Abstract
Purpose
Following total knee arthroplasty (TKA), high tibial forces, large differences in tibial forces between the medial and lateral compartments, and anterior translation of the contact locations of the femoral component on the tibial component during passive flexion indicate abnormal knee function. Because the goal of kinematically aligned TKA is to restore native knee function without soft tissue release, the objectives were to determine how well kinematically aligned TKA limits high tibial forces, differences in tibial forces between compartments, and anterior translation of the contact locations of the femoral component on the tibial component during passive flexion.
Methods
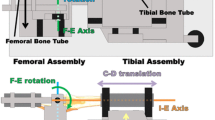
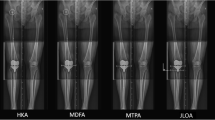
Using cruciate retaining components, kinematically aligned TKA was performed on thirteen human cadaveric knee specimens with use of manual instruments without soft tissue release. The tibial forces and tibial contact locations were measured in both the medial and lateral compartments from 0° to 120° of passive flexion using a custom tibial force sensor.
Results
The average total tibial force (i.e. sum of medial + lateral) ranged from 5 to 116 N. The only significant average differences in tibial force between compartments occurred at 0° of flexion (29 N, p = 0.0008). The contact locations in both compartments translated posteriorly in all thirteen kinematically aligned TKAs by an average of 14 mm (p < 0.0001) and 18 mm (p < 0.0001) in the medial and lateral compartments, respectively, from 0° to 120° of flexion.
Conclusions
After kinematically aligned TKA, average total tibial forces due to the soft tissue restraints were limited to 116 N, average differences in tibial forces between compartments were limited to 29 N, and a net posterior translation of the tibial contact locations was observed in all kinematically aligned TKAs during passive flexion from 0° to 120°, which are similar to what has been measured previously in native knees. While confirmation in vivo is warranted, these findings give surgeons who perform kinematically aligned TKA confidence that the alignment method and surgical technique limit high tibial forces, differences in tibial forces between compartments, and anterior translation of the tibial contact locations during passive flexion.














Similar content being viewed by others
References
Amis AA, Dawkins GP (1991) Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br 73(2):260–267
Amis AA, Gupte CM, Bull AM, Edwards A (2006) Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 14(3):257–263
Arnold EM, Ward SR, Lieber RL, Delp SL (2010) A model of the lower limb for analysis of human movement. Ann Biomed Eng 38(2):269–279
Babazadeh S, Stoney JD, Lim K, Choong PFM (2009) The relevance of ligament balancing in total knee arthroplasty: how important is it? A systematic review of the literature. Orthop Rev (Pavia). doi:10.4081/or.2009.e26
Bach JM, Hull ML (1995) A new load application system for in vitro study of ligamentous injuries to the human knee joint. J Biomech Eng 117(4):373–382
Banks S, Bellemans J, Nozaki H, Whiteside LA, Harman M, Hodge WA (2003) Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res 410(5):131–138
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84(1):50–53
Bellemans J, Vandenneucker H, Vanlauwe J, Victor J (2010) The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sports Traumatol Arthrosc 18(2):152–156
Belvedere C, Ensini A, Feliciangeli A, Cenni F, D’Angeli V, Giannini S, Leardini A (2012) Geometrical changes of knee ligaments and patellar tendon during passive flexion. J Biomech 45(11):1886–1892
Blankevoort L, Huiskes R, de Lange A (1988) The envelope of passive knee joint motion. J Biomech 21(9):705–720
Defrate LE, Nha KW, Papannagari R, Moses JM, Gill TJ, Li G (2007) The biomechanical function of the patellar tendon during in vivo weight-bearing flexion. J Biomech 40(8):1716–1722
Delport P, Labey L, De Corte R, Innocenti B, Vander Sloten J, Bellemans J (2013) Collateral ligament strains during knee joint laxity evaluation before and after TKA. Clin Biomech (Bristol, Avon) 28(7):777–782
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 96-B(7):907–913
Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG (2012) Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 35(2):e160–e169. doi:10.3928/01477447-20120123-04
Elmallah RK, Mistry JB, Cherian JJ, Chughtai M, Bhave A, Roche MW, Mont MA (2016) Can we really "Feel" a balanced total knee arthroplasty? J Arthroplasty 31(9 Suppl):102–105
Erskine RM, Jones DA, Maganaris CN, Degens H (2009) In vivo specific tension of the human quadriceps femoris muscle. Eur J Appl Physiol 106(6):827–838
Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Amis AA (2012) Length-change patterns of the collateral ligaments after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(7):1349–1356
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105(2):136–144
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty 29(5):955–960
Gustke KA, Golladay GJ, Roche MW, Jerry GJ, Elson LC, Anderson CR (2014) Increased satisfaction after total knee replacement using sensor-guided technology. Bone Joint J 96-B(10):1333–1338
Harner CD, Giffin JR, Vogrin TM, Woo SLY (2001) Anatomy and biomechanics of theposterior cruciate ligament and posterolateral corner. Oper Techn Sport Med 9(2):39–46
Heesterbeek PJ, Verdonschot N, Wymenga AB (2008) In vivo knee laxity in flexion and extension: a radiographic study in 30 older healthy subjects. Knee 15(1):45–49
Hosseini A, Qi W, Tsai TY, Liu Y, Rubash H, Li G (2015) In vivo length change patterns of the medial and lateral collateral ligaments along the flexion path of the knee. Knee Surg Sports Traumatol Arthrosc 23(10):3055–3061
Howell SM, Hodapp EE, Vernace JV, Hull ML, Meade TD (2013) Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc 21(10):2281–2287
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2012) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471(3):1000–1007
Howell SM, Hull ML, Mahfouz MR (2017) Kinematically aligned total knee arthroplasty. In: Scott S (ed) Insall and Scott Surgery of the Knee, 6th edn. Elsevier, Philadelphia, PA, pp 1784–1796
Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML (2015) Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop 39(11):2117–2124
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21(10):2271–2280
Hunt NC, Ghosh KM, Blain AP, Athwal KK, Rushton SP, Amis AA, Longstaff LM, Deehan DJ (2014) How does laxity after single radius total knee arthroplasty compare with the native knee? J Orthop Res 32(9):1208–1213
LaPrade RF, Bollom TS, Wentorf FA, Wills NJ, Meister K (2005) Mechanical properties of the posterolateral structures of the knee. Am J Sports Med 33(9):1386–1391
Li G, Most E, Sultan PG, Schule S, Zayontz S, Park SE, Rubash HE (2004) Knee kinematics with a high-flexion posterior stabilized total knee prosthesis: an in vitro robotic experimental investigation. J Bone Joint Surg Am 86-A(8):1721–1729
Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SL (1999) The importance of quadriceps and hamstring muscle loading on knee kinematics and in situ forces in the ACL. J Biomech 32(4):395–400
Lu TW, Tsai TY, Kuo MY, Hsu HC, Chen HL (2008) In vivo three-dimensional kinematics of the normal knee during active extension under unloaded and loaded conditions using single-plane fluoroscopy. Med Eng Phys 30(8):1004–1012
Markolf KL, Gorek JF, Kabo JM, Shapiro MS (1990) Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg Am 72(4):557–567
Meneghini RM, Ziemba-Davis MM, Lovro LR, Ireland PH, Damer BM (2016) Can intraoperative sensors determine the “target” ligament balance? Early outcomes in total knee arthroplasty. J Arthroplasty 31(10):2181–2187
Merican AM, Ghosh KM, Deehan DJ, Amis AA (2009) The transpatellar approach for the knee in the laboratory. J Orthop Res 27(3):330–334
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J 96-B(11 Supple A):96–100
Nedopil AJ, Howell SM, Hull ML (2016) Does malrotation of the tibial and femoral components compromise function in kinematically aligned total knee arthroplasty? Orthop Clin North Am 47(1):41–50
Neter J, Kutner MH, Nachtsheim CJ, Wasserman W (1996) Analysis of factor effects in two-factor studies-equal sample sizes. In: Irwin (ed) Applied linear statistical models. 4th edn. McGraw-Hill, Chicago, pp 849-874
Pinskerova V, Johal P, Nakagawa S, Sosna A, Williams A, Gedroyc W, Freeman MA (2004) Does the femur roll-back with flexion? J Bone Joint Surg Br 86(6):925–931
Pottenger LA, Phillips FM, Draganich LF (1990) The effect of marginal osteophytes on reduction of varus-valgus instability in osteoarthritic knees. Arthritis Rheum 33(6):853–858
Powers CM, Chen YJ, Scher IS, Lee TQ (2010) Multiplane loading of the extensor mechanism alters the patellar ligament force/quadriceps force ratio. J Biomech Eng 132(2):024503
Race A, Amis AA (1994) The mechanical properties of the two bundles of the human posterior cruciate ligament. J Biomech 27(1):13–24
Robinson JR, Bull AM, Amis AA (2005) Structural properties of the medial collateral ligament complex of the human knee. J Biomech 38(5):1067–1074
Roth JD, Howell SM (2017) Soft tissue balance of the native knee provides guidance for balancing a total knee arthroplasty. In: Matsuda S, Lustig S, van der Merwe W (eds) Soft Tissue Balancing in Total Knee Arthroplasty, pp 17–27
Roth JD, Howell SM, Hull ML (2015) Native knee laxities at 0°, 45°, and 90° of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Joint Surg Am 97(20):1678–1684
Roth JD, Howell SM, Hull ML (2017) Characterization and correction of errors in computing contact location between curved articular surfaces: application to total knee arthroplasty. J Biomech Eng 139(6). doi:10.1115/1.4036147
Roth JD, Howell SM, Hull ML (2017) An improved tibial force sensor to compute contact forces and contact locations in vitro after total knee arthroplasty. J Biomech Eng 139(4):041001–041008
Roth JD, Hull ML, Howell SM (2015) The limits of passive motion are variable between and unrelated within normal tibiofemoral joints. J Orthop Res 33(11):1594–1602
Sharma A, Dennis DA, Zingde SM, Mahfouz MR, Komistek RD (2014) Femoral condylar contact points start and remain posterior in high flexing patients. J Arthroplasty 29(5):945–949
Sharma L, Lou C, Felson DT, Dunlop DD, Kirwan-Mellis G, Hayes KW, Weinrach D, Buchanan TS (1999) Laxity in healthy and osteoarthritic knees. Arthritis Rheum 42(5):861–870
Verstraete MA, Meere PA, Salvadore G, Victor J, Walker PS (2017) Contact forces in the tibiofemoral joint from soft tissue tensions: implications to soft tissue balancing in total knee arthroplasty. J Biomech 58:195–202
Ward SR, Eng CM, Smallwood LH, Lieber RL (2009) Are current measurements of lower extremity muscle architecture accurate? Clin Orthop Relat Res 467(4):1074–1082
Watanabe T, Ishizuki M, Muneta T, Banks SA (2013) Knee kinematics in anterior cruciate ligament-substituting arthroplasty with or without the posterior cruciate ligament. J Arthroplasty 28(4):548–552
Whiteside LA (2002) Soft tissue balancing: the knee. J Arthroplasty 17(4 Suppl 1):23–27
Whiteside LA, Saeki K, Mihalko WM (2000) Functional medial ligament balancing in total knee arthroplasty. Clin Orthop Relat Res 380(11):45–57
Wilson DR, Feikes JD, O’Connor JJ (1998) Ligaments and articular contact guide passive knee flexion. J Biomech 31(12):1127–1136
Wilson DR, Feikes JD, Zavatsky AB, O’Connor JJ (2000) The components of passive knee movement are coupled to flexion angle. J Biomech 33(4):465–473
Acknowledgements
We acknowledge the support of the National Science Foundation (NSF), Award # CBET-1067527. We also acknowledge the support of Zimmer Biomet. We also would like to thank individuals who donate their remains and tissues for the advancement of education and research.
Author information
Authors and Affiliations
Contributions
JDR, MLH, and SMH collectively conceived of and designed the study. JDR carried out data collection and analysis. JDR and MLH drafted the manuscript. JDR, MLH, and SMH read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Two of the authors received research support from Zimmer Biomet related to this study (MLH and SMH). Two of the authors received research support from Think Surgical for unrelated studies (JDR and MLH). One of the authors is a paid consultant of Zimmer Biomet and Think Surgical (SMH). One of the authors received royalties from Saunders/Mosby-Elsevier and Zimmer Biomet (SMH).
Funding
This study was funded by the National Science Foundation (Award No. CBET-1067527) and Zimmer Biomet (Award No. CW88095).
Ethical approval
Following University of California policies, this study did not require institutional review board (IRB) approval because de-identiied cadaveric specimens were used.
Informed consent
The informed consent does not apply to this study because de-identified cadaveric specimens were used.
Appendices
Appendix 1: Contribution of applied muscle loads to differences in tibial forces between compartments
The differences in tibial forces between compartments (F diff,i ) created by the applied muscle loads at each flexion angle (i = 0°, 30°, 60°, 90°, and 120°) can be estimated using average anatomy and lines of action [3, 11] (Fig. 10, Eq. 1) where \( \overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {r}_{\text{BF}} \), \( \overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {r}_{\text{SMST}} \), and \( \overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {r}_{\text{Q}} \) are the vectors from the centre of the tibial plateau to the tibial insertions of the biceps femoris (BF), semitendinosus/semimembranosus (SMST), and the patellar tendon (Q), respectively; \( \overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {F}_{{{\text{BF}},i}} \), \( \overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {F}_{{{\text{SMST}},i}} \), and \( \overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {F}_{{{\text{Q}},i}} \) are the vectors whose orientation is set by the line of action and magnitude is set by the applied loads at the tibial insertions of the biceps femoris, semitendinosus/semimembranosus, and the patellar tendons, respectively; w is the average medial–lateral spacing between the contact locations in the medial and lateral compartments. The magnitude of \( \overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {F}_{{{\text{Q}},i}} \) was computed using the average ratio of the load in the quadriceps tendon to that in the patellar tendon [42].
Appendix 2: Anterior–posterior and compression–distraction components of applied muscle loads
The total tibial force (F total,i ) can be decomposed into the contribution of the muscle loads (F muscle,i ) and the contribution of the soft tissue restraints (\( F_{{{\text{soft}}\;{\text{tissue}},i}} \)) at each flexion angle (i = 0°, 10°, 30°, 45°, 60°, 90°, and 120°) (Eq. 2). The total tibial force is calculated as the sum of the medial and lateral tibial forces computed using the tibial force sensor. The anterior–posterior (A–P) and compression–distraction (C–D) components of the muscle loads are computed based on applied load to each muscle, the alignment of the muscle loads relative to the tibia [3, 11], and the ratio of the load in the quadriceps tendon to that in the patellar tendon (r Q/Pat,i ) [42] (Fig. 12).
Between 0° and 30° of flexion, the net A–P force component of the muscle loads is directed anteriorly, whereas between 30° and 120° of flexion, the net A–P force component of the muscle loads is directed posteriorly (Fig. 13). The anterior translation of both tibial contact locations between 30° and 90° (Fig. 8; Table 2) is likely driven by the muscle forces pulling the tibia posteriorly on the femur. Because the soft tissues are minimally loaded between these flexion angles (Fig. 14), the small A–P forces applied by the muscles can drive the A–P translation of the tibial contact locations.
Rights and permissions
About this article
Cite this article
Roth, J.D., Howell, S.M. & Hull, M.L. Kinematically aligned total knee arthroplasty limits high tibial forces, differences in tibial forces between compartments, and abnormal tibial contact kinematics during passive flexion. Knee Surg Sports Traumatol Arthrosc 26, 1589–1601 (2018). https://doi.org/10.1007/s00167-017-4670-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4670-z