Abstract
Purpose
This study aimed to identify the predictive factors for postoperative osteochondritis dissecans (OCD) in juvenile and adolescent knees with discoid lateral meniscus (DLM).
Methods
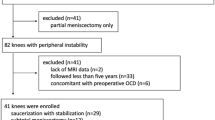
In total, 242 patients with symptomatic DLM who underwent surgery were identified. Inclusion criteria were set as follows: (1) age ≤ 17 years with an open growth plate, (2) follow-up magnetic resonance imaging, and (3) absence of preoperative OCD. Consequently, 52 patients were retrospectively investigated. Average age during surgery, body mass index (BMI), and follow-up duration were 12 years [95% confidence interval (CI) 11–13], 19.2 kg/m2 (95% CI 18.4–20.1), and 27.3 months (95% CI 20.9–33.7), respectively. Age, sex, sports activities, BMI, symptomatic OCD in other joints, postoperative rehabilitation, preoperative shift of DLM by Ahn’s classification, surgical procedures (saucerization alone or with stabilization, and subtotal meniscectomy), and postoperative meniscal width were analyzed as possible predictive factors.
Results
Postoperatively, 42 patients without OCD and 10 with OCD were observed. In univariate analysis, younger age [odds ratio (OR) 1.5; p = 0.003], subtotal meniscectomy (OR 6.3; p = 0.027), and shorter meniscal width (OR 2.7; p = 0.005) were predictive factors for postoperative OCD. Multivariate analysis demonstrated that younger age (OR 1.6; p = 0.009) and shorter meniscal width (OR 1.5; p = 0.003) were predictive factors.
Conclusions
To prevent postoperative OCD after DLM surgeries, achieving stabilization with adequate meniscal width is necessary for juvenile knees.
Level of Evidence
III.





Similar content being viewed by others
References
Abdon P, Turner MS, Pettersson H, Lindstrand A, Stenstrom A, Swanson AJ (1990) A long-term follow-up study of total meniscectomy in children. Clin Orthop Relat Res 257:166–170
Adachi N, Ochi M, Uchio Y, Kuriwaka M, Shinomiya R (2004) Torn discoid lateral meniscus treated using partial central meniscectomy and suture of the peripheral tear. Arthroscopy 20:536–542
Ahn JH, Lee SH, Yoo JC, Lee YS, Ha HC (2008) Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow-up. Arthroscopy 24:888–898
Ahn JH, Lee YS, Ha HC, Shim JS, Lim KS (2009) A novel magnetic resonance imaging classification of discoid lateral meniscus based on peripheral attachment. Am J Sports Med 37:1564–1569
Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH (2015) Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy 31:867–873
Bohndorf K (1998) Osteochondritis (osteochondrosis) dissecans: a review and new MRI classification. Eur Radiol 8:103–112
Choi SH, Ahn JH, Kim KI, Ji SK, Kang SM, Kim JS, Lee SH (2015) Do the radiographic findings of symptomatic discoid lateral meniscus in children differ from normal control subjects? Knee Surg Sports Traumatol Arthrosc 23:1128–1134
Deie M, Ochi M, Sumen Y, Kawasaki K, Adachi N, Yasunaga Y, Ishida O (2006) Relationship between osteochondritis dissecans of the lateral femoral condyle and lateral menisci types. J Pediatr Orthop 26:79–82
Edmonds EW, Shea KG (2013) Osteochondritis dissecans: editorial comment. Clin Orthop Relat Res 471:1105–1106
Fujikawa K, Iseki F, Mikura Y (1981) Partial resection of the discoid meniscus in the child’s knee. J Bone Joint Surg Br 63:391–395
Han SB, Babu CP, Choi JH, Suh DW, Jang KM (2018) Regeneration of lateral discoid meniscus after arthroscopic partial meniscectomy in an adult patient. Knee Surg Sports Traumatol Arthrosc 26:2278–2281
Haskel JD, Uppstrom TJ, Dare DM, Rodeo SA, Green DW (2018) Decline in clinical scores at long-term follow-up of arthroscopically treated discoid lateral meniscus in children. Knee Surg Sports Traumatol Arthrosc 26:2906–2911
Hefti F, Beguiristain J, Krauspe R, Möller-Madsen B, Riccio V, Tschauner C, Wetzel R, Zeller R (1999) Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B 8:231–245
Hino T, Furumatsu T, Fujii M, Kodama Y, Miyazawa S, Kamatsuki Y, Yamada K, Ozaki T (2017) Tibial eminence width can predict the presence of complete discoid lateral meniscus: a preliminary study. J Orthop Sci 22:1084–1088
Kessler JI, Nikizad H, Shea KG, Jacobs JC Jr, Bebchuk JD, Weiss JM (2014) The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am J Sports Med 42:320–326
Kim SJ, Chun YM, Jeong JH, Ryu SW, Oh KS, Lubis AM (2007) Effects of arthroscopic meniscectomy on the long-term prognosis for the discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc 15:1315–1320
Kocher MS, Tucker R, Ganley TJ, Flynn JM (2006) Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med 34:1181–1191
Manzione M, Pizzutillo PD, Peoples AB, Schweizer PA (1983) Meniscectomy in children: a long-term follow-up study. Am J Sports Med 11:111–115
Matsuo T, Kinugasa K, Sakata K, Ohori T, Mae T, Hamada M (2017) Post-operative deformation and extrusion of the discoid lateral meniscus following a partial meniscectomy with repair. Knee Surg Sports Traumatol Arthrosc 25:390–396
Mizuta H, Nakamura E, Otsuka Y, Kudo S, Takagi K (2001) Osteochondritis dissecans of the lateral femoral condyle following total resection of the discoid lateral meniscus. Arthroscopy 17:608–612
Nakayama H, Iseki T, Kambara S, Yoshiya S (2016) Analysis of risk factors for poor prognosis in conservatively managed juvenileosteochondritis dissecans of the lateral femoral condyle. Knee 23:950–954
Ogut T, Kesmezacar H, Akgun I, Cansu E (2003) Arthroscopic meniscectomy for discoid lateral meniscus in children and adolescents: 4.5 year follow-up. J Pediatr Orthop B 12:390–397
Okazaki K, Miura H, Matsuda S, Hashizume M, Iwamoto Y (2006) Arthroscopic resection of the discoid lateral meniscus: long-term followup for 16 years. Arthroscopy 22:967–971
Pellacci F, Montanari G, Prosperi P, Galli G, Celli V (1992) Lateral discoid meniscus: treatment and results. Arthroscopy 8:526–530
Rauh PB, Papoutsidakis A, Vlachonikolisi IG, Craig DM (2003) Revision arthroscopic partial meniscectomy of the knee. A retrospective review. Acta Orthop Belg 69:168–174
Rosenberg TD, Paulos LE, Parker RD, Harner CD, Gurley WD (1987) Discoid lateral meniscus: case report of arthroscopic attachment of a symptomatic Wrisberg-ligament type. Arthroscopy 3:277–282
Takigami J, Hashimoto Y, Tomihara T, Yamasaki S, Tamai K, Kondo K, Nakamura H (2018) Predictive factors for osteochondritis dissecans of the lateral femoral condyle concurrent with a discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc 26:799–805
Tsujii A, Matsuo T, Kinugasa K, Yonetani Y, Hamada M (2018) Arthroscopic minimum saucerization and inferior-leaf meniscectomy for a horizontal tear of a complete discoid lateral meniscus: report of two cases. Int J Surg Case Rep 53:372–376
Vandermeer RD, Cunningham FK (1989) Arthroscopic treatment of the discoid meniscus: results of long-term follow-up. Arthroscopy 5:101–109
Wei X, Räsänen T, Messner K (1998) Maturation-related compressive properties of rabbit knee articular cartilage and volume fraction of subchondral tissue. Osteoarthr Cartil 6:400–409
Xu Z, Chen D, Shi D, Dai J, Yao Y, Jiang Q (2016) Evaluation of posterior lateral femoral condylar hypoplasia using axial MRI images in patients with complete discoid meniscus. Knee Surg Sports Traumatol Arthrosc 24:909–914
Yamasaki S, Hashimoto Y, Takigami J, Terai S, Takahashi S, Nakamura H (2017) Risk factors associated with knee joint degeneration after arthroscopic reshaping for juvenile discoid lateral meniscus. Am J Sports Med 45:570–577
Yaniv M, Blumberg N (2007) The discoid meniscus. J Child Orthop 1:89–96
Yonetani Y, Nakamura N, Natsuume T, Shiozaki Y, Tanaka Y, Horibe S (2010) Histological evaluation of juvenile osteochondritis dissecans of the knee: a case series. Knee Surg Sports Traumatol Arthrosc 18:723–730
Acknowledgements
The authors would like to thank all doctors in Niigata University and the affiliated hospitals: Drs. Watanabe K, Yamamoto N, Omori G, Shiozaki H, Segawa H, Matsueda M, Yamagiwa H, Higano Y, Ariumi A, Mera H, Murayama T, Fujii T, Koga H, Takagi S, Katsumi R, Muraoka O, Yamanaka K, Hokari S, Tomiyama Y, Hosono Y, Otani K, Soeno T, Hijikata H, Sasage Y, Maeda K, Someya K, and Koga Y. Moreover, we would like to thank Dr. Yonetani Y in Hoshigaoka Medical Center.
Funding
No external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors did not receive and will not receive any benefits or funding from any commercial party related directly or indirectly to the subject of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mochizuki, T., Tanifuji, O., Sato, T. et al. Predictive factors for developing osteochondritis dissecans after surgery for discoid lateral meniscus are younger age and shorter meniscal width. Knee Surg Sports Traumatol Arthrosc 29, 100–108 (2021). https://doi.org/10.1007/s00167-019-05750-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05750-6