Abstract
Background
No previous study has evaluated the MCID for revision total knee arthroplasty (TKA). This study aimed to identify the MCID for the Knee Society Score (KSS), for revision TKA.
Methods
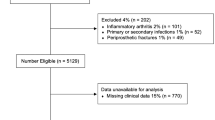
Prospectively collected data from 270 patients who underwent revision TKA at a single institution was analysed. Clinical assessment was performed preoperatively, at 6 months and 2 years using Knee Society Function Score (KSFS) and Knee (KSKS) Scores, and Oxford Knee Score (OKS). MCID was evaluated with a three-pronged methodology, using (1) anchor-based method with linear regression, (2) anchor-based method with receiver operating characteristic (ROC) and area under curve (AUC), (3) distribution-based method with standard deviation (SD). The anchors used were improvement in OKS ≥ 5, patient satisfaction, and implant survivorship following revision TKA.
Results
The cohort comprised 70% females, with mean age of 69.0 years, that underwent unilateral revision TKA. The MCID determined by anchor-based linear regression method using OKS was 6.3 for KSFS, and 6.6 for KSKS. The MCID determined by anchor-based ROC was between 15 and 20 for KSFS (AUC: satisfaction = 71.8%, survivorship = 61.4%) and between 33 and 34 for KSKS (AUC: satisfaction = 76.3%, survivorship = 67.1%). The MCID determined by distribution-based method of 0.5 SD was 11.7 for KSFS and 11.9 for KSKS.
Conclusion
The MCID of 6.3 points for KSFS, and 6.6 points for KSKS, is a useful benchmark for future studies looking to compare revision against primary TKA outcomes. Clinically, the MCID between 15 and 20 for KSFS and between 33 and 34 for KSKS is a powerful tool for discriminating patients with successful outcomes after revision TKA. Implant survivorship is an objective and naturally dichotomous outcome measure that complements the subjective measure of patient satisfaction, which future MCID studies could consider utilizing as anchors in ROC.
Level of evidence
II.




Similar content being viewed by others
References
Angst F, Aeschlimann A, Angst J (2017) The minimal clinically important difference raised the significance of outcome effects above the statistical level, with methodological implications for future studies. J Clin Epidemiol 82:128–136
Anthoine E, Moret L, Regnault A, Sébille V, Hardouin JB (2014) Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes 12:176
Ares O, Castellet E, Maculé F, León V, Montañez E, Freire A et al (2013) Translation and validation of ‘The Knee Society Clinical Rating System’ into Spanish. Knee Surg Sports Traumatol Arthrosc 21:2618–2624
Baker P, Cowling P, Kurtz S, Jameson S, Gregg P, Deehan D (2012) Reason for revision influences early patient outcomes after aseptic knee revision. Clin Orthop Relat Res 470:2244–2252
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ (2007) The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 89:893–900
Beard DJ, Harris K, Dawson J, Doll H, Murray DW, Carr AJ et al (2015) Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 68:73–79
Bin Abd Razak HR, Tan CS, Chen YJ, Pang HN, Tay KJ, Chin PL et al (2016) Age and preoperative knee society score are significant predictors of outcomes among Asians following total knee arthroplasty. J Bone Joint Surg Am 98:735–741
Boelch SP, Jakuscheit A, Doerries S, Fraissler L, Hoberg M, Arnholdt J et al (2018) Periprosthetic infection is the major indication for TKA revision–experiences from a university referral arthroplasty center. BMC Musculoskelet Disord 19:395
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Çelik D, Çoban Ö, Kılıçoğlu Ö (2019) Minimal clinically important difference of commonly used hip-, knee-, foot-, and ankle-specific questionnaires: a systematic review. J Clin Epidemiol 113:44–57
Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD (2017) Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee 24:179–190
Chesworth BM, Mahomed NN, Bourne RB, Davis AM (2008) Willingness to go through surgery again validated the WOMAC clinically important difference from THR/TKR surgery. J Clin Epidemiol 61:907–918
Choi HR, Bedair H (2014) Mortality following revision total knee arthroplasty: a matched cohort study of septic versus aseptic revisions. J Arthroplasty 29:1216–1218
Clement ND, MacDonald D, Simpson AH (2014) The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:1933–1939
Clement ND, Weir D, Holland J, Gerrand C, Deehan DJ (2019) Meaningful changes in the Short Form 12 physical and mental summary scores after total knee arthroplasty. Knee 26:861–868
Cleveland O, Piuzzi NS, Strnad G, Brooks P, Hettrich CM, Higuera-Rueda C et al (2019) Implementing a scientifically valid, cost-effective, and scalable data collection system at point of care: the Cleveland Clinic OME Cohort. J Bone Joint Surg Am 101:458–464
Cohen J (2013) Statistical power analysis for the behavioral sciences. Academic press, Cambridge
Copay AG, Eyberg B, Chung AS, Zurcher KS, Chutkan N, Spangehl MJ (2018) Minimum clinically important difference: current trends in the orthopaedic literature, part ii: lower extremity: a systematic review. JBJS Rev 6:e2
Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC (2007) Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 7:541–546
Dawson J, Beard DJ, McKibbin H, Harris K, Jenkinson C, Price AJ (2014) Development of a patient-reported outcome measure of activity and participation (the OKS-APQ) to supplement the Oxford knee score. Bone Joint J 96B:332–338
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Dowsey MM, Choong PF (2013) The utility of outcome measures in total knee replacement surgery. Int J Rheumatol 2013:506518
Escobar A, García Pérez L, Herrera-Espiñeira C, Aizpuru F, Sarasqueta C, Sáenz G, de Tejada M et al (2013) Total knee replacement; minimal clinically important differences and responders. Osteoarthr Cartil 21:2006–2012
Escobar A, Quintana JM, Bilbao A, Aróstegui I, Lafuente I, Vidaurreta I (2007) Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthr Cartil 15:273–280
Goh GS, Khow YZ, Tay DK, Lo NN, Yeo SJ, Liow MHL (2021) Preoperative mental health influences patient-reported outcome measures and satisfaction after revision total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2021.03.026
Greidanus NV, Peterson RC, Masri BA, Garbuz DS (2011) Quality of life outcomes in revision versus primary total knee arthroplasty. J Arthroplasty 26:615–620
Hartley RC, Barton-Hanson NG, Finley R, Parkinson RW (2002) Early patient outcomes after primary and revision total knee arthroplasty. A prospective study. J Bone Joint Surg Br 84:994–999
Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R et al (1998) Health-related quality of life after knee replacement. J Bone Joint Surg Am 80:163–173
Ingelsrud LH, Roos EM, Terluin B, Gromov K, Husted H, Troelsen A (2018) Minimal important change values for the Oxford Knee Score and the Forgotten Joint Score at 1 year after total knee replacement. Acta Orthop 89:541–547
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jaeschke R, Singer J, Guyatt GH (1989) Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials 10:407–415
Jayadevappa R, Cook R, Chhatre S (2017) Minimal important difference to infer changes in health-related quality of life–a systematic review. J Clin Epidemiol 89:188–198
King MT (2011) A point of minimal important difference (MID): a critique of terminology and methods. Expert Rev Pharmacoecon Outcomes Res 11:171–184
Kiran A, Bottomley N, Biant LC, Javaid MK, Carr AJ, Cooper C et al (2015) Variations in good patient reported outcomes after total knee arthroplasty. J Arthroplasty 30:1364–1371
Kiran A, Hunter DJ, Judge A, Field RE, Javaid MK, Cooper C et al (2014) A novel methodological approach for measuring symptomatic change following total joint arthroplasty. J Arthroplasty 29:2140–2145
Lee WC, Kwan YH, Chong HC, Yeo SJ (2017) The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc 25:3354–3359
Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB (2001) Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am 83:1856–1864
Lizaur-Utrilla A, Gonzalez-Parreño S, Martinez-Mendez D, Miralles-Muñoz FA, Lopez-Prats FA (2020) Minimal clinically important differences and substantial clinical benefits for Knee Society Scores. Knee Surg Sports Traumatol Arthrosc 28:1473–1478
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5:1315–1316
Maradit Kremers H, Kremers WK, Berry DJ, Lewallen DG (2017) Patient-reported outcomes can be used to identify patients at risk for total knee arthroplasty revision and potentially individualize postsurgery follow-up. J Arthroplasty 32:3304–3307
Maratt JD, Lee YY, Lyman S, Westrich GH (2015) Predictors of satisfaction following total knee arthroplasty. J Arthroplasty 30:1142–1145
Maredupaka S, Meshram P, Chatte M, Kim WH, Kim TK (2020) Minimal clinically important difference of commonly used patient-reported outcome measures in total knee arthroplasty: review of terminologies, methods and proposed values. Knee Surg Relat Res 32:19
McLawhorn AS, Buller LT (2017) Bundled payments in total joint replacement: keeping our care affordable and high in quality. Curr Rev Musculoskelet Med 10:370–377
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ et al (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89:1010–1014
Nilsdotter AK, Toksvig-Larsen S, Roos EM (2009) A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthr Cartil 17:601–606
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41:582–592
Page P (2014) Beyond statistical significance: clinical interpretation of rehabilitation research literature. Int J Sports Phys Ther 9:726–736
Piuzzi NS (2020) Patient-reported outcome measures (pain, function, and quality of life) after aseptic revision total knee arthroplasty. J Bone Joint Surg Am 102:114
Quintana JM, Escobar A, Arostegui I, Bilbao A, Azkarate J, Goenaga JI et al (2006) Health-related quality of life and appropriateness of knee or hip joint replacement. Arch Intern Med 166:220–226
Revicki D, Hays RD, Cella D, Sloan J (2008) Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol 61:102–109
Rolfson O, Bohm E, Franklin P, Lyman S, Denissen G, Dawson J et al (2016) Patient-reported outcome measures in arthroplasty registries Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop 87(Suppl 1):9–23
Silva AL, Demange MK, Gobbi RG, da Silva TF, Pécora JR, Croci AT (2012) Translation and Validation of the Knee Society Score - KSS for Brazilian Portuguese. Acta Ortop Bras 20:25–30
Squitieri L, Bozic KJ, Pusic AL (2017) The role of patient-reported outcome measures in value-based payment reform. Value Health 20:834–836
Tande A, Asante D, Sangaralingham L, Osmon D, Heien H, Mabry T, et al (2017) Risk factors for early hip or knee prosthetic joint infection (PJI): analysis of a Nationwide American Insurance Claims Dataset. Paper presented at: Open Forum Infectious Diseases 2017
Terwee CB, Roorda LD, Dekker J, Bierma-Zeinstra SM, Peat G, Jordan KP et al (2010) Mind the MIC: large variation among populations and methods. J Clin Epidemiol 63:524–534
U.S. Department of Health and Human Services (2006) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes 4:79
van Schie P, van Steenbergen LN, van Bodegom-Vos L, Nelissen R, Marang-van de Mheen PJ (2020) Between-hospital variation in revision rates after total hip and knee arthroplasty in the Netherlands: directing quality-improvement initiatives. J Bone Joint Surg Am 102:315–324
Verbeek JFM, Hannink G, Defoort KC, Wymenga AB, Heesterbeek PJC (2019) Age, gender, functional KSS, reason for revision and type of bone defect predict functional outcome 5 years after revision total knee arthroplasty: a multivariable prediction model. Knee Surg Sports Traumatol Arthrosc 27:2289–2296
Wells G, Beaton D, Shea B, Boers M, Simon L, Strand V et al (2001) Minimal clinically important differences: review of methods. J Rheumatol 28:406–412
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
YZK (Medical Student): conceptualized the study, performed the methodology, validation, and statistical analysis, wrote, reviewed, and edited the manuscript. MHLL (Orthopaedic Surgeon): conceptualized and supervised the study, performed the methodology, wrote, reviewed, and edited the manuscript. GSG (Orthopaedic Surgeon): supervised the study, wrote, reviewed, and edited the manuscript. JYQC (Orthopaedic Surgeon): supervised the study, reviewed the manuscript. NNL (Orthopaedic Surgeon): supervised the study, reviewed the manuscript. SJY (Orthopaedic Surgeon): supervised the study, reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
Ethical approval for this study was obtained from the SingHealth Centralized Institution Review Board (CIRB 2020/2237).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khow, Y.Z., Liow, M.H.L., Goh, G.S. et al. Defining the minimal clinically important difference for the knee society score following revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30, 2744–2752 (2022). https://doi.org/10.1007/s00167-021-06628-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06628-2