Abstract
Purpose
Periprosthetic infection is a common reason for surgical revision. Given the increasing resistance of bacteria to antibiotics (e.g., VRE, 4-MRGN) local antiseptic treatment is gaining in importance. However, no standard guideline-based treatment recommendation is yet available. The aim of this study was to investigate the effectiveness of sodium hypochlorite and chlorhexidine against bacterial biofilms. Furthermore, the toxicity of both antiseptics towards human chondrocytes was examined.
Methods
Human chondrocytes were isolated, cultivated and treated with sodium hypochlorite and chlorhexidine. The viability of cultures was assessed by determination of cell count, XTT and MTT ELISAs, and fluorescent staining with propidium iodide. Bacterial strains of Staphylococcus aureus, Staphylococcus epidermidis and Pseudomonas aeruginosa were added to liquid media and incubated overnight. After determination of bacterial concentrations polyethylene (PE) devices were inoculated with bacteria for 48 h until biofilms formed. The devices were then washed, treated with antiseptics for 2 and 5 min and subsequently spread on agar plates.
Results
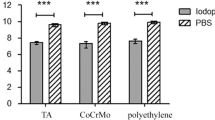
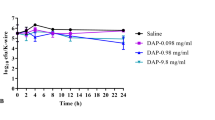
Sodium hypochlorite is more effective than chlorhexidine in penetrating biofilms of S. aureus, S. epidermidis and P. aeruginosa. Both antiseptics are chondrotoxic, but sodium hypochlorite damages human chondrocytes less than chlorhexidine in vitro.
Conclusions
The findings confirm the effectiveness of sodium hypochlorite and chlorhexidine against bacterial biofilms. Both antiseptics can be recommended for the treatment of periprosthetic infections. The toxic effects of sodium hypochlorite and chlorhexidine towards chondrocytes may mean there is a risk of damage to cartilage tissue.
Level of evidence
Controlled experimental study.









Similar content being viewed by others
References
Ince A, Schütze N, Hendrich C et al (2007) Effect of polyhexanide and gentamycin on human osteoblasts and endothelial cells. Swiss Med Wkly 137:139–145
Kramer A (2016) Wundantiseptik. Available via DIALOG. https://www.rosenfluh.ch/arsmedici-2016-09/wundantiseptik
Lineback CB, Nkemngong CA, Wu ST, Li X, Teska PJ, Oliver HF (2018) Hydrogen peroxide and sodium hypochlorite disinfectants are more effective against Staphylococcus aureus and Pseudomonas aeruginosa biofilms than quaternary ammonium compounds. Antimicrob Resist Infect Control 7:154
Röhner E, Kolar P, Seeger JB, Arnholdt J, Thiele K, Perka C, Matziolis G (2011) Toxicity of antiseptics against chondrocytes: what is best for the cartilage in septic joint surgery? Int Orthop 35:1719–1723
Röhner E, Hoff P, Gaber T, Lang A, Vörös P, Buttgereit F, Perka C, Windisch C, Matziolis G (2015) Cytokine expression in human osteoblasts after antiseptic treatment: a comparative study between polyhexanide and chlorhexidine. J Invest Surg 28:1–7
Schaumburger J, Beckmann J, Springorum HR et al (2010) Toxicity of antiseptics on chondrocytes in vitro. Z für Orthop Unfallchirurgie 148:39–43
Serag W (2018) LAVANOX® available via DIALOG. https://www.serag-wiessner.de/fileadmin/redakteur/PDF/loesungen/851194-2019_04-de-Lavanox.pdf
Severing AL, Rembe JD, Koester V, Stuermer EK (2019) [Safety and efficacy profiles of different commercial sodium hypochlorite/hypochlorous acid solutions (NaClO/HClO): antimicrobial efficacy, cytotoxic impact and physicochemical parameters in vitro. J Antimicrob Chemother 74:365–372
Tigani D, Trisolino G, Fosco M, Ben Ayad R, Costigliola P (2013) Two-stage reimplantation for periprosthetic knee infection: influence of host health status and infecting microorganism. Knee 20:9–18
van Meurs SJ, Gawlitta D, Heemstra KA, Poolman RW, Vogely HC, Kruyt MC (2014) Selection of an optimal antiseptic solution for intraoperative irrigation: an in vitro study. J Bone Joint Surg Am 96:285–291
Vörös P, Dobrindt O, Perka C, Windisch C, Matziolis G, Röhner E (2014) Human osteoblast damage after antiseptic treatment. Int Orthop 38:177–182
Willy C, Scheuermann-Poley C, Stichling M, von Stein T, Kramer A (2017) Importance of wound irrigation solutions and fluids with antiseptic effects in therapy and prophylaxis: update 2017. Unfallchirurg 120:549–560
Funding
This study was supported by the non-profit research fund of Stiftung Endoprothetik (Grant S 01/17) (Hamburg, Germany).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Medical Ethics Committee of our Center and conducted in accordance with the ethical Standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Röhner, E., Jacob, B., Böhle, S. et al. Sodium hypochlorite is more effective than chlorhexidine for eradication of bacterial biofilm of staphylococci and Pseudomonas aeruginosa. Knee Surg Sports Traumatol Arthrosc 28, 3912–3918 (2020). https://doi.org/10.1007/s00167-020-05887-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05887-9