Abstract
Purpose
Results from recent randomised controlled trials demonstrate the superiority of surgery over physiotherapy in patients with femoroacetabular impingement (FAI) of the hip in early follow-up. However, there is paucity of evidence regarding which factors influence outcomes of FAI surgery, particularly notable is the lack of information on the effect of impingement subtype (cam or pincer or mixed) on patient reported outcomes measures (PROMs). This study aims to evaluate the early outcomes of hip arthroscopy for FAI, and their determinants.
Methods
This is a retrospective analysis of prospectively collected data from the UK Non-Arthroplasty Hip Registry (NAHR) of patients undergoing arthroscopic intervention for FAI between 2012 and 2019. The null hypothesis was that there is no difference in PROMs, based on morphological subtype of FAI treated or patient characteristics, at each follow-up timepoint. The outcome measures used for the study were the iHOT-12 score and the EQ5D Index and VAS 6- and 12-month follow-up.
Results
A cohort of 4963 patients who underwent arthroscopic treatment of FAI were identified on the NAHR database. For all FAI pathology groups, there was significant improvement from pre-operative PROMs when compared to those at 6 and 12 months. Overall, two-thirds of patients achieved the minimum clinically important difference (MCID), and almost half achieved substantial clinical benefit (SCB) for iHOT-12 by 12 months. Pre-operatively, and at 12-month follow-up, iHOT-12 scores were significantly poorer in the pincer group compared to the cam and mixed pathology groups (p < 0.01). Multivariable analysis revealed PROMS improvement in the setting of a higher-grade cartilage lesion.
Conclusion
This registry study demonstrates that hip arthroscopy is an effective surgical treatment for patients with symptomatic FAI and results in a statistically significant improvement in PROMs which are maintained through 12 months follow-up.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) can give rise to hip pain, reduced range of movement, loss of function, and eventually arthritis of the hip [22, 26]. This condition can be classified as one of three morphological types; cam, pincer, or mixed [13]. The primary aim of surgical treatment of FAI is hip preservation through decreasing abnormal contact stresses across the hip joint, which can subsequently delay progression to osteoarthritis [50] and potentially improve patients’ symptoms and quality of life. Whilst Burman described direct visualisation of the hip joint through arthroscopic means in a cadaveric study in 1931 [4], Ganz originally described FAI and also ‘open surgical dislocation’ for surgical management of FAI [12]. However, arthroscopic management of FAI has now become standard of care despite initial scepticism [2, 3, 16, 36, 45].
Results from randomised control trials are now available which demonstrate the superiority of surgery over physiotherapy in patients with FAI [15, 34]. There are a number of studies that have discussed patient reported outcomes for FAI surgery, some of these have been small [5,6,7,8,9,10,11, 14, 19, 21, 25, 29, 30, 32, 35, 39, 40, 48, 51, 53,54,55,56,57,58,59, 61] however, the Danish Hip Arthroscopy Registry (DHAR), like the UK NAHR, have been able to demonstrate the outcomes of large numbers of patients undergoing surgery for FAI [43, 44]. Efficacy has also been demonstrated in adolescents as well as young adults [41]. Aside from the publications from the DHAR, there is also a paucity of studies looking at differences in patient reported outcomes measure (PROMs) based on morphology type, in FAI and the corresponding improvements in PROMs scores.
The aim of this study, therefore, was to [1] report the demographics and early outcomes for patients undergoing hip arthroscopy for FAI up to 12 months follow-up and [2] to compare outcomes by FAI pathology groups using data from the UK NAHR. The null hypothesis was that there would be no difference in terms of the 12 months iHOT-12 gain vs pre-operative scores when comparing FAI pathology groups.
Materials and methods
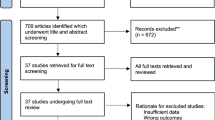
Approval for this observational study was granted by the NAHR steering committee (reference NAHR/2018/02). All patients 14 years and older who underwent a hip arthroscopy procedure to address an FAI lesion between 2012 and 2019 were identified from the NAHR database (Fig. 1, study flow diagram). Procedures used to define FAI were excision of femoral “cam” lesion and/or excision of acetabular “pincer” lesion (including rim recession [simple], rim recession with labral reattachment, and sub-spinous resection).
Patient demographics and data related to clinical diagnosis and surgical procedure are collected and uploaded by trained staff using a structured electronic form which allows for recording of isolated or simultaneous femoral and acetabular procedures. Patients who consent to data collection receive questionnaires to determine EQ-5D Index and iHOT-12 scores pre-operatively and at six months, one, two- and five-year follow-up. Follow-up data was captured in September 2020 to allow a minimum of 12 months follow-up. Due to the low return-rate of patient questionnaires at two or more years follow-up in this cohort (<5% of cases returned 2-year PROMS) it was only possible to report outcomes up to one year post-operatively. Body mass index (BMI) was also collected and reported as both a continuous and a categorical variable according to World Health Organisation (WHO) groups. Where available, acetabular chondral damage was determined as the single worst area of cartilage damage recorded intra-operatively according to Konan et al.’s [28] description (Grade 1—wave sign with intact chondrolabral junction, Grade 2—Chondrolabral junction separation but no delamination, Grade 3—Delamination, Grade 4—Exposed bone) [20]. Femoral cartilage defects were classified according to the Outerbridge classification [52].
Patients were classified according to pathology into three groups dependent upon the index procedure performed for FAI which comprised: (1) “cam”: excision of cam lesion (with no recorded procedure to treat pincer pathology during the same surgery), (2) “pincer”: excision pincer lesion (with no recorded procedure to treat cam pathology during the same surgery) and (3) “mixed”: excision of both a cam and pincer lesion during the same operation. Concurrent femoral and acetabular procedures performed in association with the index procedure which defined the pathology group were also determined for each pathology group (Table 1).
Several thresholds for the minimum clinically important difference (MCID) and substantial clinical benefit (SCB) following hip arthroscopy for FAI have been reported in the literature [23]. For patients in whom pre and post-operative outcome scores were recorded at 12 month follow-up, an improvement in iHOT-12 score of ≥13 and ≥28 were used as reference criteria for achieving MCID and SCB respectively as reported by Martin et al. [37] and Kivlan et al.[27] Additionally, the proportion of cases achieving an increase in iHOT-12 score greater than or equal to thresholds from 1 to 40 were calculated, in order that the results can be compared with the existing and future literature and provide evidence to support informed patient consent.
Statistical analysis
Bivariate analyses were conducted using Chi-square tests for categorial outcomes and Student’s t test or ANOVA as appropriate for continuous outcomes. BMI data were missing in 40% of cases; to maximise the number of observations available for multivariable modelling BMI was therefore treated as a categorical variable and these patients assigned to a “missing” group. Statistical analysis was performed in STATA (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.) and R (R Core Team [2019]. R: A language and environment for statistical computing, Vienna, Austria).
Results
A series of 4963 arthroscopies performed for treatment of FAI were identified from the NAHR database. A significantly higher proportion of female patients were observed in the pincer group (Table 2; p < 0.0001). Overall, for the entire cohort, there was significant improvement in pre-operative scores which were maintained up to 12 months (Table 3).
Pre-operatively, and at 6, and 12-month follow-up, iHOT-12 scores (unadjusted) were significantly poorer in the pincer group compared to the cam and mixed pathology groups (p < 0.01) with a similar relationship observed for EQ-5D Index scores. Within each pathology group, patients experienced statistically significant improvement in baseline pre-operative iHOT-12 and EQ-5D Index scores at 6 months which was maintained up to 12 months post-operatively (all p < 0.0001), however there were no significant between group differences in the magnitude of iHOT-12 or EQ-5D Index of VAS score improvement on univariable analysis.
Outcome scores by age group
For all FAI pathology types, significant improvement in iHOT-12 score was maintained up to 12 months post-operatively for younger (under 40 years) and older age groups. Older patients with isolated cam pathology started from significantly higher baseline iHOT-12 scores but had significantly poorer iHOT-12 improvement by 6 months compared to younger patients, however, statistical significance was lost by 12 months (Fig. 2). At 12 months, there were no differences in 12-month EQ-5D Index scores or degree of improvement for all FAI pathology groups when comparing younger and older patients and all maintained significant improvement compared to pre-operative scores.
Outcome scores by sex
Considering all FAI pathology groups combined, male patients started from a significantly higher pre-operative baseline iHOT-12 and reached significantly higher iHOT-12 scores by 12 months compared to female patients; this significance was largely driven by better post-operative outcome scores in male patients who underwent treatment for cam pathology only (Fig. 3).
For each FAI pathology group and when considering all FAI pathology groups collectively, both male and female patients saw significant improvement (delta) in their baseline pre-operative iHOT-12 score up to 6- and 12-months following surgery (all p < 0.01).
MCID & SCB
Overall, 67% of patients achieved the MCID (increase in iHOT-12 of ≥13) at up to 12 months (Fig. 4). The proportion of cases achieving MCID in the pincer group (63%) was lower than in cam (67%) and mixed (66%) pathology groups (Fig. 3). Overall, 47% of patients achieved SCB (increase in iHOT-12 of ≥28) by 12 months. Again, the proportion of cases achieving SCB in the pincer group (41%) was lower than in cam (48%) and mixed (46%) pathology groups. Data showing the proportion of cases achieving iHOT-12 improvement for thresholds between +1 and +40 are available in the supplementary materials (Supplementary material Table 1).
Predictors of PROMS improvement
Considering the overall cohort including all FAI pathology groups, patients who returned both pre and 12-month post-operative iHOT-12 questionnaires were, on average, older (36.6 versus 35.0 years, p < 0.0001) and more likely to be female (p < 0.0001) than those who did not return one or both questionnaires (p < 0.0001, supplementary table 2); there were also differences in the proportions of femoroacetabular impingement (FAI) pathology seen (p = 0.022). Differences in 12-month follow-up rates between the FAI pathology groups (Cam = 37.1%, Pincer = 32.5% and Mixed = 39.4%) may, therefore, confound the primary outcome measure of iHOT-12 improvement (delta) as responders are inherently different to non-responders. To attempt to account for the above, a combination of random sampling and propensity score matching were used to create a synthetic cohort of cases for each FAI pathology group to balance the demographic differences that may have arisen from differences in follow-up rates between the three groups. This methodology is described fully in the supplementary materials and adapted from methods published previously by this group [18]. This synthetic cohort (n = 1000, supplementary materials Table 3) was then used as the basis of a multivariable linear regression model predicting iHOT-12 12-month improvement.
Age, sex, severity of any recorded acetabular chondral lesion, BMI, pre-operative outcome score and FAI pathology group were used to predict iHOT-12 score improvement at 12 months in multivariable analysis after the creation of a novel synthetic cohort (n = 1000, patient characteristics are reported in supplementary table 3). Whilst not statistically significant, pincer pathology and a higher-grade chondral lesion showed the largest association with poorer iHOT-12 improvement at 12 months, however, there was evidence of a linear trend with respect to increasing chondral damage (Table 4). Chondral grading was therefore re-modelled as an ordered categorical variable (after excluding 341 [34%] patients in the synthetic cohort with missing chondral grading data) which confirmed a statistically significant association between increasing lesion grade and detrimental iHOT-12 improvement (coefficient −1.94 (95%CI −3.56, −0.31, p = 0.020).
Discussion
The principal finding of this study was that hip arthroscopy is an effective surgical treatment for patients with symptomatic FAI and was associated with significant improvement in patient outcomes which are maintained at 12 months follow-up. MCID is achieved in two-thirds of patients and just under half of patients have a substantial clinical benefit by 12 months. Outcomes appear better for cam and mixed pathologies as compared with pincer type lesions.
This study demonstrates that the majority of patients, irrespective of age, demonstrated a statistically significant improvement in outcome scores, although patients under 40 years may obtain greater benefit. When looking at previously published studies, age is a recognised determining factor for outcome. Domb et al. show, age to be a predictive factor for post-operative Non Arthritic Hip Score (NAHS) [9] and Kaldau et al. found that age significantly influenced the Hip Sports Activity Scale (HSAS) and, furthermore, they identified that there is a statistically significant difference in post-operative HSAS when comparing patients less than or equal to 40 years of age versus those over 40. This is mirrored in a study by McCormick et al. who stated that undergoing surgery for FAI at 39 years of age or younger was predictive of good to excellent results at a minimum of 2 years after surgery compared with a patient 40 years or older [38]. Likewise Lin et al. demonstrated that middle aged (35–50 years) and older patients (51–75 years) experienced greater declines in outcomes, when compared to young patients (15–34) [31].
When considering sex, males had significantly higher pre-operative baseline PROMs, as well as higher post-operative PROMs at 12 months. As a result, females have a significantly greater improvement in PROMs at 12 months. Indeed, the studies published in the literature which looked at outcomes based on sex [11, 17, 57] only consider the final PROM score with results matching this study’s findings. In these, the absolute score was statistically significantly better for males; however, this does not consider the degree of clinical improvement patients see, which is important to consider when selecting patients for operative intervention. Joseph et al. also considered the change in PROM score, as well as absolute values, and their findings echoed this study, with greater change/improvement in scores seen in females at 6 and 12 months [24].
Saltzman et al. have also looked at the influence of BMI on outcomes in FAI surgery and identified significant differences in PROMs based on BMI. They observed normal BMI patients, followed by underweight patients, demonstrating greater scores than their overweight, obese, and morbidly obese counterparts [56]. In multivariable modelling, similar trends were observed in the present study regarding lower score improvement in obese patients as compared to patients of normal BMI, however this did not reach statistical significance.
Data on the effect of FAI morphology type (cam, pincer, mixed) on patient reported outcomes appears to be limited, particularly when considering such a large number of procedures, with the exception of published work from the DHAR [43]. Beck et al. identified that the morphology of FAI influences the pattern of damage seen in the hip but did not correlate this with PROMs data [1]. Moon et al. found no difference in PROMs (Harris Hip Score and WOMAC) scores based on morphological subtype [42]. In the present study, iHOT-12 scores pre-operatively and at 12 months were significantly worse in the pincer group, than those in the cam and mixed group. Palmer et al. noted that, when using the Harris Hip Score (HHS) patients with mixed cam and pincer deformity has worse outcomes than those with cam alone, however, they excluded patients with “pincer only” FAI and therefore comparison between all morphological types could not be made [53].
Nho et al. looked at survivorship and outcome of hip arthroscopy for FAI syndrome performed with modern surgical techniques and reported MCID achievement of 73% in a series of 935 patients [47]. Similarly, Nwachukwu et al. reported that 68.1% patients in a series of 364 patients achieved improvement beyond MCID for Hip Outcome Score—Activities of Daily Living [37, 49] and Malviya et al. found that 76.6% patients had an improvement in QoL, (Quality of Life) measured in improvement of QoL score[46], after arthroscopic surgery for FAI [33]. In this study, 67% of patients achieved improvement in their i-HOT12 scores beyond the MCID of 13, this was greater in patients with cam and mixed pathologies as compared with pincer. The overall figure seems to be slightly less than previous reports and this might be explained by the NAHR including data submitted by surgeons of differing levels of experience including low-volume surgeons, whilst all the published evidence reports are from high volume centres with experienced surgeons. This aspect of the study makes it pragmatic and allows for realistic deductions to be made.
The NAHR allows for the capture of national data, within the UK, pertaining to ‘non-arthroplasty’ elective hip surgery procedures. It has been demonstrated that database studies are better at reporting certain outcome measures, such as: complications, revision and conversion to arthroplasty, when compared with than conventional original research publications, outlining their importance [60]. Furthermore, registries allow collection of data from low-volume surgeons and those of different skill sets presenting a more realistic picture of achievable results than results from high volume surgeons in specialist centres. The present study includes results from 69 surgeons contributing between 1 and 555 cases (mean = 72 cases, median = 25 cases) and whilst outcomes were not adjusted for surgeon experience, results of this study show arthroscopy for FAI to be a procedure providing clinical benefit to patients amongst the breadth of surgeons contributing to the NAHR.
The authors note the limitations to this study, including largely the relatively short duration of follow-up. The NAHR collects scores pre-operatively and at six months, one, two- and five-year follow-up. Due to the low return-rate of patient outcome scores at two or more years follow-up, in this cohort it was only possible to report outcomes up to one year post-operatively. However, the authors also recognise that the NAHR will continue to evolve over time and could allow for the development of more robust data collection strategies moving forward. The lessons learned from it may also be useful in the development of other registries which would allow for further population-based studies to be undertaken. Other limitations include: no standardisation of the surgical decision making process amongst surgeons, lack of operative standardisation and post-operative standardisation between centres and that, nationally, not all surgeons are contributing to the NAHR. Furthermore, by not capturing radiographic parameters it is not possible to correlate the influence of these on PROM scores and assumes the categorisation of morphological subtype by operating surgeon was correct.
To the best of the authors’ knowledge, this is one of the largest studies to date, reporting short term patient reported outcomes of hip arthroscopy for the management of FAI in a pragmatic setting. The only study known to the authors that includes a larger number of procedures is that from the DHAR that looked at more than 5000 procedures [43].
Conclusion
Arthroscopic treatment of symptomatic FAI was associated with statistically significant improvement in patient reported clinical outcome scores for the majority of patients, however, consideration to specific groups must be paid, such as; extremes of age, high BMI and the presence of pincer pathology, at least, in the short term. The outcomes may not be universally successful and this study provides important evidence to facilitate patient-clinician discussion regarding expected outcomes and guide informed consent.
References
Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 87:1012–1018
Bedi A, Chen N, Robertson W, Kelly BT (2008) The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy 24:1135–1145
Bedi A, Kelly BT, Khanduja V (2013) Arthroscopic hip preservation surgery: current concepts and perspective. Bone Joint J 95-B:10–19
Burman MS (2001) Arthroscopy or the direct visualization of joints: an experimental cadaver study. 1931. Clin Orthop Relat Res 13:5–9
Byrd JW, Jones KS (2011) Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy 27:1379–1388
Capogna BM, Ryan MK, Begly JP, Chenard KE, Mahure SA, Youm T (2016) Clinical outcomes of hip arthroscopy in patients 60 or older: a minimum of 2-year follow-up. Arthroscopy 32:2505–2510
Comba F, Yacuzzi C, Ali PJ, Zanotti G, Buttaro M, Piccaluga F (2016) Joint preservation after hip arthroscopy in patients with FAI. Prospective analysis with a minimum follow-up of seven years. Muscles Ligaments Tendons J 6:317–323
Cvetanovich GL, Weber AE, Kuhns BD, Alter J, Harris JD, Mather RC 3rd et al (2018) Hip arthroscopic surgery for femoroacetabular impingement with capsular management: factors associated with achieving clinically significant outcomes. Am J Sports Med 46:288–296
Domb BG, Martin TJ, Gui C, Chandrasekaran S, Suarez-Ahedo C, Lodhia P (2018) Predictors of clinical outcomes after hip arthroscopy: a prospective analysis of 1038 patients with 2-year follow-up. Am J Sports Med 46:1324–1330
Fiorentino G, Fontanarosa A, Cepparulo R, Guardoli A, Berni L, Coviello G (2015) Treatment of cam-type femoroacetabular impingement. Joints 3:67–71
Frank RM, Lee S, Bush-Joseph CA, Salata MJ, Mather RC, Nho SJ (2016) Outcomes for hip arthroscopy according to sex and age: a comparative matched-group analysis. J Bone Joint Surg Am 98:797–804
Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U (2001) Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 83:1119–1124
Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 417:112–120
Gedouin JE, May O, Bonin N, Nogier A, Boyer T, Sadri H et al (2010) Assessment of arthroscopic management of femoroacetabular impingement. A prospective multicenter study. Orthop Traumatol Surg Res 96:S59-67
Griffin DR, Dickenson EJ, Wall PDH, Achana F, Donovan JL, Griffin J et al (2018) Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet 391:2225–2235
Griffiths EJ, Khanduja V (2012) Hip arthroscopy: evolution, current practice and future developments. Int Orthop 36:1115–1121
Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT (2013) Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy 29:54–63
Holleyman R, Sohatee MA, Witt J, Bankes MJK, Andrade TJ, Board T et al (2020) Periacetabular osteotomy for developmental dysplasia of the hip and femoroacetabular impingement: a study using the U.K. Non-Arthroplasty Hip Registry (NAHR) Data Set. J Bone Joint Surg Am 102:1312–1320
Hufeland M, Krüger D, Haas NP, Perka C, Schröder JH (2016) Arthroscopic treatment of femoroacetabular impingement shows persistent clinical improvement in the mid-term. Arch Orthop Trauma Surg 136:687–691
Ilizaliturri VM Jr, Byrd JW, Sampson TG, Guanche CA, Philippon MJ, Kelly BT et al (2008) A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy 24:534–539
Ilizaliturri VM, Orozco-Rodriguez L, Acosta-Rodríguez E, Camacho-Galindo J (2008) Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty 23:226–234
Imam S, Khanduja V (2011) Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop 35:1427
Jónasson P, Baranto A, Karlsson J, Swärd L, Sansone M, Thomeé C et al (2014) A standardised outcome measure of pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement: cross-cultural adaptation and validation of the international Hip Outcome Tool (iHOT12) in Swedish. Knee Surg Sports Traumatol Arthrosc 22:826–834
Joseph R, Pan X, Cenkus K, Brown L, Ellis T, Di Stasi S (2016) Sex differences in self-reported hip function up to 2 years after arthroscopic surgery for femoroacetabular impingement. Am J Sports Med 44:54–59
Kaldau NC, Brorson S, Holmich P, Lund B (2018) Good midterm results of hip arthroscopy for femoroacetabular impingement. Dan Med J 65:A5483
Khanduja V, Villar RN (2007) The arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc 15:1035–1040
Kivlan BR, Martin RL, Christoforetti JJ, Wolff AB, Nho SJ, Salvo JP Jr et al (2019) The Patient acceptable symptomatic state of the 12-item international hip outcome tool at 1-year follow-up of hip-preservation surgery. Arthroscopy 35:1457–1462
Konan S, Rayan F, Meermans G, Witt J, Haddad FS (2011) Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br 93:332–336
Krych AJ, Kuzma SA, Kovachevich R, Hudgens JL, Stuart MJ, Levy BA (2014) Modest mid-term outcomes after isolated arthroscopic debridement of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc 22:763–767
Larson CM, Giveans MR (2008) Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy 24:540–546
Lin LJ, Akpinar B, Bloom DA, Youm T (2021) Age and outcomes in hip arthroscopy for femoroacetabular impingement: a comparison across 3 age groups. Am J Sports Med 49:82–89
Londers J, Van Melkebeek J (2007) Hip arthroscopy: outcome and patient satisfaction after 5 to 10 years. Acta Orthop Belg 73:478–483
Malviya A, Stafford G, Villar R (2012) Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J Bone Joint Surg Br 94-B:466–470
Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG (2018) Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up. Am J Sports Med 46:1306–1314
Mardones R, Via AG, Rivera A, Tomic A, Somarriva M, Wainer M et al (2016) Arthroscopic treatment of femoroacetabular impingement in patients older than 60 years. Muscles Ligaments Tendons J 6:397–401
Marin-Peña O, Tey-Pons M, Perez-Carro L, Said HG, Sierra P, Dantas P et al (2017) The current situation in hip arthroscopy. EFORT Open Rev 2:58–65
Martin RL, Kivlan BR, Christoforetti JJ, Wolff AB, Nho SJ, Salvo JP Jr et al (2019) Minimal clinically important difference and substantial clinical benefit values for the 12-item international hip outcome tool. Arthroscopy 35:411–416
McCormick F, Nwachukwu BU, Alpaugh K, Martin SD (2012) Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy 28:1359–1364
Meftah M, Rodriguez JA, Panagopoulos G, Alexiades MM (2011) Long-term results of arthroscopic labral debridement: predictors of outcomes. Orthopedics 34:e588-592
Menge TJ, Briggs KK, Dornan GJ, McNamara SC, Philippon MJ (2017) Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: labral debridement compared with labral repair. J Bone Joint Surg Am 99:997–1004
Menge TJ, Briggs KK, Rahl MD, Philippon MJ (2021) Hip arthroscopy for femoroacetabular impingement in adolescents: 10-year patient-reported outcomes. Am J Sports Med 49:76–81
Moon JK, Yoon JY, Kim CH, Lee S, Kekatpure AL, Yoon PW (2020) Hip arthroscopy for femoroacetabular impingement and concomitant labral tears: a minimum 2-year follow-up study. Arthroscopy 36:2186–2194
Mygind-Klavsen B, Kraemer O, Hölmich P, Lund B (2020) An updated description of more than 5,000 procedures from the Danish hip arthroscopy registry. J Bone Joint Surg Am 102:43–50
Mygind-Klavsen B, Lund B, Nielsen TG, Maagaard N, Kraemer O, Hölmich P et al (2019) Danish Hip Arthroscopy Registry: predictors of outcome in patients with femoroacetabular impingement (FAI). Knee Surg Sports Traumatol Arthrosc 27:3110–3120
Nakano N, Khanduja V (2018) Femoroacetabular impingement: the past, current controversies and future perspectives. Phys Sportsmed 46:270–272
Naughton MJ, Anderson RT (1998) Outcomes research in orthopaedics: health-related quality of life and the SF-36. Arthroscopy 14:127–129
Nho SJ, Beck EC, Nwachukwu BU, Cvetanovich GL, Neal WH, Harris JD et al (2019) Survivorship and outcome of hip arthroscopy for femoroacetabular impingement syndrome performed with modern surgical techniques. Am J Sports Med 47:1662–1669
Nielsen TG, Miller LL, Lund B, Christiansen SE, Lind M (2014) Outcome of arthroscopic treatment for symptomatic femoroacetabular impingement. BMC Musculoskelet Disord 15:394. https://doi.org/10.1186/1471-2474-1115-1394
Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS (2017) Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med 45:612–619
Nwachukwu BU, Rebolledo BJ, McCormick F, Rosas S, Harris JD, Kelly BT (2016) Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med 44:1062–1068
Olach M, Gerhard P, Giesinger K, Lampert C, Erhardt JB (2019) Clinical and radiological outcome at mean follow-up of 11 years after hip arthroscopy. Arch Orthop Trauma Surg 139:1–6
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43-B:752–757
Palmer DH, Ganesh V, Comfort T, Tatman P (2012) Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy 28:1671–1681
Philippon MJ, Briggs KK, Carlisle JC, Patterson DC (2013) Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res 471:2492–2496
Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA (2009) Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br 91:16–23
Saltzman BM, Kuhns BD, Basques B, Leroux T, Alter J, Mather RC et al (2017) The influence of body mass index on outcomes after hip arthroscopic surgery with capsular plication for the treatment of femoroacetabular impingement. Am J Sports Med 45:2303–2311
Salvo JP, Nho SJ, Wolff AB, Christoforetti JJ, Van Thiel GS, Ellis TJ et al (2018) Sex-dependent differences in preoperative, radiographic, and intraoperative characteristics of patients undergoing hip arthroscopy: results from the multicenter arthroscopic study of the hip group. Arthroscopy 34:844–852
Sansone M, Ahldén M, Jonasson P, Thomeé C, Swärd L, Collin D et al (2016) Outcome of hip arthroscopy in patients with mild to moderate osteoarthritis-A prospective study. J Hip Preserv Surg 3:61–67
Skendzel JG, Philippon MJ, Briggs KK, Goljan P (2014) The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med 42:1127–1133
Sochacki KR, Jack RA 2nd, Safran MR, Nho SJ, Harris JD (2018) There is a significant discrepancy between “big data” database and original research publications on hip arthroscopy outcomes: a systematic review. Arthroscopy 34:1998–2004
Wilkin G, March G, Beaulé PE (2014) Arthroscopic acetabular labral debridement in patients forty-five years of age or older has minimal benefit for pain and function. J Bone Joint Surg Am 96:113–118
Acknowledgements
NAHR User Group: Marcus J. K. Bankes—University College London Hospitals NHS Foundation Trust, London, England, Tony Andrade—Royal Berkshire NHS Foundation Trust, Reading, England, Tim Board—Wrightington, Wigan and Leigh NHS Foundation Trust, Wigan, England, Jonathon Conroy—Harrogate and District NHS Foundation Trust, Harrogate, England, Matthew Wilson—Royal Devon and Exeter NHS Foundation Trust, Exeter, England, Callum McBryde—The Royal Orthopaedic Hospital NHS Foundation Trust, Birmingham, England.
Funding
RH was supported to undertake this study by grants from Orthopaedic Research UK (ref. 541) and a Royal College of Surgeons of England research fellowship funded through a generous donation from the Shears Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Authors under NAHR User Group are listed in Acknowledgments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Holleyman, R., Sohatee, M., Lyman, S. et al. Hip arthroscopy for femoroacetabular impingement is associated with significant improvement in early patient reported outcomes: analysis of 4963 cases from the UK non-arthroplasty registry (NAHR) dataset. Knee Surg Sports Traumatol Arthrosc 31, 58–69 (2023). https://doi.org/10.1007/s00167-022-07042-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07042-y