconstruction. Of patients who had returned to their pre-injury or a higher level of PA at the 18 month follow-up (n = 114), 68% (n = 78) maintained that level at the 3- to 5-year follow-up after ACL reconstruction. These patients reported a higher level of psychological readiness to return to sport (98 versus 79; p = 0.013). Moreover, these patients were 6.0 years older (p = 0.016) and were characterised by male sex (56% versus 44%; p = 0.028) and a lower level of pre-injury PA (p = 0.013). At the follow-up 3–5 years after the ACL reconstruction, more than 90% met the recommendations for PA. However, the prevalence of physical inactivity had increased and the involvement in organised PA had decreased compared with the 18-month follow-up.
Conclusions
Two out of three patients who have returned to their previous level of PA at 18 months can be expected to maintain that level, 3–5 years following ACL reconstruction. These patients were mainly characterised by a higher level of psychological readiness, especially in patients who participated in knee-strenuous sport and were younger than 20 years of age. The results of this study suggest that patients become more physically inactive over time, implicating the importance of clinicians helping patients find a suitable PA that may help patients maintain an active lifestyle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Physical activity (PA) is one of the most important factors when it comes to preventing and managing non-communicable diseases, such as cardiovascular diseases, cancer, and diabetes [10, 34]. According to the World Health Organisation’s (WHO) guidelines on PA and sedentary behaviour from 2020, all adults (18–64 years of age) should participate in at least 150–300 min of moderate-intensity aerobic PA weekly; or 75–150 min of vigorous-intensity aerobic PA; or an equivalent combination of moderate- and vigorous-intensity activity [10]. For additional health benefits, adults and adolescents are also recommended to perform “muscle strengthening activities at moderate or greater intensity that involve all the major muscle groups on two or more days a week” [10].
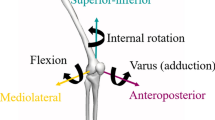
A severe knee injury, such as an injury to the anterior cruciate ligament (ACL), often entails a period of reduced frequency and intensity of PA and a change in the type of PA [15]. Historically, ACL injury research has mainly focused on aspects of returning patients to sport, which has also been used as an outcome of successful treatment [1]. However, only about 50% of patients with an ACL reconstruction return to competitive sport and about two-thirds return to their pre-injury level of sport within the first 7 years after the reconstruction [2, 3]. Patients who succeed in returning to sport after an ACL reconstruction have been characterised by lower levels of fear of re-injury [27], higher self-efficacy of knee function [6, 18], greater motivation to return to sport [4, 5, 13], and higher levels of psychological readiness to return to sport [37]. In the light of self-reported knee function, patients who return to sport reporting less impairment during sport and recreation and higher levels of knee-related quality of life (QoL) [14, 18]. Ithurburn et al. [19] reported no differences in self-reported knee function between patients who had returned to pre-injury sport and had maintained versus not maintained that level of sport 1 year after the return. However, it is not known whether there are differences in psychological factors between these patients.
Regardless of whether or not a patient returns to sport, it is of great importance to maintain any PA to minimise the risks of non-communicable diseases [34]. Specifically, the risk of developing radiographic signs of osteoarthritis (OA) is increased in patients after an ACL reconstruction [17, 25]. Exercises therapy, including strength training of the knee extensors muscles, is recommended as muscular weaknesses of the knee extensors have been associated with an increased risk of developing symptoms of knee osteoarthritis [28]. In patients who have developed OA, exercise therapy is strongly recommended. Therefore, to achieve the recommended levels of PA is a minimum level of PA for patients who develop OA after an ACL reconstruction [26]. Although previous studies [7, 20, 22] have assessed the level of PA from a long-term perspective, a few studies have investigated the frequency of PA in patients after ACL reconstruction. To better understand PA habits, there is a need for a more detailed description of the level, frequency, and type of PA in a time when most patients have completed their rehabilitation after an ACL reconstruction.
The aim of this study was to 1) characterise patients who had returned to their pre-injury PA or higher at 18 months and had maintained that level of PA at a follow-up between 3 and 5 years after the primary ACL reconstruction, and 2) describe the level, frequency, and type of PA participation during the first years after completion of the rehabilitation. The null-hypothesis was that there would be no differences in psychological factors or self-reported knee function between patients who maintained and did not maintain PA 3–5 years after the primary ACL reconstruction.
Materials and methods
Ethical approval was obtained from the Swedish Ethical Review Authority (registration numbers: 2020–02501) and the study was conducted according to the World Medical Association Declaration of Helsinki. The data were extracted on June 14, 2021.This study, based on prospectively collected data from a rehabilitation-outcome register, Project ACL, was designed following the recommendation of the STROBE statement [33]. Project ACL consists of over 3000 patients with an ACL injury with outcome data from patient-reported outcomes (PROs) and tests of muscle function (strength tests and hop tests). Evaluations are scheduled at predefined follow-ups (10 weeks, 4, 8, 12, 18 months and yearly up to 5 years and every fifth year thereafter), starting with the ACL injury or reconstruction as baseline. All the patients included in the register were given written information about the study and informed consent was obtained. All patients can withdraw from participation at any time, without any further explanation.
Eligibility criteria
Patients registered in Project ACL with at least an 18-month follow-up after the primary ACL reconstruction were assessed for eligibility. The 18 months follow-up was chosen as it corresponds to a time when most patients have completed their rehabilitation after an ACL reconstruction [24]. The following inclusion criteria were used; a primary ACL reconstruction between January 2013 and September 2017, 15 to 65 years of age at the primary ACL reconstruction and at least one follow-up at 3, 4 or 5 years after the ACL reconstruction. Patients were excluded if they reported a new ACL injury since their last follow-up or another injury or illness (e.g., ankle sprain, post COVID-19 condition, or sciatica) that might affect their ability to be physically active at the 3- to 5-year follow-up.
Return to physical activity
A modified version of the Tegner Activity Scale (Tegner) [6, 32] was used to assess the level of PA pre-injury, at 18 months and at 3–5 years after the ACL reconstruction. The Tegner is graded from 1 to 10, with 1 representing the least strenuous knee activity and 10 representing the most strenuous knee activity, such as rugby and international football. The Tegner has been reported to have acceptable test–retest reliability, with an ICC of 0.8 for patients with an ACL injury or reconstruction [8]. The modified version does not contain the “0” score, which represents “sick leave or disability pension because of knee problems” in the original version. Furthermore, the modified version of the Tegner has recreational sports activities as a choice up to level 9.
Patients who reported the same or higher Tegner at the 18-month follow-up compared with the pre-injury score were defined as having returned to their pre-injury level of PA. Based on the reported Tegner at the 3- to 5-year follow-up, the included patients were divided into the following groups: 1) same or higher PA level compared with pre-injury level (same or higher) and 2) lower PA level than the pre-injury level (lower). For the primary aim of the study, only eligible patients who had returned to their pre-injury level of PA at 18 months after ACL reconstruction were included. Patients are continuously included in Project ACL regardless of the time that has passed since the ACL injury or reconstruction. As a result, some patients only had Tegner data from the 18-month and the 3-year follow-ups, while other patients had data from all follow-ups. Moreover, in September 2020, the 4-year follow-up was excluded from the standard schedule of follow-ups. For patients who had data from more than one of the follow-ups 3–5 years after the ACL reconstruction, data from the latest follow-up were included for the main analysis.
Study outcomes
The Knee injury and Osteoarthritis Outcome Score (KOOS) [29, 30] was used to evaluate the patients’ opinions of their knee and associated problems during the previous week. The scale comprises 42 items in five subscales including pain, other symptoms, activities of daily living, function in sport, and recreation and knee-related QoL. Standardised answer options are given, and each question is assigned a score from 0 to 4. Each subscale score is calculated independently, by dividing the mean score for each subscale by 4 and then multiplying the result by 100 (100 indicates no problem and 0 indicates extreme problems). The KOOS has been reported to have acceptable test–retest reliability for patients with a knee injury (ICC = 0.85–0.93) [30]. In Project ACL, the subscale of activities of daily living is only completed preoperatively and at yearly follow-ups. As a result, the subscale of activities of daily living, at the 18-month follow-up, was excluded in this study.
A modified version of the Knee Self-Efficacy Scale (K-SES18) was used to assess patients’ knee-related self-efficacy [6]. The K-SES18 consists of two subscales, present knee self-efficacy and future knee self-efficacy. Patients rate each item on an 11-point Likert scale, ranging from 0 = not at all certain to 10 = very certain. The mean value of each subscale was used for further analysis. The K-SES18 has been reported to have acceptable reliability and validity to assess knee self-efficacy in patients, 16–50 years of age, after an ACL injury or reconstruction [6].
The Swedish version of the ACL Return to Sport after Injury Scale (ACL-RSI) [23, 36] was used to assess psychological readiness to return to sports participation 18 months after ACL reconstruction. The Swedish version consists of 12 items and has been reported to be valid, internally consistent, and reliable after ACL reconstruction (ICC = 0.89) [23]. Patients rate each item on a 10-point Likert scale. The total score for all 12 items on the ACL-RSI was used for further analysis.
Two single questions were used to assess the type of PA/sport pre-injury at 18 months and 3, 4 and 5 years after the ACL reconstruction: 1) Have you participated in any PA/sport during the last month? If “yes”, enter the main PA/sport and 2) At which level have you participated in PA or sport? Question 1 was an open-ended question and Question 2 had the following fixed-alternative responses:
-
Physically inactive (less than 30 min of PA/day or less than 150 min/week)
-
Physically active (more than 30 min of PA/day or more than 150 min/week)
-
Exercising (up to 2 days/week of regular exercising)
-
Active exercising (regular exercising 3–7 days/week without regularly participating in competition)
-
Active competition (regular exercising 3–7 days/week with regular participation in competition)
-
Elite (division 2–3, youth elite or junior elite)
-
National elite (highest division)
-
International elite
To assess the type of pre-injury PA, the results from a single question, “Enter the physical activity/sport in which you are mainly involved”, were used. This question was answered with free text upon registration in the project. The questions regarding level and type of PA/sport have been developed for Project ACL by the research group. First, the scientific literature with respect to the topic was reviewed. Then, to ensure face validity, three physiotherapists, all with experience of patients with an ACL injury, took part in the development of the questions. Data from the 18-month follow-up and from the latest registered follow-up between 3 and 5 years after the ACL reconstruction were extracted from Project ACL.
Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics for Windows, version 25, 2017 (IBM Corp., Armonk, N.Y., USA). The sample-size calculation was made for the main outcome (ACL-RSI at the 18-month follow-up), where the estimated mean was based on data in a previous study [35]. A sample-size calculation showed that a total sample size of 72 patients were required to be able to identify a 13.4-point difference, corresponding to the minimal detectable change (MDC) [35] between groups with 80% power at an alpha level of 0.05.
Descriptive statistics for patient demographics and outcomes were reported with the count and proportion for categorical variables. Continuous variables were reported as the mean or median and standard deviation (SD) or minimum and maximum. The frequency of the 12 most common types of PA was reported at pre-injury, 18 months and 3, 4 and 5 years after ACL reconstruction.
For comparisons between patients with complete data and those lost to follow-up and between patients who maintained and did not maintain PA 3–5 years after the primary ACL reconstruction, the Fisher’s exact test for dichotomous variables was used. Pearson’s chi-square test for ordered categorical variables and the Mann–Whitney U test for non-parametric and non-normally distributed data. To assess normality for the variables of age, height, and weight, the z-score for skewness and kurtosis was calculated. As some of the continuous variables were not normally distributed, presented in Table 4 (Appendix) all between-group analyses were performed with non-parametric tests. The data were defined as normally distributed if the z-score was within ± 2.58. Significance tests were conducted at the 5% level.
Result
A total of 272 patients met the inclusion criteria (Fig. 1). Of the eligible patients (n = 504), 220 patients had no follow-up 3–5 years after the ACL reconstruction. In addition, three patients were excluded as they reported disease or an injury affecting their ability to be physically active 3–5 years after the ACL reconstruction and nine patients were excluded as they sustained a second ACL injury between the 18-month and 3- to 5-year follow-ups. There were no differences between included patients (n = 281) and patients lost to follow-up (n = 220), Table 1.
Figure 1 shows the inclusion of patients and the stratification into different groups for the comparison analysis. Of the included 272 patients, 114 (42%) had returned to their pre-injury level of PA at the 18-month follow-up.
On average, the included patients had a follow-up at 3.8 years (min–max: 2.9–5.1) after their ACL reconstruction. For 70% of the patients (191/272), more than 5 years had passed since the ACL reconstruction. For these patients, the last registered follow-up was extracted from the 3-, 4-, and 5-year follow-ups for 28% (53/191), 26% (50/191), and 46% (88/191), respectively.
In patients who had returned to their pre-injury level of PA (n = 114) at 18 months, 68% (n = 78) maintained the same level of PA 3–5 years after the ACL reconstruction. Patients who maintained their pre-injury level of PA reported higher levels of psychological readiness to return to sport (median: 98 versus 79; p = 0.013) at the 18-month follow-up, were 5.0 years older (p = 0.016), had a lower pre-injury Tegner (p = 0.005), and comprised more men (56% versus 44%; p = 0.028) compared with patients who did not maintain their PA (Tables 2 and 3). Because patients who maintained their pre-injury level of PA comprised a larger proportion of patients with a pre-injury level of PA on Tegner < 6 (42% versus 19%; p = 0.005; Table 2), a sub-group analysis of patients with a pre-injury level of PA on Tegner ≥ 6 was carried out. The rationale for this was based on the assumption that maintaining a lower Tegner is less demanding than maintaining a higher level of PA. This sub-group analysis confirmed the findings that patients who had maintained their pre-injury level of PA 3–5 years after ACL reconstruction were characterised by higher levels of psychological readiness to return to sport (102 versus 79; p-value = 0.008) at the 18-month follow-up. The sub-groups analysis revealed no other differences between patients who maintained and did not maintain their pre-injury level of PA. Moreover, since patients who maintained their pre-injury level of PA were 5 years older (Table 2), a sub-group analysis stratified by the age-groups 1) younger than 20, 2) 20 < 30 years, and 3) ≥ 30 years of age was carried out. This sub-group analysis revealed that patients younger than 20 years of age who had maintained their pre-injury level of PA 3–5 years after ACL reconstruction were characterised by higher levels of present (9.8 vs 9.4; p = 0.019) and future (9.5 versus 8.7; p = 0.039) self-efficacy, higher levels of psychological readiness to return to sport (111 versus 78; p = 0.011), and enhanced function in sports and recreation (95 versus 80; p = 0.023) at the 18-month follow-up. No other differences between patients, younger than 20 years of age, who maintained and had not maintained their pre-injury level of PA were found. For patients 20 < 30 years and ≥ 30 years of age, respectively, no differences between patients who maintained and did not maintain their pre-injury level of PA were found (Table 2).
Type and frequency of PA
Figure 2 presents the patients’ main PA before their ACL injury and at 18 months and the follow-up between 3 and 5 years after the ACL reconstruction. Before the ACL injury, the four main PAs were football (28.0%), running/jogging (9.5%), strength training (8.7%), and handball (8.7%). At the following follow-ups, the most common PA was strength training, ranging from 20.2 to 25.7% Participation in organised sports, such as in football, handball, and floorball, decreased from pre-injury to the follow-up between 3 and 5 years for all sports (Fig. 2).
Figure 3 presents the self-reported frequency of PA at 18 months and the follow-up between 3 and 5 years after ACL reconstruction. At the 18-month follow-up, 9/229 patients reported that they were physically inactive according to the WHO. At the same follow-up, 38 patients (16.6%) reported that they were physically active more than 30 min of/day or more than 150 min/week. Three out of these 38 patients were younger than 18 years of age at that follow-up. At the follow-up between 3 and 5 years after the ACL reconstruction, 8.5% of 272 patients reported physical inactivity. At the 18-month follow-up, 14.0% of the included patients reported that they exercised regularly, 3–7 days/week with regular participation in competition, or more, which corresponds to the four highest possible levels of PA (Fig. 3). The corresponding frequency at the follow-up between 3 and 5 years was 13.3.
Level of physical activity 18 months to 5 years after an ACL reconstruction. Physically inactive less than 30 min of physical activity/day or less than 150 min/week; physically active more than 30 min of physical activity/day or more than 150 min/week; exercising up to 2 days/week of regular exercising; active exercising regular exercising 3–7 days/week without regular participation in competition; active competition regular exercising 3–7 days/week with regular participation in competition; Elite Division 2–3, youth elite or junior elite; national elite highest division. 3–5 years refers to the latest performed follow-up between 3 and 5 years after ACL reconstruction. Missing values for 43 and 26 patients were present at the 18-month and the 3–5-year follow-ups, respectively
Discussion
The main finding in this prospective cohort study was that around two in three patients, who returned to their pre-injury level of PA at 18 months after ACL reconstruction, maintained that level at a follow-up 3–5 years after surgery. Patients who had maintained their pre-injury level of PA were characterised by higher psychological readiness to return to sport, older age, lower pre-injury level of PA and male sex. At the follow-up 3–5 years after the ACL reconstruction, more than 90% met the recommendations for PA. However, the prevalence of physical inactivity had increased from 3.9 to 8.5% and the involvement in organised PA had decreased compared with the 18-month follow-up.
In all, 42% of all included patients (114/272) had returned to their pre-injury level of PA at the 18-month follow-up. Of these, 68% (64/114) had at least maintained the same level of PA 3–5 years after the ACL reconstruction. This means that less than one-third of all the included patients participated at their pre-injury level of PA 3–5 years after their ACL reconstruction, which is lower than the 45% that has previously been reported in patients 2–7 years after ACL reconstruction [3]. Patients who maintained their pre-injury level of PA 3–5 years after the ACL reconstruction were 5 years older than patients who did not maintain their pre-injury level of PA. This finding partly contradicts previous results reported by Ardern et al. [3] who reported that a larger proportion of patients younger than 25 years of age had returned to their pre-injury level of sport 2–7 years after ACL reconstruction compared with patients older than 25 years of age. The discrepancies between the results of the present study and the results reported by Ardern et al. [3] could be explained by the broader inclusion criteria in the present study; patients were included irrespective of their pre-injury type and level of PA, while Ardern et al. [3] included patients who regularly participated in sports. In the present study, patients who had maintained their pre-injury level of sport comprised a higher proportion of patients with a pre-injury Tegner of 1–5 than patients who did not maintain their pre-injury level of sport (42% versus 19%; p = 0.005). When only analysing patients with a pre-injury Tegner of ≥ 6, there was no difference in age between the two groups of patients, which confirms previous findings that Tegner is inversely correlated to individuals’ age [9]. Furthermore, the finding that patients who maintained their pre-injury level of PA were characterised by male sex confirms previous literature [3].
The differences in the total score on the ACL-RSI between patients who had returned and maintained their pre-injury level of PA and patients who had returned but had not maintained their pre-injury level of PA, 3–5 years after an ACL reconstruction (98 versus 79, p = 0.013), is of interest. In particular, as this finding was confirmed when analysing only the patients with a pre-injury Tegner of ≥ 6 (101.5 versus 79; p = 0.008) and in patients younger than 20 years of age (111 vs 78; p = 0.011). Psychological readiness to return to sport, as measured by the ACL-RSI, has repeatedly been reported to be associated with a successful return to sport [4, 31, 37] within the first 12 months after ACL reconstruction. It is therefore reasonable to believe that psychological readiness to return to sport is also associated with maintaining PA during the first 5 years after ACL reconstruction, especially in male patients of younger age. However, Type-I errors, i.e., no differences between the groups, could not been ruled out as there were missing values for the ACL-RSI in the two groups who had and had not maintained their pre-injury level of PA. The reason for missing values on the ACL-RSI is that this questionnaire was introduced in Project ACL 1.5 years after the start of the project. Missing values in combination with the small proportion of patients who had returned to their pre-injury level of PA resulted in a limited number of patients in each group, 67 versus 27 patients in the main analysis and only 15 versus 8 in the sub-group analysis stratified by age-groups.
In the light of the increased risk of developing symptomatic knee osteoarthritis after an ACL injury [17, 25], it is of great importance that patients with an ACL injury remain physically active throughout life. In the present study, the included patients appeared to quit organised PA, such as football, handball, and floorball, in favour of strength training and cycling/indoor cycling, when comparing the reported type of PA from pre-injury up to 5 years after the ACL reconstruction. With respect to the recommendation that patients with knee OA should be treated with a combination of aerobic and strength training exercises that load the quadriceps and hamstring muscles at regular intervals [26], it is promising that strength training was by far the most common type of PA at all follow-ups between 18 months and 5 years after the ACL reconstruction. However, the finding that patients after an ACL reconstruction appear to give up organised sports in favour of individual exercising confirm previous findings [16], but is not unique to this group. According to the “Special Eurobarometer 472 data on physical activity” [12], the frequency of exercise and sport is reported to decrease with age. Similarly, younger people are more likely to be engaged in other physical activities, as well as doing vigorous and moderate physical activity [12]. Therefore, the findings of an increased prevalence of physical inactivity and a reduction of involvement in organised PA compared with the 18-month follow-up in the present study may be explained be this age phenomenon. However, this is one of the first study that in detail describe the frequency, level, and type of physical activity in a group of patients after a primary ACL reconstruction. To better understand how patients after an ACL reconstruction differ from healthy individuals, future studies should include a healthy reference group.
Previous studies have reported that ACL-reconstructed patients are less physically active compared with healthy matched controls [7, 22]. In Sweden, 34% of individuals between 16 and 64 years of age do not meet the WHO’s recommendation of 150–300 min of PA per week [10]. Clearly, the proportions of physical inactivity in the present study were lower, ranging from 4% at the 18 month follow-up to about 8%. From the perspective of preventing non-communicable diseases, this result appears promising. However, as these patients, at group level, had a high pre-injury level of PA, reflected by the Tegner, as well as the fact that the majority of patients stated that they were involved in some sort of organised PA before their injury, the proportion of physically inactive individuals must be regarded as too high. To better understand the PA habits of patients after ACL reconstruction and compare the proportions of patients involved in different types and frequencies of PA, a prospective cohort study with a sufficient number of patients using PROs in combination with device-based assessment approaches appears to be necessary [15, 21].
This study has some limitations that were taken into account before conclusions were drawn. First, a limited, yet homogeneous group of patients were included, as strict inclusion criteria were used. The fact that only a minority of patients had returned to their pre-injury PA level at 18 months after their ACL reconstruction resulted, however, in a limited group of included patients. Nevertheless, the results can be regard as generalisable to patients after ACL reconstruction at the age of 15–65 years, as no differences were seen with respect to patient demographics or anthropometrics at the 18-month follow-up between included patients and patients lost to follow-up. Second, the use of PROs and/or single questions to assess PA is associated with limitations [11, 21]. As the Tegner only reflects how knee strenuous the PA is, we combined the Tegner with a single question where patients were asked to enter the main PA in which they had participated during the last month. To assess the frequency of PA, another single question was used, developed, and tested for face validity by the research group. However, as for all subjective measurements of the frequency of PA, it is likely that the question regarding the frequency of PA is also associated with overestimation [11, 21]. Finally, no data with respect to frequency, type, and severity of possibly associated injuries were available. Therefore, identifying patients with associated injuries that may have influenced the patients’ postoperative PA was not possible.
Few previous studies have investigated the characteristics of patients who return to their previous level of PA and maintain at least the same level of PA in the medium-term perspective after an ACL reconstruction. Moreover, this study adds a description of the level, frequency, and type of PA participation during the first 5 years after surgery in a large cohort of patients.
Conclusion
Two out of three patients who have returned to their previous level of PA at 18 months can be expected to maintain that level, 3–5 years following ACL reconstruction. Patients who maintained their level of PA were mainly characterised by a higher level of psychological readiness, especially in patients who participated in knee-strenuous sport and were younger than 20 years of age. Regardless of what level of PA patients return to, 9 of 10 patients can be expected to meet the recommendations for PA and about 1 out of 3 patients can be expected to exercise regularly, three-to-seven times per week, mainly involved in strength training and running/jogging. However, the results of this study suggest that patients become more physically inactive over time, implicating the importance of clinicians helping patients find a suitable PA that may help patients maintain an active lifestyle.
Availability of data and materials
The dataset used and/or analysed is available from the corresponding author on request.
References
Ardern CL, Glasgow P, Schneiders A, Witvrouw E, Clarsen B, Cools A et al (2016) 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med 50:853–864
Ardern CL, Taylor NF, Feller JA, Webster KE (2014) Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 48:1543–1552
Ardern CL, Taylor NF, Feller JA, Webster KE (2012) Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med 40:41–48
Ardern CL, Taylor NF, Feller JA, Webster KE (2013) A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med 47:1120–1126
Beischer S, Hamrin Senorski E, Thomee C, Samuelsson K, Thomee R (2019) How Is Psychological outcome related to knee function and return to sport among adolescent athletes after anterior cruciate ligament reconstruction? Am J Sports Med 47:1567–1575
Beischer S, Hamrin Senorski E, Thomee P, Thomee R (2021) Validation of an 18-item version of the Swedish Knee Self-Efficacy Scale for patients after ACL injury and ACL reconstruction. J Exp Orthop. https://doi.org/10.1186/s40634-021-00414-2
Bell DR, Pfeiffer KA, Cadmus-Bertram LA, Trigsted SM, Kelly A, Post EG et al (2017) Objectively Measured physical activity in patients after anterior cruciate ligament reconstruction. Am J Sports Med 45:1893–1900
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37:890–897
Briggs KK, Steadman JR, Hay CJ, Hines SL (2009) Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med 37:898–901
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G et al (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 54:1451–1462
Ekblom O, Ekblom-Bak E, Bolam KA, Ekblom B, Schmidt C, Soderberg S et al (2015) Concurrent and predictive validity of physical activity measurement items commonly used in clinical settings–data from SCAPIS pilot study. BMC Public Health. https://doi.org/10.1186/s12889-015-2316-y
European Commission (2022) Special Eurobarometer 525 - Sport and physical Activity.https://doi.org/10.2766/356346
Everhart JS, Best TM, Flanigan DC (2015) Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 23:752–762
Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM (2015) Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med 49:1033–1041
Filbay SR, Skou ST, Bullock GS, Le CY, Raisanen AM, Toomey C et al (2022) Long-term quality of life, work limitation, physical activity, economic cost and disease burden following ACL and meniscal injury: a systematic review and meta-analysis for the OPTIKNEE consensus. Br J Sports Med. https://doi.org/10.1136/bjsports-2022-105626
Gignac MA, Cao X, Ramanathan S, White LM, Hurtig M, Kunz M et al (2015) Perceived personal importance of exercise and fears of re-injury: a longitudinal study of psychological factors related to activity after anterior cruciate ligament reconstruction. BMC Sports Sci Med Rehabil. https://doi.org/10.1186/2052-1847-7-4
Grassi A, Pizza N, Al-Zu’bi BBH, Fabbro GD, Lucidi GA, Zaffagnini S (2022) Clinical outcomes and osteoarthritis at very long-term follow-up after ACL reconstruction: a systematic review and meta-analysis. Orthop J Sports Med 10:23259671211062240
Hamrin Senorski E, Samuelsson K, Thomee C, Beischer S, Karlsson J, Thomee R (2017) Return to knee-strenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surg Sports Traumatol Arthrosc 25:1364–1374
Ithurburn MP, Longfellow MA, Thomas S, Paterno MV, Schmitt LC (2019) Knee Function, Strength, and resumption of preinjury sports participation in young athletes following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 49:145–153
Kuenze C, Cadmus-Bertram L, Pfieffer K, Trigsted S, Cook D, Lisee C et al (2019) Relationship between physical activity and clinical outcomes after ACL reconstruction. J Sport Rehabil 28:180–187
Kuenze C, Collins K, Pfeiffer KA, Lisee C (2022) Assessing physical activity after ACL injury: moving beyond return to Sport. Sports Health 14:197–204
Kuenze C, Lisee C, Pfeiffer KA, Cadmus-Bertram L, Post EG, Biese K et al (2019) Sex differences in physical activity engagement after ACL reconstruction. Phys Ther Sport 35:12–17
Kvist J, Osterberg A, Gauffin H, Tagesson S, Webster K, Ardern C (2013) Translation and measurement properties of the Swedish version of ACL-Return to Sports after Injury questionnaire. Scand J Med Sci Sports 23:568–575
Lai CCH, Ardern CL, Feller JA, Webster KE (2018) Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med 52:128–138
Lie MM, Risberg MA, Storheim K, Engebretsen L, Oiestad BE (2019) What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med 53:1162–1167
Masud S, Sheehan B, Rousseau-Saine A, Tucker A, Sandman E, Wong I et al (2021) Arthroscopy Association of Canada Position Statement on exercise for knee osteoarthritis: a systematic review of guidelines. Orthop J Sports Med 9:23259671211016900
Nwachukwu BU, Adjei J, Rauck RC, Chahla J, Okoroha KR, Verma NN et al (2019) How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? a systematic review. Orthop J Sports Med 7:2325967119845313
Oiestad BE, Juhl CB, Culvenor AG, Berg B, Thorlund JB (2022) Knee extensor muscle weakness is a risk factor for the development of knee osteoarthritis: an updated systematic review and meta-analysis including 46 819 men and women. Br J Sports Med 56:349–355
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and Osteoarthritis Outcome Score (KOOS)–validation of a Swedish version. Scand J Med Sci Sports 8:439–448
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Sonesson S, Kvist J, Ardern C, Osterberg A, Silbernagel KG (2017) Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee Surg Sports Traumatol Arthrosc 25:1375–1384
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349
Warburton DER, Bredin SSD (2017) Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol 32:541–556
Webster KE, Feller JA (2021) Evaluation of the responsiveness of the anterior cruciate ligament return to sport after injury (ACL-RSI) Scale. Orthop J Sports Med 9:23259671211031240
Webster KE, Feller JA, Lambros C (2008) Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport 9:9–15
Xiao M, van Niekerk M, Trivedi NN, Hwang CE, Sherman SL, Safran MR et al (2022) Patients who return to sport after primary anterior cruciate ligament reconstruction have significantly higher psychological readiness: a systematic review and meta-analysis of 3744 patients. Am J Sports Med. https://doi.org/10.1177/036354652211024203635465221102420
Acknowledgements
None.
Funding
Open access funding provided by University of Gothenburg. The work of Susanne Beischer was supported by The Local Research and Development Council Gothenburg and Södra Bohuslän.
Author information
Authors and Affiliations
Contributions
All the authors contributed to planning the project. SB drafted the manuscript. All the authors critically revised the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None to declare.
Ethical approval
The data have been coded and none of the included patients could be identified during analyses. The study was approved by the Regional Ethical Review Board in Gothenburg and the Swedish Ethical Review Authority (registration numbers: 265–13, T023-17, 2020–02501).
Informed consent
All the included patients provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beischer, S., Hamrin Senorski, E. & Thomeé, R. Patients that maintain their pre-injury level of physical activity 3–5 years after ACL reconstruction are, 18 months after surgery, characterised by higher levels of readiness to return to sport. Knee Surg Sports Traumatol Arthrosc 31, 596–607 (2023). https://doi.org/10.1007/s00167-022-07230-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07230-w