Abstract
Purpose
To evaluate the effectiveness of a tailored intervention to reduce low value MRIs and arthroscopies among patients ≥ 50 years with degenerative knee disease in 13 Dutch orthopaedic centers (intervention group) compared with all other Dutch orthopaedic centers (control group).
Methods
All patients with degenerative knee disease ≥ 50 years admitted to Dutch orthopaedic centers from January 2016 to December 2018 were included. The tailored intervention included participation of clinical champions, education on the Dutch Choosing Wisely recommendation for MRI’s and arthroscopies in degenerative knee disease, training of orthopaedic surgeons to manage patient expectations, performance feedback, and provision of a patient brochure. A difference-in-difference analysis was used to compare the time trend before (admitted January 2016–June 2017) and after introduction of the intervention (July 2017–December 2018) between intervention and control hospitals. Primary outcome was the monthly percentage of patients receiving a MRI or knee arthroscopy, weighted by type of hospital.
Results
136,446 patients were included, of whom 32,163 were treated in the intervention hospitals. The weighted percentage of patients receiving a MRI on average declined by 0.15% per month (β = − 0.15, P < 0.001) and by 0.19% per month for arthroscopy (β = − 0.19, P < 0.001). However, these changes over time did not differ between intervention and control hospitals, neither for MRI (β = − 0.74, P = 0.228) nor arthroscopy (β = 0.13, P = 0.688).
Conclusions
The extent to which patients ≥ 50 years with degenerative knee disease received a MRI or arthroscopy declined significantly over time, but could not be attributed to the tailored intervention. This secular downward time trend may reflect anoverall focus of reducing low value care in The Netherlands.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to the ageing population, more people will suffer from degenerative knee disease in the future [23, 48]. Nowadays, around 25% of patients aged 50 years and over experience symptoms of degenerative knee disease [38, 45]. These patients suffer from complaints during walking, climbing stairs and squatting [14, 23]. Some patients also experience locking symptoms: a limited range of motion of the knee due to loose bodies or meniscal tears. Meniscal tears in this age group occur as part of a degenerative process and can be considered a feature of an early stage of osteoarthritis [17, 21].
Since 2014, clinical practice guidelines from professional orthopaedic associations [1, 4, 6, 7] as well as literature on diagnosis and treatment of these patients advise regular weight bearing radiographs including a fixed flexion view (Rosenberg view) to examine the cartilage status of the knee, and non-surgical treatment modalities including pain medication, dietary advice and exercise therapy. Routine use of an MRI for diagnosis of degenerative knee disease is not recommended for this specific patient group due to the poor association with symptoms [13, 20, 21, 32]. Similarly, arthroscopic interventions are not recommended for routine use in degenerative knee disease because limited benefits are found that are absent 1 to 2 years after surgery [16, 27, 28, 39, 40, 43]. Only when locking symptoms are present, a knee arthroscopy may be warranted. As the use of MRI and knee arthroscopy provides limited benefit, require resources and—as for any procedure—may cause harm to the patient [16, 37], both are considered low value care for patients with degenerative knee disease [29, 37].
Nevertheless, many patients are still referred for a MRI or knee arthroscopy for symptomatic degenerative knee complaints [8, 12, 15, 16, 22, 24,25,26, 30, 35, 42, 44]. Smith et al. [41] showed that in Australia knee MRI rates for patients aged 55 years and older increased from 216 per 100 000 to 1509 per 100 000 in 2017. Parent et al. [32] showed that only 38% of patients 50 years and over with degenerative knee disease had a plain radiograph in the 24 months preceding the MRI. Regarding knee arthroscopy, Rietbergen et al. [35] showed that in 2016 35% of knee arthroscopies in the Netherlands was performed without a documented valid surgical indication. Even more important 26% of these arthroscopies were performed on the patient’s request.
To create more awareness and reduce the routine use of MRI and knee arthroscopy in degenerative knee disease, “Choosing Wisely” recommendations were developed in several countries [2, 5, 9, 47]. These are evidence-based recommendations by professional medical specialist societies regarding use of diagnostic tests and surgical procedures. It has been shown that low value care is not reduced by a passive approach of only publishing these “Choosing Wisely” recommendations [36]. Tailored, active, interventions are more likely to succeed in orthopaedic centers that still routinely perform these low value care diagnostics and surgical procedures. The aim of this study is to evaluate the effectiveness of such a tailored intervention to reduce low value MRIs and arthroscopies in patients ≥ 50 years with degenerative knee disease in 13 Dutch orthopaedic centers (intervention group) compared with all other Dutch orthopaedic centers (control group). The hypothesis was that orthopaedic centers receiving the tailored intervention will reduce the use of low value MRI and knee arthroscopy to a greater extent than all other Dutch orthopaedic centers.
Materials and methods
The Medical Ethical Committee (CME P16.190/NV/nv) of the Leiden University Medical Center waived the need for ethical approval for this study under Dutch law. A difference-in-difference design was used to compare the change in time trend before and after introduction of the intervention between intervention and control hospitals. Anonymized patient-level data were extracted from the Dutch National Basic Registration of Hospital Care (LBZ) [3] for all patients aged 50 years and over with knee complaints (Diagnosis Treatment Codes (DTC) 1801–1899) and a closed care trajectory in a Dutch hospital between January 1, 2016 to December 31, 2018. Dutch Hospital Data, the national organization that collects the data from all the hospitals, gave permission to use the anonymized patient data. When a patient visits a hospital the first time for knee complaints, this will generate an initial care trajectory and a follow-up care trajectory if the patient still has complaints within 120 days after the start of this initial care trajectory. All procedures including MRI and arthroscopy are assigned to this care trajectory. Patients with all their diagnostic and surgical procedures carried out in a care trajectory, were assigned to the month at which the trajectory for a specific DTC opened. All patients diagnosed and treated in intervention hospitals were included, except patients from 1 daycare orthopedic private clinic, since those patient data were not collected in the LBZ. The control group existed of patients diagnosed and treated in all other Dutch orthopaedic hospitals providing data to the LBZ in the same period (2016: n = 49; 2017: n = 55, 2018: n = 54).
For each anonymized patient and care trajectory, information was obtained on patient characteristics (age, sex), type of orthopaedic center (University Medical Center, Teaching Hospital, and General Hospital), Diagnosis Treatment Code (1801–1899), group (intervention or control), MRI conducted (yes/no), arthroscopy conducted (yes/no), number of MRIs conducted, number of arthroscopies conducted, month and year care trajectory opened and closed, date of MRI, date of arthroscopy, number of other care trajectories open at that time point, and type of care trajectory (initial or follow-up treatment). It was defined the period January 2016–June 2017 as before the intervention, and July 2017–December 2018 as during/after the intervention. If patients had multiple care trajectories for the same DTC (e.g. for every visit and/or treatment), it is likely that these all belong to the same care path so only the DTC for the last opened care trajectory were then used.
Intervention
A tailored intervention was developed and implemented from July 2017 to February 2018 in the 13 intervention hospitals that participated in the ‘SMART’ (Step-down MRI’s and ARThroscopies) study. This intervention consisted of the following five components that were geared at previously identified barriers and facilitators [33] and based on previous literature were shown to have the greatest potential to reduce low value care (see also box 1):
-
A local clinical leader who encouraged colleagues to follow the clinical practice guidelines (July 2017),
-
Education for orthopaedic surgeons to increase their knowledge about the Dutch Choosing Wisely recommendation (July 2017),
-
Training to improve their skills to manage patient expectations (September 2017),
-
Feedback of performance data to orthopaedic surgeons (September 2017, February 2018), and
-
A patient brochure that professionals could use in their consultations (January 2018).
Outcomes
The primary outcome was the monthly percentage of patients receiving a MRI or knee arthroscopy in their care trajectory. Patients with degenerative knee disease were identified by diagnostic codes: arthrosis (DTC 1801) or meniscus lesion (DTC 1805). As a secondary outcome the monthly percentage of patients aged 50 years and over with a cruciate ligament injury (DTC 1820 and 1830) receiving a MRI or knee arthroscopy was calculated, which was expected not to be influenced by the tailored intervention.
Statistical analysis
Descriptive statistics were used to compare characteristics of patients treated in intervention or control hospitals, stratified by type of hospital (general hospital, teaching hospital, university medical center) as this is known to affect the hospitals’ patient-mix.
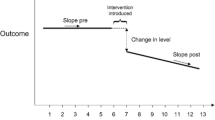
A difference-in-difference approach was used to examine the change in monthly percentage of patients receiving a knee arthroscopy/MRI before and after introduction of the intervention between intervention and control hospitals [19]. The monthly percentage of patients receiving a MRI or knee arthroscopy was therefore also weighted for the distribution across type of hospital. The key assumption for performing a difference-in-difference analysis is a parallel trend, that is a similar time trend before introduction of the intervention for both intervention and control group [19]. This assumption was tested by visual examination and by assessing the significance of the interaction term (time (months) x group (intervention or control group)) before introduction of the intervention, which showed that the assumption was met.
For the difference-in-difference analysis, the following formula was used: weighted monthly % patients receiving a MRI or Arthroscopy = α + β1time + β2introduction + β3group + β4introduction × group, using linear regression analysis. In this equation, time covers 36 months, introduction refers to the period of introduction of the intervention (0 = before introduction of the tailored intervention, 1 = after introduction of the tailored intervention), and group indicates intervention or a control hospital (0 = control, 1 = intervention). The interaction term introduction x group therefore indicates whether the difference before and after introduction of the intervention differed between intervention and control hospitals. The same analyses were carried out for the secondary outcome in cruciate ligament injured patients, to assess whether there was a change in use of MRI or arthroscopy for a patient group not targeted by the intervention.
Since the components of the intervention were implemented over a period of time, these may not all have resulted in an immediate effect. Sensitivity analyses were therefore employed assuming different lag periods after the introduction of the intervention in July 2017 to account for the time it takes an intervention to affect care delivery: 3 months, 6 months, and 8 months. In addition, sensitivity analyses were performed excluding patients with a start of the initial care trajectory before January 2016, and excluding patients with a start of the initial care trajectory in November–December 2018. These analyses were done since only partial care trajectories might have been included in the data, resulting in missing MRIs or arthroscopies. All analyses were carried out with R statistics (version 3.6.2). A p value < 0.05 was considered significant in all analyses.
Results
215,293 records for patients ≥ 50 years and over with degenerative knee disease were identified, which involved 136,446 patients with a care trajectory. Table 1 shows that patients did not differ in age, but that there was a difference in the distribution of sex, % DTC 1801, and % of multiple DTCs per patient between intervention and control hospitals stratified by hospital type.
Figures 1 and 2 show the observed time trends in weighted monthly percentage of patients receiving MRI or arthroscopy respectively, for intervention and control hospitals with the vertical line indicating the start of the intervention. The results of the difference-in-difference analysis based on these time series data, are shown in Table 2a and b for use of MRI and arthroscopy respectively. The variable time is significant in both tables, as also apparent in the figures, indicating a secular declining trend of 0.15% per month in percentage of patients receiving a MRI and 0.19% per month for arthroscopy i.e. 5.4% and 6.8% fewer patients receiving MRI and arthroscopy during the study period. The variable group is also significant in both tables, indicating that intervention hospitals on average had lower percentages of patients receiving MRI/arthroscopy than control hospitals (0.86% lower for MRI and 0.83% lower for arthroscopy, also shown in Figs. 1 and 2 with the lines for intervention hospitals consistently lower than control hospitals. The interaction term introduction x group is the variable of interest to show the effect of the intervention, which is non-significant meaning that the change in percentage of patients receiving a MRI or arthroscopy before and after the introduction of the intervention, did not differ significantly between intervention and control group. In other words, the intervention did not significantly change the time trend in intervention hospitals beyond what already occurred elsewhere.
These analyses were repeated for patients with a cruciate ligament injury (diagnosis code 1820/1830) who were not targeted by the intervention (Appendix A). Again, a significant reduction in patients receiving a MRI was shown of 0.29% per month, but was non-significant for arthroscopy. As expected because the intervention was not targeted at these patients, no effect of the intervention was found as shown by the non-significant interaction term (introduction x group).
Sensitivity analyses for the different lag periods (3, 6, and 8 months) showed similar results (Appendix B and C). Other sensitivity analyses excluding patients with a DTC open before January 2016 and excluding patients with a DTC open in November 2018 or December 2018, also showed similar results (data not shown).
Discussion
The most important finding of the present study was that a secular time trend reduced the weighted monthly percentage of patients with degenerative knee disease receiving a MRI and arthroscopy across both intervention and the control hospitals. The tailored intervention designed to reduce low value care did not further reduce the percentage of patients receiving a MRI or arthroscopy.
Previous research has shown that de-implementation of low value care in orthopaedic surgery is challenging and that providing a substitute will likely be more effective than doing nothing [46]. This might explain the lack of an effect in the present study, as no clear substitute was provided as part of the intervention, although the orthopaedic surgeons could offer patients non-surgical treatments, like advice on possible weight loss in overweight patients, physical exercises, short periods of pain killers and even adequate explanation for the presence of the knee symptoms. That substitution may be more effective is also supported by the recent study of Barlow et al. who showed that providing a substitute conservative care pathway rather than knee arthroscopy is able to reduce low value knee arthroscopies [11]. However, the study of Barlow did not use a control group, so that the observed reduction may have been part of a secular trend. Therefore, more research is needed to investigate the effectiveness of such substitute interventions.
Increasing awareness among clinicians has been shown previously to result in changes in clinical practice, particularly for issues receiving widespread attention. For instance, Kiadaliri et al. [26] showed that the development of national guideline’s recommendation against the use of knee arthroscopy in patients with knee osteoarthritis was associated with a decrease in knee arthroscopy in Sweden. In addition, Reeves et al. [33] showed, that clinical practice change occurred even before actual findings of orthopaedic trials were published. The latter phenomenon is known as the ‘rising tide’ [18] i.e. a pronounced secular trend created by social responses to a particular issue which has gained widespread attention. The current study could be another example of changing overall awareness regarding non-indicated procedures, substantiated by the growing number of studies published about the non-indicated use of MRI and arthroscopy [8, 12, 15, 16, 22, 24, 26, 30, 31, 35, 42, 44] as well as by discussions about the Dutch guideline for knee arthroscopy at meetings of the Netherlands Orthopaedic Association from 2017 onwards and the dissemination of (inter)national clinical guidelines.
Other studies have identified additional barriers that may influence decisions around performing MRI or arthroscopy, which may have been insufficiently addressed with the tailored intervention in the present study. Barlow et al. [10] found, for example, that the desire to help patients and to meet their expectations, the belief that those expectations did not involve non-surgical treatment modalities, time pressure in de clinic, and a perceived (or real) pressure from patients for an arthroscopy, were substantial barriers for reducing the use of arthroscopy in knee osteoarthritis. For the Netherlands, Rietbergen et al. have previously shown relevant barriers and facilitators for reducing the use of knee arthroscopy in degenerative knee disease which informed the intervention in the present study [34]. These barriers included orthopedic surgeons’ beliefs in the added value of MRI’s and knee arthroscopies as well as positive experiences with MRI’s and knee arthroscopies among friends and family in the patient’s environment, which both may influence the decision making for MRI and arthroscopy [34].
A strength of this study is that to a control group was included to take into account any secular time trends and separate this for the intervention effect. In the absence of such a control group, the change over time might be incorrectly attributed to the introduction of the intervention, as may have been the case in previous studies [11]. However, there are also some limitations that should be noted. First, the percentage of patients with a low value MRI or arthroscopy may have been overestimated, as in some patients there may be a valid reason for a MRI or knee arthroscopy (e.g., a truly locked knee; an extension limitation of the knee due to an intra-articular blockage) [33], which cannot be deducted from the administrative data that were used in this study. Secondly, data of orthopaedic private clinics were not available in the LBZ database so the results of this study cannot be generalized to these centers. However, a previous study [35] showed that these orthopaedic private clinics perform low value care in this patient group comparable to other hospitals. Thus it is likely that they will have been influenced by the same time trend observed in all other Dutch hospitals.
The findings of this study emphasize that it is unclear when additional quality improvement interventions are needed to reduce low value care, and when the ‘rising-tide’ phenomenon is enough to increase awareness and to implement new insights from trials or guideline recommendations. More qualitative research is needed to gain further insight into the ‘rising tide’ phenomenon, identifying when interventions are needed to de-implement low value care. Based on the findings of the study, orthopaedic surgeons are advised to improve their care by considering for which patients MRI or arthroscopy has limited value and by explaining to patients why MRI or arthroscopy has limited value, potentially supported by patient brochures.
Conclusions
This study showed that the weighted monthly percentage of patients ≥ 50 years with degenerative knee disease who receive a MRI or arthroscopy was reduced across both intervention and control hospitals as part of a secular trend. The tailored intervention did not have an additional effect beyond this secular downward time trend.
References
Arthroscopy of the knee (in dutch) (2019) https://richtlijnendatabase.nl/richtlijn/artroscopie_van_de_knie/startpagina_-_artroscopie_van_de_knie.html.
Australian Rheumatology Association: tests, treatments and procedures clinicians and consumers should question (2018) http://www.choosingwisely.org.au/recommendations/ara.
DHD. Landelijke basisregistratie ziekenhuiszorg (LBZ). https://www.dhd.nl/producten-diensten/lbz/paginas/dataverzameling-lbz.aspx Accessed October 2019.
ESSKA meniscus consensus project: degenerative meniscus lesions (2016) https://cdn.ymaws.com/www.esska.org/resource/resmgr/Docs/2016-meniscus-consensus-proj.pdf.
Orthopaedics: ten things physicians and patients should question (2018) https://choosingwiselycanada.org/orthopaedics/.
Osteoarthritis: care and management (2014) https://www.nice.org.uk/guidance/cg177.
VA/DoD clinical practice guideline for the non-surgical management of hip and knee osteoarthritis (2014) https://www.healthquality.va.gov/guidelines/CD/OA/VADoDOACPGFINAL090214.pdf.
Adelani MA, Harris AH, Bowe TR, Giori NJ (2016) Arthroscopy for knee osteoarthritis has not decreased after a clinical trial. Clin Orthop Relat Res 474:489–494
Al Sayah F, Williams B, Pederson JL, Majumdar SR, Johnson JA (2014) Health literacy and nurses’ communication with type 2 diabetes patients in primary care settings. Nurs Res 63:408–417
Barlow T, Plant CE (2015) Why we still perform arthroscopy in knee osteoarthritis: a multi-methods study. BMC Musculoskelet Disord 16:85. https://doi.org/10.1186/s12891-015-0537-y
Barlow T, Rhodes-Jones T, Ballinger S, Metcalfe A, Wright D, Thompson P (2020) Decreasing the number of arthroscopies in knee osteoarthritis—a service evaluation of a de-implementation strategy. BMC Musculoskelet Disord 21:140. https://doi.org/10.1186/s12891-020-3125-8
Bergkvist D, Dahlberg LE, Neuman P, Englund M (2016) Knee arthroscopies: who gets them, what does the radiologist report, and what does the surgeon find? An evaluation from southern Sweden. Acta Orthop 87:12–16
Bhattacharyya TMD, Gale DMD, Dewire PMD, Totterman SMD, Gale MEMD, McLaughlin SMPH et al (2003) The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am 85:4–9
Bijlsma JW, Berenbaum F, Lafeber FP (2011) Osteoarthritis: an update with relevance for clinical practice. Lancet 377:2115–2126
Bohensky MA, Sundararajan V, Andrianopoulos N, de Steiger RN, Bucknill A, Kondogiannis CM et al (2012) Trends in elective knee arthroscopies in a population-based cohort, 2000–2009. Med J Aust 197:399–403
Brignardello-Petersen R, Guyatt GH, Buchbinder R, Poolman RW, Schandelmaier S, Chang Y et al (2017) Knee arthroscopy versus conservative management in patients with degenerative knee disease: a systematic review. BMJ Open 7:e016114. https://doi.org/10.1136/bmjopen-2017-016114
Buchbinder R, Harris IA, Sprowson A (2015) Management of degenerative meniscal tears and the role of surgery. BMJ 350:h2212. https://doi.org/10.1136/bmj.h2212
Chen YF, Hemming K, Stevens AJ, Lilford RJ (2016) Secular trends and evaluation of complex interventions: the rising tide phenomenon. BMJ Qual Saf 25:303–310
Dimick JB, Ryan AM (2014) Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA 312:2401–2402
Englund M (2008) The role of the meniscus in osteoarthritis genesis. Rheum Dis Clin North Am 34:573–579
Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M et al (2008) Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med 359:1108–1115
Hamilton DF, Howie CR (2015) Knee arthroscopy: influence of systems for delivering healthcare on procedure rates. BMJ 351:h4720. https://doi.org/10.1136/bmj.h4720
Hunter DJ, Bierma-Zeinstra S (2019) Osteoarthritis. Lancet 393:1745–1759
Jarvinen TL, Guyatt GH (2016) Arthroscopic surgery for knee pain. BMJ 354:i3934. https://doi.org/10.1136/bmj.i3934
Khatri C, Dickenson E, Ahmed I, Bretherton C, Ranaboldo T, Shaw C et al (2021) ARthroscopy in Knee OsteoArthritis (ARK-OA): a multicentre study assessing compliance to national guidelines. Eur J Orthop Surg Traumatol 31:1443–1449
Kiadaliri A, Bergkvist D, Dahlberg LE, Englund M (2019) Impact of a national guideline on use of knee arthroscopy: an interrupted time-series analysis. Int J Qual Health Care 31:G113–G118
Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM (2016) Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ 354:i3740. https://doi.org/10.1136/bmj.i3740
MacFarlane LA, Yang H, Collins JE, Brophy RH, Cole BJ, Spindler KP et al (2021) Association between baseline “Meniscal symptoms” and outcomes of operative and non-operative treatment of meniscal tear in patients with osteoarthritis. Arthritis Care Res (Hoboken). https://doi.org/10.1002/acr.24588
Miller G, Rhyan C, Beaudin-Seiler B, Hughes-Cromwick P (2018) A framework for measuring low-value care. Value Health 21:375–379
Muheim LLS, Senn O, Fruh M, Reich O, Rosemann T, Neuner-Jehle SM (2017) Inappropriate use of arthroscopic meniscal surgery in degenerative knee disease. Acta Orthop 88:550–555
Parent ME, Vezina F, Carrier N, Masetto A (2018) Indications for and clinical procedures resulting from magnetic resonance imaging of the knee in older patients: are we choosing wisely? Can Fam Phys 64:e126–e132
Parent ME, Vézina F, Carrier N, Masetto A (2018) Indications for and clinical procedures resulting from magnetic resonance imaging of the knee in older patients: are we choosing wisely? Can Fam Phys 64:e126–e132
Reeves K, Chan S, Marsh A, Gallier S, Wigley C, Khunti K et al (2020) Implementation of research evidence in orthopaedics: a tale of three trials. BMJ Qual Saf 29:374–381
Rietbergen T, Diercks RL, Anker-van der Wel I, van den Akker-van Marle ME, Lopuhaa N, Janssen RPA et al (2019) Preferences and beliefs of Dutch orthopaedic surgeons and patients reduce the implementation of “Choosing Wisely” recommendations in degenerative knee disease. Knee Surg Sports Traumatol Arthrosc 28:3101–3117
Rietbergen T, Marang-van de Mheen PJ, Diercks RL, Janssen RPA, van der Linden-van der Zwaag HMJ, Nelissen R et al (2021) Performing a knee arthroscopy among patients with degenerative knee disease: one-third is potentially low value care. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06615-7
Rosenberg A, Agiro A, Gottlieb M, Barron J, Brady P, Liu Y et al (2015) Early trends among seven recommendations from the choosing wisely campaign. JAMA Intern Med 175:1913–1920
Scott IA, Duckett SJ (2015) In search of professional consensus in defining and reducing low-value care. Med J Aust 203:179–181
Siemieniuk RAC, Harris IA, Agoritsas T, Poolman RW, Brignardello-Petersen R, Van de Velde S et al (2017) Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ 357:j1982. https://doi.org/10.1136/bmj.j1982
Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Kalske J et al (2020) Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br J Sports Med 54:1332–1339
Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H et al (2013) Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 369:2515–2524
Smith L, Barratt A, Buchbinder R, Harris IA, Doust J, Bell K (2020) Trends in knee magnetic resonance imaging, arthroscopies and joint replacements in older Australians: still too much low-value care? ANZ J Surg. https://doi.org/10.1111/ans.15712
Thorlund JB, Hare KB, Lohmander LS (2014) Large increase in arthroscopic meniscus surgery in the middle-aged and older population in Denmark from 2000 to 2011. Acta Orthop 85:287–292
Thorlund JB, Juhl CB, Roos EM, Lohmander LS (2015) Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. Br J Sports Med 49:1229–1235
Tornow K, Chalian M, Zerr J, Moore D, Thropp R, Xi Y et al (2019) A quality improvement project to reduce unnecessary knee mri for chronic degenerative changes. J Am Coll Radiol 16:940–944
Turkiewicz A, Gerhardsson de Verdier M, Engstrom G, Nilsson PM, Mellstrom C, Lohmander LS et al (2015) Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology (Oxford) 54:827–835
Voorn VMA, Marang-van de Mheen PJ, van der Hout A, Hofstede SN, So-Osman C, van den Akker-van Marle ME et al (2017) The effectiveness of a de-implementation strategy to reduce low-value blood management techniques in primary hip and knee arthroplasty: a pragmatic cluster-randomized controlled trial. Implement Sci 12:72. https://doi.org/10.1186/s13012-017-0601-0
Wisely C (2019) American medical society for sports medicine: five things physicians and patients should question. http://www.choosingwisely.org/societies/american-medical-society-for-sports-medicine/.
Zhang W, Doherty M, Peat G, Bierma-Zeinstra MA, Arden NK, Bresnihan B et al (2010) EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 69:483–489
Acknowledgements
We would like to acknowledge all hospitals that participated in the SMART study (alphabetically): Amphia, Breda; Antonius Ziekenhuis, location Sneek; Deventer Ziekenhuis, Deventer; Elisabeth-TweeSteden Ziekenhuis (ETZ), location Tilburg; Franciscus Gasthuis, Rotterdam; ICONE, Schijndel; Leids Universitair Medisch Centrum (LUMC), Leiden; Medisch Centrum Leeuwarden (MCL), Leeuwarden; Medisch Spectrum Twente, location Enschede; Noordwest Ziekenhuisgroep, location Alkmaar; OCON Orthopedische Kliniek, location Hengelo; TerGooi, Hilversum and Blaricum; Universitair Medisch Centrum Groningen (UMCG), Groningen. SMART study group: P. Pander, MD, Department of Orthopaedic Surgery, Northwest clinics orthopaedic department, Alkmaar, the Netherlands. D. J. Hofstee, MD, Department of Orthopaedic Surgery, Northwest clinics orthopaedic department, Alkmaar, the Netherlands. R. C. I. van Geenen, MD, PhD, Department of Orthopaedic Surgery, Amphia Hospital, Breda, the Netherlands. K. L. M. Koenraadt, Foundation for orthopedic research, care & education (FORCE), Amphia Hospital, Breda, the Netherlands. J. P. A. H. Onderwater, MD, Department of Orthopaedic Surgery, Antonius Zorggroep, Sneek/Emmeloord, the Netherlands. Y. V. Kleinlugtenbelt, MD, PhD, Department of Orthopaedic Surgery, Deventer Hospital, Deventer, the Netherlands. T. Gosens, MD, PhD, Department of Orthopaedic Surgery, Elisabeth-Tweesteden Hospital, Tilburg, the Netherlands. T. V. S. Klos, MD, PhD, Department of Orthopaedic Surgery, ICONE, Schijndel, the Netherlands. P. C. Rijk, MD, PhD, Department of Orthopaedic Surgery, Medical Center Leeuwarden, Leeuwarden, the Netherlands. B. Dijkstra, MSc, Department of Orthopaedic Surgery, Medical Center Leeuwarden, Leeuwarden, the Netherlands. A. V. C. M. Zeegers, MD, PhD, Department of Orthopaedic Surgery, Medisch Spectrum Twente, Enschede, the Netherlands. R. A. G. Hoogeslag, MD, Department of Orthopaedic Surgery, OCON, Hengelo, the Netherlands. M. H. A. Huis in’t Veld, PhD, Department of Orthopaedic Surgery, OCON, Hengelo, the Netherlands. A. A. Polak, MD, Department of Orthopaedic Surgery, Franciscus Gasthuis, Rotterdam, the Netherlands. N. R. Paulino Pereira, MD, PhD, Department of Orthopaedic Surgery, TerGooi Hospital, Hilversum, the Netherlands. T. M. J. S. Vervest, Department of Orthopaedic surgery, Tergooi Hospital, Hilversum, the Netherlands. H. C. van der Veen, MD, PhD, Department of Orthopaedics, University Medical Center Groningen, Groningen, the Netherlands. N. Lopuhaä, ReumaNederland, Amsterdam, The Netherlands.
Funding
This study is funded by the Netherlands Organization for Health Research and Development (ZonMw) grant 8392010022. They have no role in the study design or analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The Medical Ethical Committee (CME P16.190/NV/nv) of the Leiden University Medical Center waived the need for ethical approval for this study under Dutch law.
Informed consent
For this type of article, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of SMART study group are listed in acknowledgements.
Appendix
Appendix
Appendix A: difference-in-difference analysis MRI and arthroscopy for 1820/1830
Table 3.
Appendix B: sensitivity analyses MRI for different lag periods (3, 6, and 8 months)
Table 4.
Appendix C: sensitivity analyses Arthroscopy for different lag periods (3, 6, and 8 months)
Table 5.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rietbergen, T., Marang-van de Mheen, P.J., de Graaf, J. et al. A tailored intervention does not reduce low value MRI’s and arthroscopies in degenerative knee disease when the secular time trend is taken into account: a difference-in-difference analysis. Knee Surg Sports Traumatol Arthrosc 30, 4134–4143 (2022). https://doi.org/10.1007/s00167-022-06949-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06949-w