Abstract
Purpose
Medial patellofemoral ligament reconstruction (MPFLR) is often indicated in athletes with lateral patellar instability to prevent recurrence and allow for a successful return to play. In this patient population, the ability to return to play is one of the most important clinical outcomes. The purpose of the current study was to analyze the characteristics of patients who were unable return to play following MPFL reconstruction.
Methods
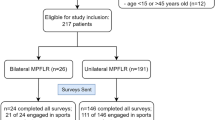
A retrospective review of patients who underwent MPFL reconstruction and subsequently did not return to play after a minimum of 12-months of follow-up was performed. Patients were evaluated for their psychological readiness to return to sport using the MPFL-Return to Sport after Injury (MPFL-RSI) score, which is a modification of the ACL-RSI score. A MPFL-RSI score > 56 is considered a passing score for being psychologically ready to return to play. Additionally, reasons for not returning to play including Visual Analog Scale for pain (VAS), Kujala score, satisfaction, and recurrent instability (including dislocations and subluxations) were evaluated.
Results
The study included a total of 35 patients who were unable to return to play out of a total cohort of 131 patients who underwent MPFL reconstruction as treatment for patellar instability. Overall, 60% were female with a mean age of 24.5, and a mean follow-up of 38 months. Nine patients (25.7%) passed the MPFL-RSI benchmark of 56 with a mean overall score of 44.2 ± 21.8. The most common primary reasons for not returning to play were 14 were afraid of re-injury, 9 cited other lifestyle factors, 5 did not return due to continued knee pain, 5 were not confident in their ability to perform, and 2 did not return due to a feeling of instability. The mean VAS score was 1.9 ± 2.3, the mean Kujala score was 82.5 ± 14.6, and the mean satisfaction was 76.9%. Three patients (8.7%) reported experiencing a patellar subluxation event post-operatively. No patient sustained a post-operative patellar dislocation.
Conclusion
Following MPFL reconstruction, patients that do not return to play exhibit poor psychological readiness with the most common reason being fear of re-injury.
Level of evidence
IV.
Similar content being viewed by others
References
Ambra LF, Franciozi CE, Phan A, Faloppa F, Gomoll AH (2020) Isolated MPTL reconstruction fails to restore lateral patellar stability when compared to MPFL reconstruction. Knee Surg Sports TraumatolArthrosc. https://doi.org/10.1007/s00167-020-06015-3
Boelch SP, Gurok A, Gilbert F, Weissenberger M, Rudert M, Barthel T et al (2021) Why compromise the patella? Five-year follow-up results of medial patellofemoral ligament reconstruction with soft tissue patellar fixation. IntOrthop. https://doi.org/10.1007/s00264-020-04922-1
Chahla J, Smigielski R, LaPrade RF, Fulkerson JP (2019) An updated overview of the anatomy and function of the proximal medial patellar restraints (medial patellofemoral ligament and the medial quadriceps tendon femoral ligament). Sports Med Arthrosc Rev 27:136–142
Chouteau J (2016) Surgical reconstruction of the medial patellofemoral ligament. Orthop Traumatol Surg Res 102:S189–S194
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Feucht MJ, Mehl J, Forkel P, Achtnich A, Schmitt A, Izadpanah K et al (2020) Failure analysis in patients with patellar redislocation after primary isolated medial patellofemoral ligament reconstruction. Orthop J Sports Med 8:2325967120926178
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Forsdyke D, Smith A, Jones M, Gledhill A (2016) Psychosocial factors associated with outcomes of sports injury rehabilitation in competitive athletes: a mixed studies systematic review. Br J Sports Med 50:537–544
Gerometta A, Klouche S, Herman S, Lefevre N, Bohu Y (2018) The Shoulder Instability-Return to Sport after Injury (SIRSI): a valid and reproducible scale to quantify psychological readiness to return to sport after traumatic shoulder instability. Knee Surg Sports TraumatolArthrosc 26:203–211
Johnson DS, Turner PG (2019) Management of the first-time lateral patellar dislocation. Knee 26:1161–1165
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L (2007) The anatomy of the medial part of the knee. J Bone JtSurg Am 89:2000–2010
Lee DY, Park YJ, Song SY, Hwang SC, Park JS, Kang DG (2018) Which technique is better for treating patellar dislocation? A systematic review and meta-analysis. Arthroscopy 34(3082–3093):e3081
Manjunath AK, Hurley ET, Jazrawi LM, Strauss EJ (2020) Return to play after medial patellofemoral ligament reconstruction: a systematic review. Am J Sports Med. https://doi.org/10.1177/0363546520947044363546520947044
MarcheggianiMuccioli GM, Lullini G, Grassi A, Macchiarola L, Cammisa E, Maccaferri B et al (2020) Good results are reported at 60-month follow-up after medial patello-femoral ligament reconstruction with fascia lata allograft for recurrent patellar dislocation. Knee Surg Sports TraumatolArthrosc. https://doi.org/10.1007/s00167-020-06142-x
McPherson AL, Feller JA, Hewett TE, Webster KE (2019) Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med 47:857–862
Migliorini F, Rath B, Tingart M, Meisen N, Eschweiler J (2019) Surgical management for recurrent patellar dislocations in skeletally immature patients. Eur J OrthopSurgTraumatol 29:1815–1822
O’Connor RF, King E, Richter C, Webster KE, Falvey EC (2020) No relationship between strength and power scores and anterior cruciate ligament return to sport after injury scale 9 months after anterior cruciate ligament reconstruction. Am J Sports Med 48:78–84
Saccomanno MF, Sircana G, Fodale M, Donati F, Milano G (2016) Surgical versus conservative treatment of primary patellar dislocation. A systematic review and meta-analysis. IntOrthop 40:2277–2287
Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ (2018) Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health 10:146–151
Sappey-Marinier E, Sonnery-Cottet B, O’Loughlin P, Ouanezar H, Reina Fernandes L, Kouevidjin B et al (2019) Clinical outcomes and predictive factors for failure with isolated MPFL reconstruction for recurrent patellar instability: a series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med 47:1323–1330
Schneider DK, Grawe B, Magnussen RA, Ceasar A, Parikh SN, Wall EJ et al (2016) Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med 44:2993–3005
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35:801–804
Shultz CL, Schrader SN, Packard BD, Wascher DC, Treme GP, Richter DL (2020) Is Diagnostic arthroscopy at the time of medial patellofemoral ligament reconstruction necessary? Orthop J Sports Med 8:2325967120945654
Sidharthan S, Wang G, Schlichte LM, Fulkerson JP, Green DW (2020) Medial patellofemoral ligament reconstruction in skeletally immature patients. JBJS EssentSurg Tech 10:e0110
Sigonney F, Lopes R, Bouche PA, Kierszbaum E, Moslemi A, Anract P et al (2020) The ankle ligament reconstruction-return to sport after injury (ALR-RSI) is a valid and reproducible scale to quantify psychological readiness before returning to sport after ankle ligament reconstruction. Knee Surg Sports TraumatolArthrosc. https://doi.org/10.1007/s00167-020-06020-6
Smith MK, Werner BC, Diduch DR (2018) Avoiding complications with MPFL reconstruction. Curr Rev Musculoskelet Med 11:241–252
Straume-Naesheim TM, Randsborg PH, Mikaelsen JR, Sivertsen EA, Devitt B, Granan LP et al (2019) Recurrent lateral patella dislocation affects knee function as much as ACL deficiency—however patients wait five times longer for treatment. BMC MusculoskeletDisord 20:318
Uimonen MM, Repo JP, Huttunen TT, Nurmi H, Mattila VM, Paloneva J (2020) Surgery for patellar dislocation has evolved towards anatomical reconstructions with assessment and treatment of anatomical risk factors. Knee Surg Sports TraumatolArthrosc. https://doi.org/10.1007/s00167-020-06277-x
Webster KE, Feller JA, Lambros C (2008) Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. PhysTher Sport 9:9–15
Zaman S, White A, Shi WJ, Freedman KB, Dodson CC (2018) Return-to-play guidelines after medial patellofemoral ligament surgery for recurrent patellar instability: a systematic review. Am J Sports Med 46:2530–2539
Funding
No funding was received to conduct this study.
Author information
Authors and Affiliations
Contributions
EH conceived the design of the study and carried out data analysis and writing of the manuscript. DM carried out data acquisition, data analysis, and editing of the manuscript. BM carried out writing and editing of the manuscript. GG participated in writing and editing of the manuscript. MA participated in writing and editing of the manuscript. KC participated in writing and editing of the manuscript. LJ participated in writing and editing of the manuscript. ES participated in writing and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
Ethical approval was received by NYU Langone Institutional Review Board (#20-00972).
Informed consent
A waiver of documentation of Informed Consent was granted in accordance with 45 CFR 46.117 (c) (2).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hurley, E.T., Markus, D.H., Mannino, B.J. et al. Patients unable to return to play following medial patellofemoral ligament reconstructions demonstrate poor psychological readiness. Knee Surg Sports Traumatol Arthrosc 29, 3834–3838 (2021). https://doi.org/10.1007/s00167-021-06440-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06440-y