Abstract
Purpose
The aim of this study is to systematically review the current, relevant literature and provide a thorough understanding of the various open surgical approaches utilized to gain access to the talar dome for treatment of osteochondral lesions. Realizing the limits of access from soft tissue exposures and osteotomies, with and without external distraction, will help surgeons to select the appropriate approach for each individual clinical situation.
Methods
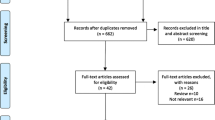
A literature search was performed using three major medical databases: PubMed (MEDLINE), Scopus, and Embase. The Quality Appraisal for Cadaveric Studies (QUACS) scale was used to assess the methodological quality of each included study.
Results
Of 3108 reviewed articles, nine cadaveric studies (113 limbs from 83 cadavers) evaluating the accessibility of the talar dome were included in the final analysis. Most of these (7/9 studies) investigated talar dome access in the context of treating osteochondral lesions of the talus (OLTs) requiring perpendicular visualization of the involved region. Five surgical approaches (anteromedial; AM, anterolateral; AL, posteromedial; PM, posterolateral; PL, and direct posterior via an Achilles tendon splitting; DP), four types of osteotomy (anterolateral tibial, medial malleolar, distal fibular, and plafondplasty), and two methods of distraction (Hintermann retractor and external fixator) were used among the included studies. The most commonly used methods quantified talar access in the sagittal plane (6/9 studies, 66.7%). The greatest exposure of the talar dome can be achieved perpendicularly by performing an additional malleolar osteotomy (90.9% for lateral, and 100% for medial). The methodological quality of all included studies was determined to be satisfactory.
Conclusion
Gaining perpendicular access to the central portion of the talar dome, measured in the sagittal plane, has clear limitations via soft tissue approaches either medially or laterally from the anterior or posterior aspects of the ankle. It is possible to access a greater talar dome area in a non-perpendicular fashion, especially from the posterior soft tissue approach. Various types of osteotomies can provide greater accessibility to the talar dome. This systematic review can help surgeons to select the appropriate approach for treatment of OLTs in each individual patient preoperatively.
Level of evidence
Level IV.




Similar content being viewed by others
References
Alexander AH, Lichtman DM (1980) Surgical treatment of transchondral talar-dome fractures (osteochondritis dissecans). Long-term follow-up. J Bone Joint Surg Am 62:646–652
Alexander IJ, Watson JT (1991) Step-cut osteotomy of the medial malleolus for exposure of the medial ankle joint space. Foot Ankle 11:242–243
Angthong C, Yoshimura I, Kanazawa K, Takeyama A, Hagio T, Ida T et al (2013) Critical three-dimensional factors affecting outcome in osteochondral lesion of the talus. Knee Surg Sports Traumatol Arthrosc 21:1418–1426
Barg A, Pagenstert G, Leumann A, Valderrabano V (2013) Malleolar osteotomy–osteotomy as approach. Orthopade 42:309–321
Berndt AL, Harty M (1959) Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am 41-A:988–1020
Canale ST, Belding RH (1980) Osteochondral lesions of the talus. J Bone Joint Surg Am 62:97–102
Dekker TJ, Dekker PK, Tainter DM, Easley ME, Adams SB (2017) Treatment of osteochondral lesions of the talus: a critical analysis review. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.16.00065
Early JS (2004) Management of fractures of the talus: body and head regions. Foot Ankle Clin 9:709–722
Easley ME, Latt LD, Santangelo JR, Merian-Genast M, Nunley JA 2nd (2010) Osteochondral lesions of the talus. J Am Acad Orthop Surg 18:616–630
Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM (2007) Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int 28:154–161
Filardo G, Andriolo L, Soler F, Berruto M, Ferrua P, Verdonk P et al (2019) Treatment of unstable knee osteochondritis dissecans in the young adult: results and limitations of surgical strategies-the advantages of allografts to address an osteochondral challenge. Knee Surg Sports Traumatol Arthrosc 27:1726–1738
Flick AB, Gould N (1985) Osteochondritis dissecans of the talus (transchondral fractures of the talus): review of the literature and new surgical approach for medial dome lesions. Foot Ankle 5:165–185
Galla M, Duensing I, Kahn TL, Barg A (2019) Open reconstruction with autologous spongiosa grafts and matrix-induced chondrogenesis for osteochondral lesions of the talus can be performed without medial malleolar osteotomy. Knee Surg Sports Traumatol Arthrosc 27:2789–2795
Garras DN, Santangelo JA, Wang DW, Easley ME (2008) A quantitative comparison of surgical approaches for posterolateral osteochondral lesions of the talus. Foot Ankle Int 29:415–420
Georgiannos D, Bisbinas I, Badekas A (2016) Osteochondral transplantation of autologous graft for the treatment of osteochondral lesions of talus: 5- to 7-year follow-up. Knee Surg Sports Traumatol Arthrosc 24:3722–3729
Haidich AB (2010) Meta-analysis in medical research. Hippokratia 14:29–37
Hammit MD, Hobgood ER, Tarquinio TA (2006) Midline posterior approach to the ankle and hindfoot. Foot Ankle Int 27:711–715
Hangody L, Feczko P, Bartha L, Bodo G, Kish G (2001) Mosaicplasty for the treatment of articular defects of the knee and ankle. Clin Orthop Relat Res 391(Suppl):S328–S336
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85-A(Suppl 2):25–32
Kerkhoffs G, Karlsson J (2019) Osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 27:2719–2720
Leumann A, Horisberger M, Buettner O, Mueller-Gerbl M, Valderrabano V (2016) Medial malleolar osteotomy for the treatment of talar osteochondral lesions: anatomical and morbidity considerations. Knee Surg Sports Traumatol Arthrosc 24:2133–2139
Malagelada F, Dalmau-Pastor M, Vega J, Dega R, Clark C (2019) Access to the talar dome surface with different surgical approaches. Foot Ankle Surg 25:618–622
Mayne AIW, Lawton R, Reidy MJ, Harrold F, Chami G (2018) A comparison of surgical exposures for posterolateral osteochondral lesions of the talar dome. Foot Ankle Surg 24:107–109
McInnes MDF, Moher D, Thombs BD, McGrath TA, Bossuyt PM, the P-DTAG et al (2018) Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319:388–396
Melenevsky Y, Mackey RA, Abrahams RB, Thomson NB 3rd (2015) Talar fractures and dislocations: a radiologist’s guide to timely diagnosis and classification. Radiographics 35:765–779
Muir D, Saltzman CL, Tochigi Y, Amendola N (2006) Talar dome access for osteochondral lesions. Am J Sports Med 34:1457–1463
Murphy EP, Fenelon C, Egan C, Kearns SR (2019) Matrix-associated stem cell transplantation is successful in treating talar osteochondral lesions. Knee Surg Sports Traumatol Arthrosc 27:2737–2743
Patzkowski JC, Kirk KL, Orr JD, Waterman BR, Kirby JM, Hsu JR (2012) Quantification of posterior ankle exposure through an achilles tendon-splitting versus posterolateral approach. Foot Ankle Int 33:900–904
Peters PG, Parks BG, Schon LC (2012) Anterior distal tibia plafondplasty for exposure of the talar dome. Foot Ankle Int 33:231–235
Rammelt S, Zwipp H (2009) Talar neck and body fractures. Injury 40:120–135
Ramponi L, Yasui Y, Murawski CD, Ferkel RD, DiGiovanni CW, Kerkhoffs G et al (2017) Lesion size is a predictor of clinical outcomes after bone marrow stimulation for osteochondral lesions of the talus: a systematic review. Am J Sports Med 45:1698–1705
Rausch S, Loracher C, Frober R, Gueorguiev B, Wagner A, Gras F et al (2014) Anatomical evaluation of different approaches for tibiotalocalcaneal arthrodesis. Foot Ankle Int 35:163–167
Rush JK, Kirk K, Kirby J, Hsu J (2010) Lateral talar dome access utilizing temporary invasive distraction. Foot Ankle Int 31:236–241
Sandlin MI, Charlton TP, Taghavi CE, Giza E (2017) Management of osteochondral lesions of the talus. Instr Course Lect 66:293–299
Shakked RJ, Tejwani NC (2013) Surgical treatment of talus fractures. Orthop Clin North Am 44:521–528
Shank JR, Benirschke SK, Swords MP (2017) Treatment of peripheral talus fractures. Foot Ankle Clin 22:181–192
Tochigi Y, Amendola A, Muir D, Saltzman C (2002) Surgical approach for centrolateral talar osteochondral lesions with an anterolateral osteotomy. Foot Ankle Int 23:1038–1039
Vallier HA (2015) Fractures of the talus: state of the Art. J Orthop Trauma 29:385–392
Wilke J, Krause F, Niederer D, Engeroff T, Nurnberger F, Vogt L et al (2015) Appraising the methodological quality of cadaveric studies: validation of the QUACS scale. J Anat 226:440–446
Woelfle JV, Reichel H, Nelitz M (2013) Indications and limitations of osteochondral autologous transplantation in osteochondritis dissecans of the talus. Knee Surg Sports Traumatol Arthrosc 21:1925–1930
Young KW, Deland JT, Lee KT, Lee YK (2010) Medial approaches to osteochondral lesion of the talus without medial malleolar osteotomy. Knee Surg Sports Traumatol Arthrosc 18:634–637
Acknowledgements
The authors wish to thank Dillon O’Neil, MD for his assistance in preparing this manuscript.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
An ethical approval was not required for this systematic literature review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sripanich, Y., Dekeyser, G., Steadman, J. et al. Limitations of accessibility of the talar dome with different open surgical approaches. Knee Surg Sports Traumatol Arthrosc 29, 1304–1317 (2021). https://doi.org/10.1007/s00167-020-06113-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06113-2