Abstract
Purpose
Given the increasing incidence of arthroscopic anterior cruciate ligament reconstruction (ACLR), mid- to long-term rates of reoperations were investigated on the ipsilateral knee following ACLR.
Methods
New York Statewide Planning and Research Cooperative Systems (SPARCS) database was queried from 2003 to 2012 to identify patients with a primary ICD-9 diagnosis for ACL tear and concomitant CPT code for ACLR. Patients were longitudinally followed for at least 2 years to determine incidence and nature of subsequent ipsilateral knee procedures.
Results
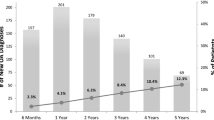
The inclusion criteria were met by 45,231 patients who had undergone ACLR between 2003 and 2012. Mean age was found to be 29.7 years (SD 11.6). Subsequent ipsilateral outpatient knee surgery after a mean of 25.7 ± 24.5 months was performed in 10.7% of patients. Revision ACLR was performed for nearly one-third of reoperations. Meniscal pathology was addressed in 58% of subsequent procedures. Age 19 or younger, female gender, worker’s compensation (WC) insurance, and Caucasian race were identified as independent risk factors for any ipsilateral reoperation. An initial isolated ACLR and initial ACLR performed by a high-volume surgeon were found to be independently associated with lower reoperation rates. Tobacco use was not significant. Survival rates of 93.4%, 89.8% and 86.7% at 2-, 5- and 10 years, respectively, were found for any ipsilateral reoperation.
Conclusion
A 10.7% ipsilateral reoperation rate at an average of 25.9 (SD 24.5) months after ACLR and an overall ACLR revision rate of 3.1% were demonstrated by the analysis. Meniscal pathology was addressed in the majority of subsequent interventions. Age 19 or younger, female gender, Caucasian race, and WC claim were associated with reoperation. Initial isolated ACLR and procedure performed by high-volume surgeon were associated with reduced reoperation.
Level of evidence
Level III.






Similar content being viewed by others
References
Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J (2012) The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med 40:2230–2235
Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K (2015) Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med 43:121–127
Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU (2015) Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers' compensation subjects. Spine 40:748–756 (Phila Pa 1976)
Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU (2015) Return to work after Diskogenic fusion in workers' compensation subjects. Orthopedics 38:e1065–1072
Bansal A, Khatib ON, Zuckerman JD (2014) Revision total joint arthroplasty: the epidemiology of 63,140 cases in New York State. J Arthroplasty 29:23–27
Barber SD, Noyes FR, Mangine R, DeMaio M (1992) Rehabilitation after ACL reconstruction: function testing. Orthopedics 15:969–974
Barenius B, Forssblad M, Engstrom B, Eriksson K (2013) Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 21:914–927
Barrett GR, Rook RT, Nash CR, Coggin MR (2001) The effect of Workers' Compensation on clinical outcomes of arthroscopic-assisted autogenous patellar tendon anterior cruciate ligament reconstruction in an acute population. Arthroscopy 17:132–137
Baverel L, Demey G, Odri GA, Leroy P, Saffarini M, Dejour D (2015) Do outcomes of outpatient ACL reconstruction vary with graft type? Orthop Traumatol Surg Res 101:803–806
Brandsson S, Faxen E, Eriksson BI, Sward L, Lundin O, Karlsson J (1999) Reconstruction of the anterior cruciate ligament: comparison of outside-in and all-inside techniques. Br J Sports Med 33:42–45
Buss DD, Warren RF, Wickiewicz TL, Galinat BJ, Panariello R (1993) Arthroscopically assisted reconstruction of the anterior cruciate ligament with use of autogenous patellar-ligament grafts. Results after twenty-four to forty-two months. J Bone Jt Surg Am 75:1346–1355
Cancienne JM, Gwathmey FW, Miller MD, Werner BC (2016) Tobacco use is associated with increased complications after anterior cruciate ligament reconstruction. Am J Sports Med 44:99–104
Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E (2013) Cumulative incidence of ACL reconstruction after ACL injury in adults: role of age, sex, and race. Am J Sports Med 41:544–549
Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL (2012) National trends in rotator cuff repair. J Bone Jt Surg Am 94:227–233
Crawford SN, Waterman BR, Lubowitz JH (2013) Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy 29:1566–1571
Csintalan RP, Inacio MC, Funahashi TT, Maletis GB (2014) Risk factors of subsequent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med 42:619–625
Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S (2014) 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med 42:675–680
Dragoo JL, Padrez K, Workman R, Lindsey DP (2009) The effect of relaxin on the female anterior cruciate ligament: Analysis of mechanical properties in an animal model. Knee 16:69–72
Ellis HB, Matheny LM, Briggs KK, Pennock AT, Steadman JR (2012) Outcomes and revision rate after bone-patellar tendon-bone allograft versus autograft anterior cruciate ligament reconstruction in patients aged 18 years or younger with closed physes. Arthroscopy 28:1819–1825
Ensor KL, Kwon YW, Dibeneditto MR, Zuckerman JD, Rokito AS (2013) The rising incidence of rotator cuff repairs. J Shoulder Elbow Surg 22:1628–1632
Eriksson K, Anderberg P, Hamberg P, Lofgren AC, Bredenberg M, Westman I et al (2001) A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Jt Surg Br 83:348–354
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Jt Surg Br 30B:664–670
Faltstrom A, Hagglund M, Magnusson H, Forssblad M, Kvist J (2016) Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish national ACL register. Knee Surg Sports Traumatol Arthrosc 24:885–894
Gaskill T, Pullen M, Bryant B, Sicignano N, Evans AM, DeMaio M (2015) The prevalence of symptomatic deep venous thrombosis and pulmonary embolism after anterior cruciate ligament reconstruction. Am J Sports Med 43:2714–2719
Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G et al (2014) Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med 42:2319–2328
Hanypsiak BT, Spindler KP, Rothrock CR, Calabrese GJ, Richmond B, Herrenbruck TM et al (2008) Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med 36:671–677
Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Consortium M, Spindler KP (2015) Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med 43:1583–1590
Kartus JT, Russell VJ, Salmon LJ, Magnusson LC, Brandsson S, Pehrsson NG et al (2002) Concomitant partial meniscectomy worsens outcome after arthroscopic anterior cruciate ligament reconstruction. Acta Orthop Scand 73:179–185
Khatib O, Onyekwelu I, Zuckerman JD (2014) The incidence of proximal humeral fractures in New York State from 1990 through 2010 with an emphasis on operative management in patients aged 65 years or older. J Shoulder Elbow Surg 23:1356–1362
Kiapour AM, Fleming BC, Proffen BL, Murray MM (2015) Sex influences the biomechanical outcomes of anterior cruciate ligament reconstruction in a preclinical large animal model. Am J Sports Med 43:1623–1631
Kim S, Bosque J, Meehan JP, Jamali A, Marder R (2011) Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Jt Surg Am 93:994–1000
Komatsuda T, Sugita T, Sano H, Kusakabe T, Watanuki M, Yoshizumi Y et al (2006) Does estrogen alter the mechanical properties of the anterior cruciate ligament? An experimental study in rabbits. Acta Orthop 77:973–980
Kowalchuk DA, Harner CD, Fu FH, Irrgang JJ (2009) Prediction of patient-reported outcome after single-bundle anterior cruciate ligament reconstruction. Arthroscopy 25:457–463
Laxdal G, Kartus J, Ejerhed L, Sernert N, Magnusson L, Faxen E et al (2005) Outcome and risk factors after anterior cruciate ligament reconstruction: a follow-up study of 948 patients. Arthroscopy 21:958–964
Lind M, Menhert F, Pedersen AB (2012) Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med 40:1551–1557
Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG (2009) Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Jt Surg Am 91:2321–2328
Maletis GB, Chen J, Inacio MC, Funahashi TT (2016) Age-related risk factors for revision anterior cruciate ligament reconstruction: a Cohort study of 21,304 patients from the Kaiser permanente anterior cruciate ligament registry. Am J Sports Med 44:331–336
Maletis GB, Inacio MC, Desmond JL, Funahashi TT (2013) Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. Bone Jt J 95(B):623–628
Maletis GB, Inacio MC, Funahashi TT (2013) Analysis of 16,192 anterior cruciate ligament reconstructions from a community-based registry. Am J Sports Med 41:2090–2098
Maletis GB, Inacio MC, Funahashi TT (2015) Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med 43:641–647
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr et al (2014) Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42:2363–2370
Memtsoudis SG (2009) Limitations associated with the analysis of data from administrative databases. Anesthesiology 111:449 (author reply 450–441)
Nwachukwu BU, McFeely ED, Nasreddine A, Udall JH, Finlayson C, Shearer DW et al (2011) Arthrofibrosis after anterior cruciate ligament reconstruction in children and adolescents. J Pediatr Orthop 31:811–817
Onyekwelu I, Khatib O, Zuckerman JD, Rokito AS, Kwon YW (2012) The rising incidence of arthroscopic superior labrum anterior and posterior (SLAP) repairs. J Shoulder Elbow Surg 21:728–731
Owens BD, Mountcastle SB, Dunn WR, DeBerardino TM, Taylor DC (2007) Incidence of anterior cruciate ligament injury among active duty U.S. military servicemen and servicewomen. Mil Med 172:90–91
Ponce BA, Cain EL Jr, Pflugner R, Fleisig GS, Young BL, Boohaker HA et al (2016) Risk factors for revision anterior cruciate ligament reconstruction. J Knee Surg 29:329–336
Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J et al (2006) Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med 34:721–732
Sanders TL, Kremers HM, Bryan AJ, Kremers WK, Stuart MJ, Krych AJ (2017) Procedural intervention for arthrofibrosis after ACL reconstruction: trends over two decades. Knee Surg Sports Traumatol Arthrosc 25:532–537
Scott DJ, Sherman S, Dhawan A, Cole BJ, Bach BR Jr, Mather RC 3rd (2015) Quantifying the economic impact of provider volume through adverse events: the case of sports medicine. Orthop J Sports Med 3:2325967115574476
Shelbourne KD, Gray T (2000) Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. five- to fifteen-year evaluations. Am J Sports Med 28:446–452
Shelbourne KD, Gray T, Haro M (2009) Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 37:246–251
Sherman SL, Lyman S, Koulouvaris P, Willis A, Marx RG (2008) Risk factors for readmission and revision surgery following rotator cuff repair. Clin Orthop Relat Res 466:608–613
Slauterbeck JR, Hardy DM (2001) Sex hormones and knee ligament injuries in female athletes. Am J Med Sci 322:196–199
Spindler KP, Wright RW (2008) Clinical practice. Anterior cruciate ligament tear. N Engl J Med 359:2135–2142
Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A (2010) Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med 38:1542–1548
Swartz SH, Cowan TM, DePue J, Goldstein MG (2002) Academic profiling of tobacco-related performance measures in primary care. Nicotine Tob Res 4(Suppl 1):S38–44
Tejwani SG, Chen J, Funahashi TT, Love R, Maletis GB (2015) Revision risk after allograft anterior cruciate ligament reconstruction: association with graft processing techniques, patient characteristics, and graft type. Am J Sports Med 43:2696–2705
Trojian TH, Collins S (2006) The anterior cruciate ligament tear rate varies by race in professional Women's basketball. Am J Sports Med 34:895–898
van Dijck RA, Saris DB, Willems JW, Fievez AW (2008) Additional surgery after anterior cruciate ligament reconstruction: can we improve technical aspects of the initial procedure? Arthroscopy 24:88–95
Viswanath P, Monaco NA, Lubahn JD (2015) Patient-related factors influencing ulnar-shortening osteotomy outcomes using the trimed dynamic compression plate. Orthopedics 38:e106–111
von Porat A, Roos EM, Roos H (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63:269–273
Wasserstein D, Khoshbin A, Dwyer T, Chahal J, Gandhi R, Mahomed N et al (2013) Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med 41:2099–2107
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
The authors did not receive any financial support for the research, authorship, or publication of this article.
Ethical approval
IRB Approval was not applicable according to New York University Langone Medical Center Office of Science and Research Institutional Review Board as the study did not contain human subjects research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Capogna, B.M., Mahure, S.A., Mollon, B. et al. Young age, female gender, Caucasian race, and workers’ compensation claim are risk factors for reoperation following arthroscopic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 28, 2213–2223 (2020). https://doi.org/10.1007/s00167-019-05798-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05798-4