Abstract
Purpose
To compare outcome of operative and non-operative treatment of avulsion fractures of the hamstring origin, with minor (< 1.5 cm) and major (≥ 1.5 cm) displacement, and early (≤ 4 weeks) and delayed (> 4 weeks) surgery.
Methods
A systematic literature search was performed using PubMed, Cochrane, Embase, CINAHL and SPORTDiscus. A quality assessment was performed using the Physiotherapy Evidence Database (PEDro) scale.
Results
Eight studies with 90 patients (mean age: 16 years) were included. All studies had low methodological quality (PEDro score ≤ 5). Operative treatment yielded a return to preinjury activity rate (RTPA) of 87% (95% CI: 68–95), return to sports (RTS) rate of 100% (95% CI: 82–100), Harris hip score (HHS) of 99 (range 96–100) and a University of California Los Angeles activity scale (UCLA) score of 100%. Non-operative treatment yielded a RTPA rate of 100% (95% CI:68–100), RTS rate of 86% (95% CI: 69–94), HHS score of 99 (range 96–100), and non-union rate of 18% (95% CI: 9–34). All patients with minor displacement were treated non-operatively (RTPA: 100% [95% CI: 21–100], RTS: 100% [95% CI: 51–100]). For major displacement, operative treatment led to RTPA and RTS rates of 86% (95% CI: 65–95) and 100% (95% CI: 84–100), and 0% (0/1, 95% CI: 0–79) and 100% (95% CI: 51–100) for non-operative treatment. Early surgery yielded RTPA and RTS rates of 100% (95% CI: 34–100 & 57–100) compared to 100 (95% CI: 72–100) and 90% (95% CI: 60–98) for delayed repair.
Conclusion
All included studies have high risk of bias. There is only low level of evidence with a limited number of included patients to compare outcome of operative and non-operative treatment. Overall outcome was satisfactory. There is a treatment selection phenomenon based on displacement, with acceptable outcome in both groups. There is insufficient data to draw conclusions regarding timing of surgery.
Level of evidence
IV
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An avulsion fracture involves the forceful detachment of a bony fragment at the insertion of a tendon or ligament [10, 16]. At the proximal hamstring attachment, this type of injury generally involves the ischial apophysis. The apophysis is a secondary ossification center and represents the weakest element of the muscle–tendon-bone attachment in skeletally immature patients [4] due to incomplete closure. While full closure does not occur until late adolescence [7, 10, 11, 18] avulsion fractures of the pelvis most frequently occur among younger athletes; 95% of these injuries occur between 13 and 17 years of age [1, 4, 8, 18].
Two recent systematic reviews [3, 4] on treatment outcome of pelvic avulsion fractures showed an overall higher ‘excellent outcome’ rate and return to sports (RTS) rate compared to non-operative treatment. Both reviews concluded that, especially in patients with high functional demand and with a fragment displacement greater than 1.5 cm, operative repair should be considered [3, 4].
The main limitation of these two recent reviews is that they did not distinguish between different avulsion fracture sites and thus did not report separate data for avulsion fractures of the hamstring origin.
The main aim of this review was to evaluate clinical and radiological outcome of operative and non-operative treatment for proximal avulsion fractures of the hamstring origin. Secondary aims were to assess outcome for minor (< 1.5 cm) and major (≥ 1.5 cm) fragment displacement, as well as early (≤ 4 weeks) and delayed (> 4 weeks) surgery. Our hypothesis was that operative treatment yields superior clinical outcome, especially in avulsion fractures with displacement ≥1.5 cm. We expected early surgery to yield better clinical outcome than delayed surgery.
Materials and methods
Search strategy
A literature search using PubMed, Cochrane, Embase, CINAHL and SPORTDiscus was performed to identify potentially eligible articles up to 12 December 2019. There was no restriction on publication date. The search strategy per database can be found in the supplementary appendix.
Study selection
Selection of potentially eligible studies was performed using web app Rayyan [12] (QCRI, Doha, Qatar). Duplicates were removed. Using the eligibility criteria in Fact box 1, two reviewers (HJAN & ADM) independently assessed article eligibility based on title and abstract, followed by assessment of full-texts. If there was any doubt regarding eligibility based on screening of title and abstract, the study was moved forward to full-text screening. If no consensus was reached after assessing the full-text, a third reviewer was available. Citation tracking of included full-texts was performed after screening of full-texts. For any full-text that was not available, authors were contacted by email.

Data extraction and synthesis
Relevant data was extracted independently by two authors (HJAN & ADM) using a standardised data extraction form. This form included study design, study population, duration of follow-up, avulsion fragment displacement, treatment modality, complications, and outcome measures. In case of uncertainties, a third author was consulted. Outcome measures that were used in multiple included studies were pooled.
Risk of bias assessment
To assess the risk of bias of the included studies, The PEDro Scale [17] was used by us. Assessment was done independently by two reviewers (HJAN & ADM). In case consensus was not reached, assessment by a third reviewer was decisive. The PEDro scale uses eleven items (Fact box 2) to score the methodological quality of the included studies. Each appraisal item could be scored with ‘no’ or ‘yes’. The first item of the scale relates to external validity and is not included in the final score. This means that the final score (0–10) is calculated using items 2–11. A PEDro score of ≥ 6 indicates a low risk of bias (i.e., high-quality) study. A score of ≤ 5 indicates a high risk of bias study (i.e., low-quality study).

Evidence synthesis
Data from studies with low risk of bias will be pooled if available from multiple studies. If no studies with low risk of bias are available, data from studies with high risk of bias will be pooled. If data cannot be pooled, a best evidence synthesis will be done.
For pooled outcomes given as a proportion, 95% confidence intervals (95% CI, binomial proportion) using a Wilson score interval were calculated by us. If 95% confidence intervals overlapped indicating absence of statistically significant differences, no further statistical testing of between-group differences was performed.
Results
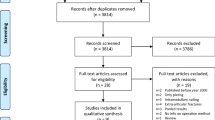
The literature search identified 586 potentially eligible study. After study selection, 8 studies were included [2, 5, 6, 9, 10, 13,14,15] (Fig. 1).
Study characteristics
The eight included studies were all case series (Table 1), with a total of 90 patients and a weighted mean age of 16 years (range in study means 14–19). Gender was reported for 79 patients (13 females and 66 males). Operative treatment was chosen in 27 patients and 63 patients were treated non-operatively.
Risk of bias assessment
The outcome of the risk of bias assessment is shown in Table 2. All assessed articles scored ≤ 5 and were considered to have high risk of bias, mainly due to the absence of blinding, randomization and control groups.
Outcome measures
Outcome measures used in the included studies were return to sports rate (RTS), return to preinjury activity rate (RTPA), outcome grading based on a 4-point outcome grading system shown in Table 3 (poor, moderate, good, excellent) [2, 5, 6, 9, 10, 13,14,15], Harris hip score (HHS) [5], rate of non-union [5, 13], Tegner Activity Scale (TAS), and University of California Los Angeles (UCLA) activity scale [2].
Outcome following operative and non-operative treatment
Operative treatment was chosen in 27 patients (6 studies) and non-operative treatment in 63 patients (5 studies). Outcome per group is presented in Table 4. Fourteen patients that were initially treated non-operatively proceeded to undergo secondary operative treatment. Excluding these cases, operative repair led to good-to-excellent outcome in 85%, compared to 83% after non-operative treatment. An RTPA rate of 87% (20/23) and RTS rate of 100% (18/18) in the operative group, compared to 100% (8/8) and 86% (24/28) in the non-operative group, was calculated. Non-unions were only reported in the non-operative group, and occurred in 18% (6/33). There was no difference between the groups in terms of mean HHS (both 99, range 96–100). The UCLA score was 100%, but was only reported in three patients in the operative group.
Outcome of secondary operative treatment
For 8 patients that underwent secondary operative treatment outcome was reported separately, and a RTS rate of 88% was calculated. Reported causes of unsatisfying results in these patients were non-union, hamstring syndrome, pseudotumor, calcified fragments and sciatic nerve entrapment.
Outcome of treatment and fragment displacement
Six studies (N = 37) reported extent of fragment displacement. Patients were divided in two groups: < 1.5 cm (N = 5) and ≥ 1.5 cm (N = 32) displacement (Table 5). All 5 patients with < 1.5 cm displacement were treated non-operatively, with a RTPA rate of 100% (1/1) and RTS rate of 100% (4/4). Thirty-two patients had a displacement of ≥ 1.5 cm from which 27 (84%) were treated operatively and 5 (16%) were treated non-operatively. The operated treatment group had RTPA and RTS rates of 86% (18/21) and 100% (20/20). In the non-operative treatment group, the RTPA and RTS rates were 0% (0/1) and 100% (4/4).
Outcome of treatment and timing of surgery
In five studies (N = 24), both timing of surgery and treatment outcome were reported (Table 6) [2, 5, 6, 9, 14]. Six patients underwent early surgery (≤ 4 weeks post injury), and all (100%) returned to pre-injury activity level (2/2) and returned to sports (5/5).
Eighteen patients underwent delayed surgery (> 4 weeks post injury), with RTPA and RTS rates of 100% (10/10) and 90% (9/10).
Discussion
The most important finding of the present study was that only studies with high risk of bias (PEDro score ≤ 5) and a limited number of included patients were available to compare treatment outcome of operative and non-operative treatment for avulsion fractures of the hamstring origin. The clinical outcome in both groups was satisfactory with high RTPA and RTS rates. The comparison is further limited by the fact that avulsion fractures with minor (< 1.5 cm) fragment displacement were all treated non-operatively indicating a selection phenomenon. Given the low level of evidence, it remains unclear which intervention is preferred. This review serves to provide an overview of currently available literature for clinicians and has identified the gaps in current evidence for future research efforts.
Overall, both operative and non-operative treatment resulted in satisfactory outcome. The group with minor avulsion fragment displacement (< 1.5 cm) had good outcome with non-operative treatment, but no data is available to compare it to outcome of operative treatment in this group. In the group with major (≥ 1.5 cm) fragment displacement, outcome in terms of RTS and RTPA are generally acceptable. For timing of operative repair, early repair (≤ 4 weeks) resulted in RTS and RTPA rates similar to the delayed repair (> 4 weeks) group, but data is scarce.
There are no other systematic reviews that have investigated outcome of avulsion fractures of the hamstring origin in isolation. Eberbach et al. [4] pooled all pelvic avulsion fractures and reported overall success rates of 88 and 79% for operative and non-operative treatment, respectively (n.s.). In addition, RTS rates of 92 and 80% were reported (p = 0.03). The review of Calderazzi et al. [3] reported similar findings. Operative treatment resulted in a RTS rate of 95% compared to 90% for non-operative treatment. The authors advocated operative treatment for avulsion fractures with greater fragments and major displacement.
These results appear to be in line with our findings in avulsion fractures of the hamstring origin. For the relationship between extent of avulsion fragment displacement and treatment outcome, the same cut-off of 1.5 cm as Eberbach et al. [4] was used. Their review concluded that avulsion fractures with less than 1.5 cm displacement could be treated non-operatively. Operative treatment was recommended for avulsion fractures with more than 1.5 cm displacement. In the current systematic review, avulsion fractures with minor displacement were treated non-operatively with satisfactory outcome. The comparison with operative repair in this group could not be made due to absence of reported data. Operative and non-operative treatment of avulsion fractures with more than 1.5 cm displacement appear to result in similar outcome but it should be noted that the sample size in the non-operative group is very small. Both early and delayed surgery yielded high RTS and RTPA rates.
All included studies in this review were scored as low-quality. There was no randomization, blinding or comparison used which causes a high risk of (e.g., selection) bias. A selection phenomenon, where treatment choice was seemingly based on the extent of avulsion fragment displacement which impeded a proper comparison, was noted. Another issue introducing bias is the lack of data on the initial and apparent non-satisfactory outcome of non-operative treatment in patients that underwent secondary operative treatment. In addition, the (sub)group sizes were too small to draw firm conclusions regarding the < 1.5 cm group and timing of surgery. There was notable variation in treatment protocols used in the various studies. This is, however, the first systematic review investigating outcome of operative and non-operative treatment for proximal hamstring avulsion fractures separately.
Implications for clinical practice and future research
In current practice, where avulsion fractures with minor (< 1.5 cm) displacement are treated non-operatively and majorly displaced (≥ 1.5 cm) avulsion fractures are predominantly treated with operative repair, overall outcome is satisfactory. Due to paucity of data and high risk of bias it remains unclear which treatment should be advised in the individual patient. On the one hand, these findings can be viewed as a confirmation of currently employed treatment decision-making based on the amount of displacement. Still, the need for comparative prospective studies and ideally randomized controlled trials is underlined to allow for a proper comparison and, by extension, development of evidence-based treatment protocols. In the meanwhile, our findings can be used to inform patients about expected outcome and guide shared-decision making.
Conclusion
All included studies have high risk of bias. Thus, there is only low level of evidence with a limited number of included patients to compare outcome of operative and non-operative outcome for proximal avulsion fractures of the hamstring origin. Overall, satisfactory outcome was found in both groups with high RTPA and RTS rates. A selection phenomenon in which treatment is chosen based on the amount of avulsion fragment displacement, resulting in acceptable outcome in both groups, was noted. There was insufficient data to conclude whether a difference exists between early and delayed surgery.
References
Anderson SJ (2002) Lower extremity injuries in youth sports. Pediatr Clin North Am 49:627–641
Biedert RM (2015) Surgical management of traumatic avulsion of the ischial tuberosity in young athletes. Clin Sports Med 25:67–72
Calderazzi F, Nosenzo A, Galavotti C, Pogliacomi F, Ceccarelli F (2018) Apophyseal avulsion fractures of the pelvis. A review. Acta Biomed Ateneo Parmense 89:470–476
Eberbach H, Hohloch L, Feucht MJ, Konstantinidis L, Südkamp NP, Zwingmann J (2017) Operative versus conservative treatment of apophyseal avulsion fractures of the pelvis in the adolescents: a systematical review with meta-analysis of clinical outcome and return to sports. BMC Musculoskelet Disord 18:162
Ferlic PW, Sadoghi P, Singer G, Kraus T, Eberl R (2014) Treatment for ischial tuberosity avulsion fractures in adolescent athletes. Knee Surg Sports Traumatol Arthrosc 22:893–897
Gidwani S, Bircher MD (2007) Avulsion injuries of the hamstring origin - a series of 12 patients and management algorithm. Ann R Coll Surg Engl 89:394–399
Howard FM, Piha RJ (1965) Fractures of the apophyses in adolescent athletes. JAMA 192:842–844
Kocher MS, Tucker R (2006) Pediatric athlete hip disorders. Clin Sports Med 25:241–253
Kujala UM, Orava S, Karpakka J, Leppavuori J, Mattila K (1997) Ischial tuberosity apophysitis and avulsion among athletes. Int J Sports Med 18:149–155
Metzmaker JN, Pappas AM (1985) Avulsion fractures of the pelvis. Am J Sports Med 13:349–358
Moeller JL (2003) Pelvic and hip apophyseal avulsion injuries in young athletes. Curr Sports Med Rep 2:110–115
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5(5):210
Schuett DJ, Bomar JD, Pennock AT (2015) Pelvic apophyseal avulsion fractures: a retrospective review of 228 cases. J Pediatr Orthop B 35:617–623
Shyamalan G, Bircher M (2010) Chronic complete proximal hamstring injury: The double-window approach for bony avulsions. Injury 41:823–826
Sinikumpu JJ, Hetsroni I, Schilders E, Lempainen L, Serlo W, Orava S (2018) Operative treatment of pelvic apophyseal avulsions in adolescent and young adult athletes: a follow-up study. Eur J Orthop Surg Traumatol 28:423–429
Tehranzadeh J (1987) The spectrum of avulsion and avulsion-like injuries of the musculoskeletal system. RadioGraphics 7:945–974
Verhagen AP, de Vet HCW, de Bie RA, Kessels AGH, Boers M, Bouter LM, Knipschild PG (1998) The delphi list. J Clin Epidemiol 51:1235–1241
Waite BL, Krabak BJ (2008) Examination and treatment of pediatric injuries of the hip and pelvis. Phys Med Rehabil Clin N Am 19:305–318
Acknowledgements
The authors would like to thank Ms. Faridi van Etten-Jamaludin for her help with the literature search.
Funding
No external funding.
Author information
Authors and Affiliations
Contributions
HN/AM: Conception, literature search, study selection, data extraction, drafting of manuscript. JT/GR/GK: Conception, interpretation, reviewing and editing of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nauta, H.J.A., van der Made, A.D., Tol, J.L. et al. Satisfactory clinical outcome of operative and non-operative treatment of avulsion fracture of the hamstring origin with treatment selection based on extent of displacement: a systematic review. Knee Surg Sports Traumatol Arthrosc 29, 1813–1821 (2021). https://doi.org/10.1007/s00167-020-06222-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06222-y