Abstract
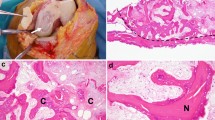
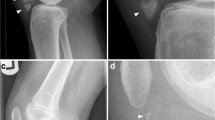
Osteochondritis dissecans (OCD) is an acquired, potentially reversible idiopathic disease of subchondral bone resulting in delamination and sequestration. Although juvenile-type OCD lesions typically appear stable on superficial examination, conservative treatment results in cure in approximate 50% of patients. We hypothesized that juvenile-type OCD lesions exhibit an underlying instability despite stability at the articular surface and this underlying instability might underlie the lack of effectiveness of conservative treatment. In this study, osteochondral cylindrical tissue samples obtained from stable juvenile OCD lesions located at the medial femoral condyle (classical site) were examined. Eight patients with symptomatic juvenile-type OCD at the classical site underwent arthroscopy. Osteochondral cylindrical tissue samples were obtained from the central portion using a biopsy needle. The samples underwent macroscopic and microscopic examination. All cylindrical samples demonstrated macroscopic separation. On microscopic examination, no degenerative changes in articular cartilage and no bone necrosis were observed. Histological examination revealed two distinct patterns in the samples: (1) thick homogeneous hyaline cartilage alone with little fibrous tissue surrounding areas of separation and (2) nearly normal, thin hyaline cartilage above a mixed layer of hyaline cartilage and subchondral trabeculae and fibrous/fibro-cartilaginous tissue at the areas of separation, indicating delayed or nonunion. Pathological findings in stable juvenile OCD lesions indicate an underlying instability at deeper layers of articular cartilage and poor healing at areas of separation. Improved knowledge of the histology of juvenile-type OCD lesions may support surgical treatment. Early marrow stimulation and/or fixation may be the treatment of choice to promote healing even in macroscopically stable juvenile-type OCD lesions.





Similar content being viewed by others
Notes
ICRS Cartilage Injury Evaluation Package AahwcofcIep.
References
Anderson AF, Lipscomb AB, Coulam C (1990) Antegrade curettement, bone grafting and pinning of osteochondritis dissecans in the skeletally mature knee. Am J Sports Med 18:254–261
Aurich M, Anders J, Trommer T et al (2006) Histological and cell biological characterization of dissected cartilage fragments in human osteochondritis dissecans of the femoral condyle. Arch Orthop Trauma Surg 126:606–614
Barrie HJ (1980) Hypertrophy and laminar calcification of cartilage in loose bodies as probable evidence of an ossification abnormality. J Pathol 132:161–168
Barrie HJ (1984) Hypothesis—a diagram of the form and origin of loose bodies in osteochondritis dissecans. J Rheumatol 11:512–513
Barrie HJ (1987) Osteochondritis dissecans 1887–1987. A centennial look at Konig’s memorable phrase. J Bone Joint Surg Br 69:693–695
Cahill B (1985) Treatment of juvenile osteochondritis dissecans and osteochondritis dissecans of the knee. Clin Sports Med 4:367–384
Cahill BR (1995) Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg 3:237–247
Cahill BR, Phillips MR, Navarro R (1989) The results of conservative management of juvenile osteochondritis dissecans using joint scintigraphy. A prospective study. Am J Sports Med 17:601–605 discussion 605-606
Chiroff RT, Cooke CP 3rd (1975) Osteochondritis dissecans: a histologic and microradiographic analysis of surgically excised lesions. J Trauma 15:689–696
Clanton TO, DeLee JC (1982) Osteochondritis dissecans. History, pathophysiology and current treatment concepts. Clin Orthop Relat Res 167:50–64
Green WT, Banks HH (1953) Osteochondritis dissecans in children. J Bone Joint Surg Am 35-A:26–47 (passim)
Hunziker EB, Kapfinger E, Geiss J (2007) The structural architecture of adult mammalian articular cartilage evolves by a synchronized process of tissue resorption and neoformation during postnatal development. Osteoarthr Cartil 15:403–413
Kocher MS, Tucker R, Ganley TJ et al (2006) Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med 34:1181–1191
Konig H, Skalej M, Hontzsch D et al (1988) NMR tomography of bone–cartilage transplants in the knee joint: transplant morphology and an attempt at the quantitative assessment of cartilage changes. Rofo 148:176–182
Linden B, Telhag H (1977) Osteochondritis dissecans. A histologic and autoradiographic study in man. Acta Orthop Scand 48:682–686
Milgram JW (1978) Radiological and pathological manifestations of osteochondritis dissecans of the distal femur. A study of 50 cases. Radiology 126:305–311
Mitsuoka T, Shino K, Hamada M et al (1999) Osteochondritis dissecans of the lateral femoral condyle of the knee joint. Arthroscopy 15:20–26
Mizuta H, Nakamura E, Otsuka Y et al (2001) Osteochondritis dissecans of the lateral femoral condyle following total resection of the discoid lateral meniscus. Arthroscopy 17:608–612
Mubarak SJ, Carroll NC (1979) Familial osteochondritis dissecans of the knee. Clin Orthop Relat Res 140:131–136
Nagura S (1960) The so-called osteochondritis dissecans of Konig. Clin Orthop Relat Res 18:100–121
Rivas R, Shapiro F (2002) Structural stages in the development of the long bones and epiphyses: a study in the New Zealand white rabbit. J Bone Joint Surg Am 84-A:85–100
Tomatsu T, Imai N, Takeuchi N et al (1992) Experimentally produced fractures of articular cartilage and bone. The effects of shear forces on the pig knee. J Bone Joint Surg Br 74:457–462
Acknowledgment
The authors are very grateful to Dr. Kiyoshi Kawano, Department of Clinical Pathology, Osaka Rosai Hospital for his histological evaluations and supports.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yonetani, Y., Nakamura, N., Natsuume, T. et al. Histological evaluation of juvenile osteochondritis dissecans of the knee: a case series. Knee Surg Sports Traumatol Arthrosc 18, 723–730 (2010). https://doi.org/10.1007/s00167-009-0898-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0898-6