Abstract
Purpose
To compare acute ACL reconstruction (ACLR) within 8 days of injury with delayed reconstruction after normalized range of motion (ROM), 6–10 weeks after injury. It was hypothesized that acute ACL reconstruction with modern techniques is safe and can be beneficial in terms of patient-reported outcomes and range of motion.
Methods
The effect of acute and delayed ACLR was randomized studied on 70 patients with high recreational activity level, Tegner level 6 or more, between 2006 and 2013. Patient-reported outcomes, objective IKDC, KOOS, and manual stability measurements were documented during the 24-month follow-up period.
Results
The acute ACLR group did not result in increased stiffness and showed superior outcome regarding strength and how the patient felt their knee functioning at 24 months. In addition, the acute group was not inferior to the delayed group in any assessment. Regarding patient-related outcomes in KOOS, both groups showed significant improvements in all subscales, but no difference was found between the groups. Functional return (FR) rate was almost double compared to the Swedish knee ligament register and treatment failure (TF) rate was reduced by half, no significant difference between the groups. No difference regarding cyclops removal, re-injury of ACL or meniscus was found between the two surgical timing groups.
Conclusion
Acute ACLR within 8 days of injury does not appear to adversely affect ROM or result in increased stiffness in the knee joint and was not inferior to the delayed group in any assessment when compared to delayed surgery.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute anterior cruciate ligament (ACL) rupture is a common and serious injury to the knee. The incidence in Sweden is close to 80/100,000 inhabitants, with non-contact ACL injuries most commonly occurring in athletes who participate in pivoting sports such as soccer, handball, and alpine skiing [33]. Though it has been established that ACL reconstruction (ACLR) decreases pathological knee laxity and reduces episodes of instability [13, 20, 29], many patients never return to their pre-injury activity level. In addition, irrespective of how the injury is treated, many patients later develop osteoarthritis (OA) of the knee and studies comparing long-term outcomes following ACLR compared to non-operative treatment have not demonstrated consistent results [12, 13, 16].
While it is generally agreed that ACLR is indicated for patients with signs of instability and a desire to resume a high activity level in pivoting sports, the optimal timing of ACLR has not yet been determined. The current recommendation is to delay ACLR after an acute injury due to the risk of arthrofibrosis and suboptimal clinical results [28, 37]. However, several studies have shown similar postoperative range of motion (ROM) regardless of whether surgery was performed within 48 h, 2 weeks, or if ACLR was delayed for a minimum of 6 weeks [1, 10, 17, 22, 30]. Early ACLR can facilitate early return to sport and work, and has been reported to be more cost effective, while increased time between injury and surgical intervention is associated with increased incidence of meniscus and cartilage injuries [9, 20, 23, 34].
In an initial study, involving patients with high activity levels, compared outcomes following ACLR performed within 8 days of injury to surgery 6–10-week postinjury and demonstrated no significant differences in ROM at 6-month follow-up [10]. In this study, outcomes for the two groups were assessed at a minimum of 24-month post-surgery. It was hypothesized that an acute ACLR would not result in inferior patient-reported outcomes nor a higher frequency of ROM deficits.
Materials and methods
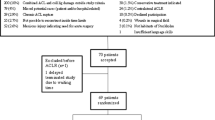
Active adults between 18 and 40 years of age who presented to the Orthopaedics Department of Stockholm South Hospital with an acute ACL rupture in a previously healthy knee were enrolled in the study. Exclusion criteria were: Tegner activity level [35] below level 6, major cartilage or meniscus injury on MRI requiring acute surgery, signs of OA on acute radiograph, a medial collateral ligament injury grade 2 or more, or multiple ligament injuries. During this period, 2,088 patients were assessed and 70 patients were included and randomized with the sealed envelope technique. One patient in the delayed group dropped out before surgery due to personal reasons. In an intial study, the details of recruitment process, full inclusion and exclusion criteria, patient demographics, and the randomization process have previously been published [10]. All patients provided written informed consent prior to study participation.
All reconstructions were performed using anatomical single-bundle hamstring grafts and all patients underwent a standardized rehabilitation protocol at one physiotherapy center, with full weight bearing allowed from day 1.
Patient evaluation
Demographic data were obtained at baseline and included patient age, gender, injured side, time from injury to surgery, and concomitant injuries. Knee injury and osteoarthritis outcome score (KOOS) [26], Lysholm score [35] and Tegner activity level were obtained preoperatively. Patient-reported Tegner activity level refers prior to injury was also recorded. Preoperative examination was completed with a physical examination, including ROM (passive ROM measured with a goniometer and reported as a deficit in extension and flexion), instrumented laxity using the Rolimeter and thigh-circumference measured 10 cm proximal to the proximal pole of the patella. Follow-up examinations were performed at 6, 12, and 24 months postoperatively and included the same scores as preoperatively as well as functional strength test assessed with the single leg hop. Isokinetic peak torque strength at 60°, 180°, and 240°/s, and isometric torque strength at 60° and 180°, in both extension and flexion was measured with Biodex®. ACL graft failures, contralateral ACL ruptures and meniscal repair failures requiring revision meniscus surgery were recorded.
The study was approved by the regional ethics committee at the Karolinska Institute, Stockholm Sweden (reference no. 2006/404-31/3/2008/1541-32).
Statistical analysis
Statistical analysis was performed with the IBM SPSS 25.0 software package for Macintosh. Nominal variables were tested by the χ2 test or the Fisher’s exact test. Ordinal variables and non-normally distributed interval and scale variables were evaluated by the Mann–Whitney U test, and the Student’s t test was used for normally distributed scale variables in independent groups. Longitudinal statistics were done with the paired-samples t test for normally distributed scale variables and the Wilcoxon signed-rank test for ordinal and non-normally distributed scale variables. The tests were two-sided. The results were considered significant at p < 0.05.
A sample size calculation was performed using the primary outcome variable ROM at 3 months. If the mean difference between the groups was 5° or more (corresponding to means of 122.5 vs. 117.5) and the common within-group standard deviation was 7.0, a sample size of 32 patients in each of the two groups would have a power of 80% to yield a statistically significant result, with 5% risk of a type-one error.
Results
Demographic data of the study groups are displayed in Table 1. The only significant difference between group I (acute reconstruction) and group II (delayed reconstruction) was the time between injury and reconstruction. Despite several attempts to contact all patients by both mail and telephone, not all patients attended the 2-year clinical visit. Twelve (17%) patients were lost to follow-up, with no significant difference between groups I and II.
Patient-related outcome
As shown in Table 2 and Fig. 1, no difference in patient-related outcome score was found. Lysholm, KOOS, and Tegner showed no statistically significant differences between the acute and delayed treatment groups. Median Tegner level was restored to pre-injury and desired levels in both groups, with almost all patients returning to Tegner activity level 6 or higher, i.e., knee-strenuous sports.
Functional recovery (FR) and treatment failure (TF)
Functional recovery was defined as a Knee Osteoarthritis Outcome Score (KOOS) above: 90 for Pain, 84 for Symptoms, 91 for ADL, 80 for Sport/Rec, and 81 for quality of life (QoL). TF was defined as a KOOS, QoL < 44 [4]. No significant difference between the groups, almost 40% in each group achieved FR, was found.
Objective IKDC and manual laxity measurements
The overall objective IKDC as well as manual laxity measurements did not display any significant differences between the acute and delayed surgery patients. It also showed high scores in both groups, with almost all patients within grade AB (normal to nearly normal), as presented in Table 2.
Passive range of motion
The distribution of range of motion scores according to deficits in flexion and extension at 24 months in the study groups is presented in Table 2. No statistically significant difference was found between the acute and delayed treatment groups in patients with an isolated ACL tear. The patients with an extension deficit at 3-month follow-up had regained their ROM by 24 months, i.e., those found to have an extension deficit at 24 months had lost ROM subsequent to the 3-month follow-up.
Functional strength
Similar results were found in the groups regarding muscle circumference and functional strength measured with the one leg hop test. However, significant differences were found in isokinetic flexion between groups during the Biodex test, Table 2. Values in the acute group were significantly higher for the flexor muscles at 180° and 240°/s, by 8.1% (p = 0.05) and 9.4% (p = 0.01), respectively. The other strength assessments performed were not statistically different, although higher values were found for group I.
Additional surgery
There was additional surgery in six cases (18%) of the acute group and 13 (37%) of the delayed (n.s.), Table 3. One patient in each group sustained a graft rupture during the study period and both reported a new significant trauma. Arthroscopic removal of a cyclops lesion was necessary in 6 patients in the delayed group and one in the acute.
Discussion
The most important finding of this randomized control trial is that good clinical results can be achieved 24 months after acute ACLR and that early extension deficits seen at the 3-month follow-up had resolved.
This study supports the findings of other recent studies which have demonstrated that the timing of ACLR does not influence postoperative ROM [1, 7, 10, 17, 24] and contradicts the findings of older studies including Shelbourne et al. [25, 28, 37]. These differences may be due to the fact that these older studies were performed without the use of contemporary arthroscopic techniques, were retrospective, and perhaps most importantly had a more restrictive postoperative rehabilitation regime. In addition, a lack of classification in the literature regarding which timeframe constitutes acute vs. delayed surgery makes it difficult to compare these studies [11]. In this study, acute reconstruction did not result in increased stiffness. There were superior outcomes for the acute group regarding strength and how the patient perceived their knee function at 24 months. In addition, the acute group was not inferior to the delayed group in any assessment. Regarding patient-related outcomes in KOOS, both groups showed significant improvements in all subscales, but no difference was found between the groups. The KOOS results were also slightly better than those from the Swedish anterior cruciate ligament registry [2] and the results from a US cohort study [32]. This further supports the fact that acute ACLR is a safe option.
Non-operative treatment of an ACL injury remains an option and can yield satisfactory results [13, 15, 31], although the body of evidence is limited due to the scarcity of randomized studies. Frobell et al. concluded that for adults with acute ACL injuries, there is no difference between surgical management (ACL reconstruction followed by structured rehabilitation) and non-operative treatment (structured rehabilitation only) in patient‐reported outcomes of knee function at 2 and 5 years after injury. However, nearly, 50% of the participants with an ACL rupture remained symptomatic following rehabilitation and later opted for ACL reconstruction surgery [13].
An association between the time from injury to surgery and the risk of additional medial meniscal injuries and chondral injuries has been reported by several studies investigating ACL injuries [4,5,6, 19]. Chhadia et al. found a significant association between medial meniscal injury, as well as medial and lateral compartment chondral injury, and delayed surgery (beyond 6 and 12 months) [8]. With the increased risk for further injuries, it is questionable whether initial non-operative treatment in patients with a high pre-injury activity level is the best alternative.
Anterior cruciate ligament reconstruction is commonly recommended for patients who participate in pivoting sports and aspire to return to pre-injury sports participation. The rates of return to pre-injury level of sport following ACLR differ between studies and between elite and non-elite athletes (83% vs. 63%) [3, 21]. Using pre-injury level of sport as a measure of successful surgery may not accurately reflect positive outcomes, for example, patients with pre-injury Tegner levels of ten who subsequently return to a score of eight. The study confirms that while not all patients did return to pre-injury level of sport, almost all could return to a knee-strenuous sport. No significant difference between the groups in this regard was found, but it was noted that fewer had returned in the acute group. A further in-depth analysis of these acutely operated patients who did not return to knee-strenuous sport found that they did not demonstrate inferior outcomes in any subjective or objective assessment when compared to patients who returned to their previous activity level. Furthermore, the FR and TR did not differ between those who returned and those who did not. KOOS also showed higher score in sport/req, even though fewer returned to the same Tegner levels. As such, it is unclear why they did not return to their previous level. As this study was not designed specifically to look at return to sport, one explanation of this finding could be a type 2 error, due to too few patients being included in the study to be able to accurately assess return to sport outcomes.
The ACL graft failure rate in this study was low and did not differ between the groups (2.9%) [14, 18].
The FR rate was almost double that seen in a previous study found in the Swedish Knee Ligament Register (SKLR) [4]. Although waiting time itself does not have an impact on the outcome, it can be argued that an acute or early ACLR, which is performed before recurrent giving ways occur, increases the likelihood of achieving FR. The study also showed that TF was reduced by half in the acute group compared to the SKLR. This suggests early surgery, before recurring giving ways have occurred, decreases additional injuries, and increases the likelihood of FR. Finally, it should be mentioned that an acute ACLR has been shown to be more cost-effective than delayed surgery, and time spent on rehabilitation before the surgery is better utilized postoperatively [23, 27, 36].
The major strength of this study is its prospective, randomized design and the use of the same surgical technique. Furthermore, one center with the same postoperative rehabilitation protocol was used in both groups. The two groups were also comparable in terms of age, gender and pre-injury Tegner activity level, factors which could contribute to selection bias in a non-randomized trial.
Potential limitations are the limited number of patients. Though there were sufficient numbers according to the power analysis for the primary endpoint, there may not have been enough patients included to detect other significant differences. A further limitation was the change in surgical method during the study period (transtibial vs. femoral portal drilling). Furthermore, there were a relative high number of patients who were lost to the latest follow-up, although with no difference between the groups.
Conclusion
This study provides further evidence that acute ACL reconstruction can be performed safely without an increased risk of developing stiffness. Thus, clinicians can make their decision about the optimal time for surgery for each individual patient based on other parameters and plan acute reconstruction if indicated.
Change history
18 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00167-021-06500-3
References
Andernord D, Karlsson J, Musahl V, Bhandari M, Fu FH, Samuelsson K (2013) Timing of surgery of the anterior cruciate ligament. Arthroscopy 29:1863–1871
Ardern CL, Sonesson S, Forssblad M, Kvist J (2017) Comparison of patient-reported outcomes among those who chose ACL reconstruction or non-surgical treatment. Scand J Med Sci Sports 27:535–544
Ardern CL, Webster KE, Taylor NF, Feller JA (2011) Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med 45:596–606
Barenius B, Forssblad M, Engstrom B, Eriksson K (2013) Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 21:914–927
Barenius B, Nordlander M, Ponzer S, Tidermark J, Eriksson K (2010) Quality of life and clinical outcome after anterior cruciate ligament reconstruction using patellar tendon graft or quadrupled semitendinosus graft: an 8-year follow-up of a randomized controlled trial. Am J Sports Med 38:1533–1541
Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K (2014) Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med 42:1049–1057
Bottoni CR, Liddell TR, Trainor TJ, Freccero DM, Lindell KK (2008) Postoperative range of motion following anterior cruciate ligament reconstruction using autograft hamstrings: a prospective, randomized clinical trial of early versus delayed reconstructions. Am J Sports Med 36:656–662
Chhadia AM, Inacio MC, Maletis GB, Csintalan RP, Davis BR, Funahashi TT (2011) Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med 39:1894–1899
de Campos GC, Nery W, Teixeira PE, Araujo PH, Alves WM (2016) Association between meniscal and chondral lesions and timing of anterior cruciate ligament reconstruction. Orthop J Sports Med 4:2325967116669309
Eriksson K, von Essen C, Jönhagen S, Barenius B (2018) No risk of arthrofibrosis after acute anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26:2875–2882
Flint JH, Wade AM, Giuliani J, Rue JP (2014) Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med 42:235–241
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS (2010) A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 363:331–342
Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS (2013) Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ 346:f232
Gabler CM, Jacobs CA, Howard JS, Mattacola CG, Johnson DL (2016) Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: a systematic review, meta-analysis, and meta-regression. Am J Sports Med 44:1069–1079
Gföller P, Abermann E, Runer A, Hoser C, Pflüglmayer M, Wierer G et al (2019) Non-operative treatment of ACL injury is associated with opposing subjective and objective outcomes over 20 years of follow-up. Knee Surg Sports Traumatol Arthrosc 27:2665–2671
Grindem H, Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA (2012) A pair-matched comparison of return to pivoting sports at 1 year in anterior cruciate ligament-injured patients after a nonoperative versus an operative treatment course. Am J Sports Med 40:2509–2516
Herbst E, Hoser C, Gföller P, Hepperger C, Abermann E, Neumayer K et al (2017) Impact of surgical timing on the outcome of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:569–577
Kaeding CC, Léger-St-Jean B, Magnussen RA (2017) Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med 36:1–8
Kay J, Memon M, Shah A, Yen YM, Samuelsson K, Peterson D et al (2018) Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 26:3738–3753
Krutsch W, Zellner J, Baumann F, Pfeifer C, Nerlich M, Angele P (2017) Timing of anterior cruciate ligament reconstruction within the first year after trauma and its influence on treatment of cartilage and meniscus pathology. Knee Surg Sports Traumatol Arthrosc 25:418–425
Lai CCH, Ardern CL, Feller JA, Webster KE (2018) Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med 52:128–138
Marcacci M, Zaffagnini S, Iacono F, Neri MP, Petitto A (1995) Early versus late reconstruction for anterior cruciate ligament rupture. Results after five years of followup. Am J Sports Med 23:690–693
Mather RC, Hettrich CM, Dunn WR, Cole BJ, Bach BR, Huston LJ et al (2014) Cost-effectiveness analysis of early reconstruction versus rehabilitation and delayed reconstruction for anterior cruciate ligament tears. Am J Sports Med 42:1583–1591
Meighan AA, Keating JF, Will E (2003) Outcome after reconstruction of the anterior cruciate ligament in athletic patients. A comparison of early versus delayed surgery. J Bone Joint Surg Br 85:521–524
Mohtadi NG, Webster-Bogaert S, Fowler PJ (1991) Limitation of motion following anterior cruciate ligament reconstruction. A case-control study. Am J Sports Med 19:620–624 (discussion 624–625)
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and Osteoarthritis Outcome Score (KOOS)–validation of a Swedish version. Scand J Med Sci Sports 8:439–448
Saltzman BM, Cvetanovich GL, Nwachukwu BU, Mall NA, Bush-Joseph CA, Bach BR Jr (2016) Economic analyses in anterior cruciate ligament reconstruction: a qualitative and systematic review. Am J Sports Med 44:1329–1335
Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M (1991) Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med 19:332–336
Signorelli C, Filardo G, Bonanzinga T, Grassi A, Zaffagnini S, Marcacci M (2016) ACL rupture and joint laxity progression: a quantitative in vivo analysis. Knee Surg Sports Traumatol Arthrosc 24:3605–3611
Smith TO, Davies L, Hing CB (2010) Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 18:304–311
Smith TO, Postle K, Penny F, McNamara I, Mann CJ (2014) Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee 21:462–470
Spindler KP, Huston LJ, Wright RW, Kaeding CC, Marx RG, Amendola A et al (2011) The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med 39:348–359
Swedish (2017) Swedish National Knee Ligament Register. Swedish national ACL database homepage. http://www.aclregister.nu
Taketomi S, Inui H, Yamagami R, Kawaguchi K, Nakazato K, Kono K et al (2018) Surgical timing of anterior cruciate ligament reconstruction to prevent associated meniscal and cartilage lesions. J Orthop Sci 23:546–551
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
von Essen C, McCallum S, Barenius B, Eriksson K (2019) Acute reconstruction results in less sick-leave days and as such fewer indirect costs to the individual and society compared to delayed reconstruction for ACL injuries. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05397-3
Wasilewski SA, Covall DJ, Cohen S (1993) Effect of surgical timing on recovery and associated injuries after anterior cruciate ligament reconstruction. Am J Sports Med 21:338–342
Acknowledgements
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding has been received for this study.
Ethical approval
The study was approved by the regional ethics committee at the Karolinska Institute, Stockholm Sweden (reference no. 2006/404-31/3/2008/1541-32).
Informed consent
Informed consent was obtained by each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
von Essen, C., Eriksson, K. & Barenius, B. Acute ACL reconstruction shows superior clinical results and can be performed safely without an increased risk of developing arthrofibrosis. Knee Surg Sports Traumatol Arthrosc 28, 2036–2043 (2020). https://doi.org/10.1007/s00167-019-05722-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05722-w