Abstract
Orthopedic patients are frequently affected by temporary phases of immobility during the course of traumatic/degenerative joint diseases and particularly after joint surgery. These phases are usually accompanied by a significant loss of muscle mass and strength. However, since the patients’ load capacity is usually reduced, physicians and physiotherapists are often faced with the dilemma of not being able to offer an adequate therapeutic strategy for muscle preservation or early muscle building, since the high mechanical loads required for this in the training process are usually not feasible or even contraindicated for a certain period of time. In recent years, a training technique originating from sports science, called blood flow restriction (BFR) training, has increasingly been used in preoperative therapy or for rehabilitation. As the BFR method uses special blood pressure cuffs to occlude venous outflow from the exercising limb during exclusively low mechanical load strength training, the significant effects of muscle hypertrophy demonstrated by this method are of greatest interest to rehabilitation research. This article focuses on the training technique, the underlying mechanisms and potential risks, as well as integration of the technique into the clinical rehabilitation process based on existing data. Furthermore, this article provides the basis for a future consensus paper to validate the usability and effectiveness of BFR training in the conservative and rehabilitative therapeutic phases of joint surgery.
Zusammenfassung
Orthopädische Patienten leiden während des Verlaufs von traumatisch oder degenerativ bedingten Gelenkerkrankungen oftmals unter temporären Phasen der Immobilität, insbesondere nach Gelenkoperationen. Solche Phasen gehen gewöhnlich mit einem beträchtlichen Verlust an Muskelmasse und -kraft einher. Da jedoch die Belastungskapazität der Patienten üblicherweise vermindert ist, stehen die Ärzte und Physiotherapeuten häufig vor dem Problem, keine passende therapeutische Strategie für den Muskelerhalt oder frühen Muskelaufbau anbieten zu können. Die für diesen Trainingsprozess erforderlichen hohen mechanischen Belastungen, sind gewöhnlich nicht praktikabel oder sogar für eine bestimmte Zeit kontraindiziert. In den letzten Jahren wurde zunehmend eine Trainingstechnik in der präoperativen Therapie oder Rehabilitation eingesetzt, die ursprünglich aus der Sportwissenschaft stammt, nämlich das Blutflussrestriktionstraining (BFR-Training). Da bei der BFR-Methode spezielle Blutdruckmanschetten zur Okklusion des venösen Ausflusses aus der trainierenden Extremität während eines Krafttrainings mit ausschließlich geringer mechanischer Belastung verwendet werden, sind die signifikanten Effekte auf die Muskelhypertrophie, die mit dieser Methode erzielt werden, von größtem Interesse für die Rehabilitationsforschung. Im vorliegenden Beitrag liegt der Fokus auf der Trainingstechnik, den zugrunde liegenden Mechanismen und möglichen Risiken sowie der Integration dieser Technik in den klinischen Rehabilitationsprozess auf der Grundlage bestehender Daten. Darüber hinaus stellt der Beitrag die Basis für ein zukünftiges Konsenspapier dar, um die Anwendbarkeit und Wirksamkeit des BFR-Trainings in der konservativen und rehabilitativen Therapiephase der Gelenkchirurgie zu validieren.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Clinicians and scientists have recently been increasingly confronted with the term “blood flow restriction training” (BFR training). In the past decade, BFR training has been widly used in the rehabilitation of injuries as well as in prehabilitation and in sports, with the aim of enhancing muscle mass and strength by applying only low mechanical loads to the joints or the injured extremity. The idea of supporting the training stimulus by controlled hypoxia is not new but has now been taken up for rehabilitation as well, since it could be shown that under hypoxic conditions, similar effects can be achieved with low mechanical load training as with traditional strength training with high mechanical loads [1]. For rehabilitation purposes, this means that immobilization-induced muscle atrophy can be reduced and targeted hypertrophy training can be started earlier. Despite the rising number of research articles in this field and the increasing clinical use of BFR training, knowledge about this method among orthopedic surgeons is still relatively low. This was impressively demonstrated in a recent survey conducted by the Rehabilitation, Prevention, and Conservative Therapy Committee of the Association for Arthroscopy and Joint Surgery (AGA): of 551 experienced arthroscopists/joint surgeons (at least residency level) surveyed, only 42% reported knowing the BFR training technique and only 8% reported using this technique with their patients in rehabilitation. Standardized protocols were used by only 5% of the respondents (Degenhardt et al. manuscript in preparation).
The aim of this review is therefore to present the current state of knowledge regarding the indications, mode of action, and side effects of BFR training and to highlight the need for further research in relation to prehabilitation and rehabilitation. Subsequently, the preparation of a consensus paper on the use of BFR training in pre- and rehabilitation is aspired, involving the most important clinical societies and experienced BFR users.
Underlying mechanisms of blood flow restriction training
The underlying mechanisms of BFR-mediated muscular adaptations are still poorly understood. Several previous studies have shown that BFR training activates intracellular anabolic signaling cascades and satellite cells [2,3,4]. However, it is unclear what the exact trigger is. High mechanical strains, such as those involved in traditional strength training with high mechanical loads, as well as the associated microtrauma to muscles, are unlikely to occur during BFR training and consequently do not come into question as central anabolic signals.
Comparatively early, BFR exercise was observed to be associated with significantly increased levels of growth hormone (hGH) after exercise. For example, Takarada et al. [5] described in 2000 that after only five low-load sets (20% of one-repetition maximum [1 RM], 20 repetitions) on the leg extensor, the hGH concentration increased 290-fold from resting levels under BFR conditions. Current understanding is that these rises are caused by the accumulation of metabolites (e.g., lactate, H+, and K+) [6, 7], which is particularly pronounced under the hypoxic BFR conditions. However, the importance of acute, exercise-induced enhancements of anabolic hormones for muscle growth is under discussion to date [8,9,10]. Additionally, it is currently believed that although hGH itself induces anabolic effects in muscle as well, the primary effect is mediated via liver-released IGF‑1. However, the results on BFR-induced IGF‑1 rises are very heterogeneous [11,12,13]. Similarly, anabolic testosterone does not always seem to increase after BFR training [14, 15]. Therefore, the evidence that anabolic hormones are responsible for BFR-induced hypertrophy should be considered as low.
Another hypothesis is that the effects are induced by an altered neuromuscular recruitment pattern. For example, it is known that under physiological conditions, the body initially recruits slow-twitch muscle fibers (STF) at low resistances and only adds fast-twitch fibers (FTF) as the load increases [16]. This recruitment pattern is referred as Henneman’s size order principle [17]. However, due to the reduction of blood flow, premature fatigue of STF occurs and the muscle is pressured to recruit FTF despite the low resistance to counteract force reduction [18]. However, Suga et al. [19], who investigated FTF recruitment using 31P magnetic resonance spectroscopy, found FTF recruitment in only one third of subjects exercising with BFR (at 20% of the individual 1 RM). In comparison, more than two thirds of the subjects who trained without BFR but at 65% of their 1 RM recruited FTF fibers. Accordingly, it is unlikely that an altered recruitment pattern is the sole explanation for the BFR-mediated effects.
It is also conceivable that the metabolites themselves induce anabolic effects. For example, animal studies have shown that lactate can stimulate muscle growth [20], which could not be confirmed in human studies [21]. Furthermore, BFR-induced cell swelling has also been discussed as another possible trigger of anabolic signaling cascades. According to this theory, the fluid shift into the muscle cell triggered by intracellular accumulation of metabolites should create pressure from inside against the cytoskeleton and thus increase muscle protein synthesis. However, convincing results on this theory are also lacking so far. Overall, the mechanisms of BFR training-induced skeletal muscle adaptations remain largely unclear and further fundamental studies are needed (Fig. 1).
Mechanisms of action and effects of blood flow restriction training. Modified from: Saatmann, N. et al. [57]. GLUT4 glucose transporter type 4, IGF‑1 insulin-like growth factor 1, MAPK mitogen-activated protein kinase, IL‑6 interleukin 6, VEGF vascular endothelial growth factor, eNOS nitric oxide synthase, AMPK 5′-AMP-activated protein kinase
Clinical blood flow restriction training I: impact on functional recovery
Postoperative or posttraumatic immobilization and phases of unloading cause a loss of muscle mass and muscle strength [22, 23]. For example, Thomas et al. (2016) showed that 6 months after anterior cruciate ligament reconstruction (ACL-R), reductions in muscle cross-sectional area of about 15% and strength deficits of about 30% of the quadriceps muscles are still present compared with the non-operated leg [23]. Such muscular deficits are associated with movement compensations and performance limitations as well as decreased subjective knee joint function [24, 25]. To counteract the negative consequences of degeneration, moderate training loads of 60 to 80% of the 1 RM are recommended in training practice for inducing muscle hypertrophy, although maximal effects on muscle mass and strength benefit from higher loads (> 80% 1 RM) [26]. However, in early to mid-stages of rehabilitation, high mechanical loads are contraindicated and should be administered in a periodized schedule only after pain, swelling, and neuronal inhibition processes have subsided [27]. Therefore, to bridge as well as to mitigate atrophy effects, alternative training methods that allow early muscle hypertrophy and strength gains without the use of high mechanical loads are important. Consequently, the described characteristics of BFR training could represent a promising approach for clinical practice through the use of only low mechanical loads, and represent a currently insufficiently explored opportunity for functional rehabilitation in phases of impaired joint function [28].
For athletic and healthy populations, numerous studies have already demonstrated the comparability of low-load BFR training and high-load strength training (60–80% 1 RM) in terms of enhancement of muscle mass and strength [29,30,31,32]. However, meta-analysis has revealed that greater effects on muscle strength were observed after high-load strength training (> 65% 1 RM) than after BFR training [30]. For the clinical setting, there are basically two useful fields of BFR application: passive BFR (pBFR training) or active BFR training. In pBFR, only the metabolic stress is applied by venous occlusion and arterial hypoxemia, without associated mechanical loading of the affected muscles. This form of exercise is particularly suitable during periods of immobilization and bed rest, where active exercising is difficult to implement or contraindicated [33]. For example, Takarada et al. (2000) and Kubota et al. (2008) showed that intermittent pBFR applications can effectively mitigate a 2‑week immobilization-induced muscle atrophy [34, 35]. In contrast, Iversen et al. (2016) did not observe any reduction in muscle atrophy by similar pBFR protocols in the postoperative period after ACL‑R [36].
To counteract the negative effects of immobilization after surgery, neuromuscular stimulation (NMES) has been proposed as an additive method of increasing protein biosynthesis, muscle strength, and joint function after knee surgery [37]. Positive effects of NMES have been described in patients during the direct postoperative period when high-load strength training is still contraindicated, thus indicating a potential field of use overlapping with BFR. Combining the use of NMES and BFR appears to enhance the effects of both methods on protein metabolism and muscle hypertrophy [38,39,40].
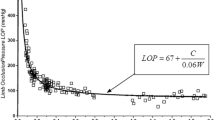
Regarding active BFR training, Hughes et al. (2017) demonstrated in patients with ACL‑R, gonarthrosis, and sarcopenia that BFR training produced higher strength gains than load-matched strength training without BFR but was less effective than high-load strength training [41]. However, due to the increased patient acceptance of BFR training, it can be used as a helpful surrogate on a transitional basis. The same author showed in a later randomized controlled trial that 8 weeks of BFR training produced similar hypertrophy and strength effects compared to high-load strength training (70% 1 RM) after ACL‑R, with BFR training showing higher scores in subjective knee function as well as being associated with less pain and swelling [42]. In a similar controlled study, Ohta et al. (2003) even demonstrated superior effects of 16 weeks of BFR training on muscle strength and muscle mass after ACL‑R [43]. In contrast, Curran et al. (2020) failed to show additional hypertrophy and strength gains of an 8‑week BFR intervention after ACL‑R when BFR training was applied in combination with high mechanical loads (70% 1 RM) compared to high mechanical load strength training without BFR [40]. Accordingly, useful effects of BFR training seem to be presented only in combination with low mechanical loads (20 to 40% 1 RM) [8]. This can be explained by the fact that high-load stimuli (> 60% 1 RM) per se induce high mechanical pressures in the muscle, which already trigger partial vascular occlusion, so that no additive training effect can be expected from the BFR intervention [44]. However, it remains to be stated that on the basis of the sparse and in part very heterogeneous data available, no valid statement can currently be made regarding exercise characteristics (such as training volumes, mechanical load, occlusion pressure) of BFR training for use in medical training therapy. For this reason, only load criteria from existing studies on healthy subjects can be derived for clinical practice to date (Fig. 2).
Another field of application for BFR interventions is prehabilitation. The aim of prehabilitation is to optimize the strength and performance level of the patient/affected limb prior to surgical interventions in terms of a “better-in, better-out” strategy [45]. For this purpose, Zargi et al. (2018) performed five preoperative BFR sessions for the knee extensors compared to placebo (sham) loading before ACL‑R and were able to show improved strength endurance and neuromuscular activation of the quadriceps muscle by BFR training 4 weeks postoperatively [46]. However, clinically relevant effects on preservation of muscle mass or strength could not be demonstrated, which is in line with results of previous investigations [24]. In a similar approach, Tramer et al. (2022) also failed to show superior strength effects of a 2-week BFR prehabilitation before ACL‑R compared to standard training [47]. In contrast, Franz et al. (2022) showed that 6 weeks of preoperative BFR training prior to total knee arthroplasty revealed superior postoperative outcomes in terms of muscle mass, muscle strength, and subjective knee function compared to sham loading or current standard care without prehabilitation [45].
In summary, these results show that BFR training can attenuate immobilization-related atrophy processes on the one hand and is able to induce comparable hypertrophy and strength effects in the postoperative course compared to high-load strength training on the other. In addition, BFR training causes comparatively less pain and swelling and is associated with a higher therapeutic acceptance. Thus, it can be assumed that BFR training can be optimally applied in cases of limited joint function before higher mechanical loads can be tolerated. Nevertheless, a heterogeneous data base is currently evident, which needs to be addressed in the future to enable valid recommendations for clinical practice (Fig. 3).
Regarding the effectiveness of prehabilitation with BFR, differences in the applied exercise designs and investigated patient populations as well as the limited evidence available make a conclusive evaluation difficult [28]. Therefore, further prospective studies for different injury entities and populations are needed. In addition, future research approaches should investigate the exact dose–response relationships of BFR training in order to define empirically validated loading normative valuess for optimal clinical treatment in the pre- and postoperative phases. Furthermore, long-term outcomes of rehabilitative BFR applications are lacking, including larger sample sizes, robust methodology, and homogeneous outcome variables.
Clinical blood flow restriction training II: impact on regenerated and graft tissue
Ligament reconstruction, meniscus repair or suture, and cartilage regenerative procedures are among the surgical procedures on the knee joint that require prolonged periods of (partial) bodyweight unloading during postoperative care. The duration of unloading varies by surgical procedure. Depending on the type and extent of (ligament) reconstruction, meniscal or cartilage damage, and the selected therapy (including Pridie drilling, minced cartilage defect filling, autologous chondrocyte implantation, or osteochondral grafting), gradual or complete unloading periods of up to 8 weeks are necessary [48,49,50]. These rehabilitative phases after joint surgery intensify the surgery-related consequences of the procedure, such as mobility restrictions, arthrogenic muscle inhibition, or loss of strength of the quadriceps and other muscle groups. In this regard, BFR training offers the potential to mitigate these joint-specific and muscular consequences, and thus most studies on BFR use after ACL reconstruction, cartilage regenerative surgery, or meniscal refixation/suture have focused on clinical and functional treatment outcomes [51,52,53]. However, whether BFR training also has direct positive or negative effects on the affected operated/reconstructed tissues, e.g., cartilage regenerate, has not been sufficiently investigated to date [54,55,56]. In this respect, the effects of temporary hypoxia phases on glucose and nitrogen metabolism, vascular adaptation and mitochondrial function, hormone regulation, protein and collagen synthesis, and the associated systemic and local effects have been at least fundamentally described [57,58,59]. Therefore, a possible influence of the BFR technique on operated tissues away from skeletal muscle can be hypothesized in theory.
While elevations in circulating growth hormones induced by BFR training are under debate as a contributor to muscle hypertrophy, in theory these hormonal responses could have a beneficial influence on protein and collagen synthesis of osteochondral or meniscoid tissue [60]. In principle, hGH and the growth factors regulated by them, such as IGF-I, vascular endothelial growth factor (VEGF), or transforming growth factor‑β (TGF-β), are assumed to have an important role in cartilage and bone healing, especially in the differentiation of chondrocytes, fibroblasts, and myoblasts, as well as in collagen synthesis [61,62,63]. In particular, the hypoxia-induced transcription factor hypoxia-inducible factor 1 alpha (HIF 1α) and its regulation by IGF may play an essential role in chondrocyte synthesis and activity [64]. Therefore, it is assumable that both the catabolic processes in articular cartilage of osteoarthritis patients and the healing of cartilage regenerate may be positively influenced by increased transcription of HIF 1α [65, 66]. Other growth factors such as TGF‑β, fibroblast growth factor (FGF), platelet-derived growth factor (PDGF), and bone morphogenetic protein (BMP) have been investigated in vitro and in animal models with regard to their effect on protein and collagen synthesis as well as on cartilage and bone healing [67,68,69], and can also be influenced by hypoxia. Considering this, it seems reasonable to propose that BFR-induced tissue hypoxia influences the HIF system and thus the cellular response to oxygen availability, in particular collagen synthesis [70, 71].
Formation of collagen is essential in cartilage and meniscus therapy as well as for the ligamentization processes after ligament reconstruction. The described processes of BFR-induced hypoxia offer the potential to promote collagen synthesis; however, the exact mechanisms of action and clinical implications require further investigation. In conclusion, BFR-induced hypoxia offers an interesting treatment option which should be further investigated in future studies to evaluate its many supporting effects on tissue healing and postoperative tissue regeneration after ligament reconstruction and cartilage or meniscus therapy.
Risks and side effects of blood flow restriction training
Due to the described physiological changes in the extremities under hypoxia, BFR training provides an extraordinary stress stimulus to the organism at a local and a systemic level. Regarding adverse events and side effects, scientific surveys among regular BFR users revealed symptoms such as temporary tingling paresthesia and hypesthesia, petechial hemorrhages in the subcutis, delayed-onset muscle soreness, and presyncopal cardiovascular dysregulation [72, 73]. These side effects exemplify the fact that BFR training represents a physiological stimulus, the local and systemic impacts of which and resulting risks must be considered during its application.
The BFR-induced venous occlusion during exercise not only provides an accumulation of metabolites in the ligated limb, but it also causes significant hypertension of the capacitance vessels. Invasive catheterization of the arterial and venous vessels of the upper extremities during BFR training revealed that both vascular compartments experience a significant increase in intravascular pressure compared to exercise conditions without venous occlusion (free flow) [74]. While the arterial system is accustomed to short- and long-term hypertensive states, this condition could cause long-term damage in the muscle-weak venous system.
It is well known from surgical disciplines that use of tourniquets leads to an increase in the risk of venous thrombosis [75]. In contrast, during physical exercise under free-flow conditions, coagulation homeostasis stays constant, with a rise in thrombotic and fibrinolytic potential [76]. In the context of BFR training, research has revealed that exercise under venous occlusion results in a significant increase in tissue plasminogen activator (tPA) compared to control exercise conditions [77]. This serine protease converts plasminogen to plasmin by proteolysis and thus acts as an endogenous activator of fibrinolysis. Enhanced release from the endothelium could be demonstrated after BFR exercise in young as well as in older subject populations [78]. With consideration of work from rehabilitative clinical research, recent meta-analyses and systematic reviews postulate a fibrinolytic rather than a thrombotic effect of BFR training on the coagulation cascade [79].
In addition to these local changes due to the applied pressure, BFR training also provides adaptation at the systemic level. During exercise, the applied cuff provides restriction of venous return from the limb. To maintain cardiac output, arterial blood pressure is successively increased and the heart rate is elevated [80]. Especially with bilateral application of the BFR technique, orthostatic dysregulation may occur with higher exercise intensities and/or changes in position. Further stress on the cardiovascular system occurs at the moment of opening the cuffs, when the stagnant venous blood regains access to the circulatory system. During this process, the increased preload that occurs is also compensated for by a further rise in heart rate. Additionally, it is unknown to what extent the altered electrolyte ratios of the BFR-exercised limb in the reperfusion phase have an additional influence on the function of the cardiovascular system. Therefore, from a physiological point of view, it remains to be stated that in bilateral application of BFR, opening of the cuffs should occur sequentially and with a time interval.
Although the described effects represent a range of adverse effects to be derived from BFR training, the mechanical application of the technique and occlusion pressure measurement alone may also have a negative impact. In cases of iatrogenic changes in the extremity vessels (including bypasses, stent implantations), cuff application with short-term vessel occlusion can potentially lead to serious consequences. For this reason, comprehensive medical history taking with consideration of systemic (e.g., cardiovascular illnesses) and local (e.g., vascular surgeries) previous findings and/or the condition after surgical intervention is necessary before BFR exposure in the individual subject.
Blood flow restriction in orthopedic pre- and rehabilitation: research desiderata
While BFR training has shown significant effects on muscular adaptation such as hypertrophy and strength development in numerous sports science studies, the effects on pre- and rehabilitation of musculature and tissue regeneration after surgical interventions are still largely unknown. However, based on the described characteristics and effects of BFR training, a far-reaching impact of the training method on rehabilitation can be assumed. For evidence-based application of the technique in the clinical setting, further data from larger patient populations need to be collected and important open questions must be addressed.
While some theories already exist regarding the underlying mechanisms of BFR training, future scientific approaches to the clinical care of patients should attempt to incorporate these theories into their investigation battery and thus collect more data from the clinical setting. It is important to note that the pathology and the surgical intervention cause changes in the physiological processes of muscles and/or regenerative tissues, which also need to be characterized in order to comprehensively describe the influence of the BFR technique (e.g., how does the muscular recruitment pattern change before and after surgery and to what extent does a BFR load cause a change compared to a control group). Furthermore, it has to be evaluated to what extent the surgical intervention changes the cardiovascular exercise capacity and coagulation homeostasis of a patient, potentially altering the risk profile of the BFR technique. This includes questions about the exact time at which a BFR technique should be implemented in the rehabilitative process and under which anamnestic/clinical findings BFR training should still be contraindicated.
Furthermore, it is questionable which technique (e.g., pBFR, active BFR training) should be applied at what time in the pre- and postoperative therapeutic process. For this reason, future studies should investigate, based on existing protocols (e.g., duration of an intervention, intensity of the load), at which dose–response relationship a BFR intervention should be applied before and after a joint-preserving surgical intervention. In order to allow studies with larger numbers of subjects, study protocols should also be kept lean to allow for integration of scientific work into the clinical treatment process.
Another promising topic of BFR training in the clinical therapy of ligament reconstruction, cartilage regenerative procedures, or osteosynthesis is its effect on the individual tissue types. Following the effects of hypoxic conditions in cell culture on various tissues, there could also be an influence of BFR after tissue injuries or surgical procedures. To investigate this topic, future research should focus on close cooperation between cellular research in vitro and therapeutic application in vivo. While laboratory work is able to demonstrate underlying effects of BFR exposure in bone, cartilage, and tendon tissue, indirect (e.g., analyses from peripheral blood, synovial fluid) or direct (e.g., T2* measurements of regenerated cartilage) studies in patients could support the raised hypotheses. It remains to be stated that the BFR training technique represents a new, hopeful therapeutic alternative to counteract pathology- or surgery-induced muscle atrophy and strength losses. However, to what extent and with which timing and/or dose this training technique offers benefits or even poses risks cannot be conclusively determined based on the existing literature. Based on the scientific evidence to date, there is a lack of comprehensive guidelines for integrating the technique into current clinical work. The BFR technique probably offers a high potential in the conservative pre- and postoperative treatment pertaining to joint-preserving interventions, with a still unknown influence on the injured or reconstructed tissues.
References
Perera E, Zhu XM, Horner NS et al (2022) Effects of blood flow restriction therapy for muscular strength, hypertrophy, and endurance in healthy and special populations: a systematic review and meta-analysis. Clin J Sport Med 32(5):531–545. https://doi.org/10.1097/JSM.0000000000000991
Hwang PS, Willoughby DS (2019) Mechanisms behind blood flow-restricted training and its effect toward muscle growth. J Strength Cond Res 33(1):S167–S179
Drummond MJ, Fujita S, Abe T et al (2008) Human muscle gene expression following resistance exercise and blood flow restriction. Med Sci Sports Exerc 40(4):691–698
Wernbom M, Apro W, Paulsen G et al (2013) Acute low-load resistance exercise with and without blood flow restriction increased protein signalling and number of satellite cells in human skeletal muscle. Eur J Appl Physiol 113(12):2953–2965
Takarada Y, Nakamura Y, Aruga S et al (2000) Rapid increase in plasma growth hormone after low-intensity resistance exercise with vascular occlusion. J Appl Physiol (1985) 88(1):61–65
Goto K, Ishii N, Kizuka T et al (2005) The impact of metabolic stress on hormonal responses and muscular adaptations. Med Sci Sports Exerc 37(6):955–963
Schoenfeld BJ (2013) Potential mechanisms for a role of metabolic stress in hypertrophic adaptations to resistance training. Sports Med 43(3):179–194
West DWD, Burd NA, Tang JE et al (2010) Elevations in ostensibly anabolic hormones with resistance exercise enhance neither training-induced muscle hypertrophy nor strength of the elbow flexors. J Appl Physiol (1985) 108(1):60–67. https://doi.org/10.1152/japplphysiol.01147.2009
West DWD, Kujbida GW, Moore DR et al (2009) Resistance exercise-induced increases in putative anabolic hormones do not enhance muscle protein synthesis or intracellular signalling in young men. J Physiol 587(21):5239–5247. https://doi.org/10.1113/jphysiol.2009.177220
West DWD, Phillips SM (2012) Associations of exercise-induced hormone profiles and gains in strength and hypertrophy in a large cohort after weight training. Eur J Appl Physiol 112(7):2693–2702. https://doi.org/10.1007/s00421-011-2246-z
Behringer M, Heinke L, Leyendecker J et al (2018) Effects of blood flow restriction during moderate-intensity eccentric knee extensions. J Physiol Sci 68(5):589–599. https://doi.org/10.1007/s12576-017-0568-2
Kawada S, Ishii N (2005) Skeletal muscle hypertrophy after chronic restriction of venous blood flow in rats. Med Sci Sports Exerc 37(7):1144–1150
Takano H, Morita T, Iida H et al (2005) Hemodynamic and hormonal responses to a short-term low-intensity resistance exercise with the reduction of muscle blood flow. Eur J Appl Physiol 95(1):65–73. https://doi.org/10.1007/s00421-005-1389-1
Fujita S, Abe T, Drummond MJ et al (2007) Blood flow restriction during low-intensity resistance exercise increases S6K1 phosphorylation and muscle protein synthesis. J Appl Physiol (1985) 103(3):903–910. https://doi.org/10.1152/japplphysiol.00195.2007
Yinghao L, Jing Y, Yongqi W et al (2021) Effects of a blood flow restriction exercise under different pressures on testosterone, growth hormone, and insulin-like growth factor levels. J Int Med Res 49(9):3000605211039564
Heckman CJ, Enoka RM (2012) Motor unit. Compr Physiol 2(4):2629–2682
Henneman E (1957) Relation between size of neurons and their susceptibility to discharge. Science 126(3287):1345–1347
Fatela P, Mendonca GV, Veloso AP et al (2019) Blood flow restriction alters motor unit behavior during resistance exercise. Int J Sports Med 40(9):555–562. https://doi.org/10.1055/a-0888-8816
Suga T, Okita K, Morita N et al (2009) Intramuscular metabolism during low-intensity resistance exercise with blood flow restriction. J Appl Physiol (1985) 106(4):1119–1124. https://doi.org/10.1152/japplphysiol.90368.2008
Ohno Y, Ando K, Ito T et al (2019) Lactate stimulates a potential for hypertrophy and regeneration of mouse skeletal muscle. Nutrients. https://doi.org/10.3390/nu11040869
Shirai T, Kitaoka Y, Uemichi K et al (2022) Effects of lactate administration on hypertrophy and mTOR signaling activation in mouse skeletal muscle. Physiol Rep 10(16):e15436
Gao Y, Arfat Y, Wang H et al (2018) Muscle atrophy induced by mechanical unloading: mechanisms and potential countermeasures. Front Physiol 9:235. https://doi.org/10.3389/fphys.2018.00235
Thomas AC, Wojtys EM, Brandon C et al (2016) Muscle atrophy contributes to quadriceps weakness after anterior cruciate ligament reconstruction. J Sci Med Sport 19(1):7–11. https://doi.org/10.1016/j.jsams.2014.12.009
Palmieri-Smith RM, Lepley LK (2015) Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med 43(7):1662–1669. https://doi.org/10.1177/0363546515578252
Schmitt LC, Paterno MV, Hewett TE (2012) The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 42(9):750–759. https://doi.org/10.2519/jospt.2012.4194
Schoenfeld BJ, Grgic J, Van Every DW et al (2021) Loading recommendations for muscle strength, hypertrophy, and local endurance: a re-examination of the repetition continuum. Sports (Basel). https://doi.org/10.3390/sports9020032
Buckthorpe M, La Rosa G, Villa DF (2019) Restoring knee extensor strength after anterior cruciate ligament reconstruction: a clinical commentary. Intl J Sports Phys Ther 14(1):159–172
Wengle L, Migliorini F, Leroux T et al (2022) The effects of blood flow restriction in patients undergoing knee surgery: a systematic review and meta-analysis. Am J Sports Med 50(10):2824–2833. https://doi.org/10.1177/03635465211027296
Grønfeldt BM, Lindberg Nielsen J, Mieritz RM et al (2020) Effect of blood-flow restricted vs heavy-load strength training on muscle strength: systematic review and meta-analysis. Scand J Med Sci Sports 30(5):837–848. https://doi.org/10.1111/sms.13632
Lixandrão ME, Ugrinowitsch C, Berton R et al (2018) Magnitude of muscle strength and mass adaptations between high-load resistance training versus low-load resistance training associated with blood-flow restriction: a systematic review and meta-analysis. Sports Med 48(2):361–378
Pignanelli C, Christiansen D, Burr JF (2021) Blood flow restriction training and the high-performance athlete: science to application. J Appl Physiol (1985) 130(4):1163–1170. https://doi.org/10.1152/japplphysiol.00982.2020
Scott BR, Loenneke JP, Slattery KM et al (2016) Blood flow restricted exercise for athletes: a review of available evidence. J Sci Med Sport 19(5):360–367. https://doi.org/10.1016/j.jsams.2015.04.014
Patterson SD, Hughes L, Warmington S et al (2019) Blood flow restriction exercise: considerations of methodology, application, and safety. Front Physiol 10:533. https://doi.org/10.3389/fphys.2019.00533
Kubota A, Sakuraba K, Sawaki K et al (2008) Prevention of disuse muscular weakness by restriction of blood flow. Med Sci Sports Exerc 40(3):529–534
Takarada Y, Takazawa H, Ishii N (2000) Applications of vascular occlusion diminish disuse atrophy of knee extensor muscles. Med Sci Sports Exerc 32(12):2035–2039
Iversen E, Røstad V, Larmo A (2016) Intermittent blood flow restriction does not reduce atrophy following anterior cruciate ligament reconstruction. J Sport Health Sci 5(1):115–118. https://doi.org/10.1016/j.jshs.2014.12.005
Labanca L, Bonsanto F, Raffa D et al (2022) Does adding neuromuscular electrical stimulation to rehabilitation following total knee arthroplasty lead to a better quadriceps muscle strength recovery? A systematic review. Int J Rehabil Res 45(2):118–125. https://doi.org/10.1097/MRR.0000000000000525
Strasser EM, Stättner S, Karner J et al (2009) Neuromuscular electrical stimulation reduces skeletal muscle protein degradation and stimulates insulin-like growth factors in an age- and current-dependent manner: a randomized, controlled clinical trial in major abdominal surgical patients. Ann Surg 249(5):738–743
Santiago-Pescador S, Fajardo-Blanco D, López-Ortiz S et al (2022) Acute effects of electrostimulation and blood flow restriction on muscle thickness and fatigue in the lower body. Eur J Sport Sci. https://doi.org/10.1080/17461391.2022.2113145
Natsume T, Yoshihara T, Naito H (2019) Electromyostimulation with blood flow restriction enhances activation of mTOR and MAPK signaling pathways in rat gastrocnemius muscles. Appl Physiol Nutr Metab 44(6):637–644. https://doi.org/10.1139/apnm-2018-0384
Hughes L, Paton B, Rosenblatt B et al (2017) Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br J Sports Med 51(13):1003–1011. https://doi.org/10.1136/bjsports-2016-097071
Hughes L, Rosenblatt B, Haddad F et al (2019) Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK national health service randomised controlled trial. Sports Med 49(11):1787–1805
Ohta H, Kurosawa H, Ikeda H et al (2003) Low-load resistance muscular training with moderate restriction of blood flow after anterior cruciate ligament reconstruction. Acta Orthop Scand 74(1):62–68
Laurentino G, Ugrinowitsch C, Aihara AY et al (2008) Effects of strength training and vascular occlusion. Int J Sports Med 29(8):664–667. https://doi.org/10.1055/s-2007-989405
Franz A, Ji S, Bittersohl B et al (2022) Impact of a six-week prehabilitation with blood-flow restriction training on pre- and postoperative skeletal muscle mass and strength in patients receiving primary total knee arthroplasty. Front Physiol 13:881484. https://doi.org/10.3389/fphys.2022.881484
Žargi T, Drobnič M, Stražar K et al (2018) Short-term preconditioning with blood flow restricted exercise preserves quadriceps muscle endurance in patients after anterior cruciate ligament reconstruction. Front Physiol 9:1150. https://doi.org/10.3389/fphys.2018.01150
Tramer JS, Khalil LS, Jildeh TR et al (2023) Blood flow restriction therapy for 2 weeks prior to anterior cruciate ligament reconstruction did not impact quadriceps strength compared to standard therapy. Arthroscopy 39(2):373–381. https://doi.org/10.1016/j.arthro.2022.06.027
Calanna F, Duthon V, Menetrey J (2022) Rehabilitation and return to sports after isolated meniscal repairs: a new evidence-based protocol. J Exp Orthop 9(1):80. https://doi.org/10.1186/s40634-022-00521-8
Jakobsen TL, Thorborg K, Fisker J et al (2022) Blood flow restriction added to usual care exercise in patients with early weight bearing restrictions after cartilage or meniscus repair in the knee joint: a feasibility study. J Exp Orthop 9(1):101. https://doi.org/10.1186/s40634-022-00533-4
Faber S, Niemeyer P, Fickert S (2021) Knorpelersatzverfahren und Regeneration am Knie- und Hüftgelenk. Orthopädie Unfallchirurgie up2date 16(04):335–356
Culvenor AG, Girdwood MA, Juhl CB et al (2022) Rehabilitation after anterior cruciate ligament and meniscal injuries: a best-evidence synthesis of systematic reviews for the OPTIKNEE consensus. Br J Sports Med 56(24):1445–1453. https://doi.org/10.1136/bjsports-2022-105495
Mason JS, Crowell MS, Brindle RA et al (2022) The effect of blood flow restriction training on muscle atrophy following meniscal repair or chondral restoration surgery in active duty military: a randomized controlled trial. J Sport Rehabil 31(1):77–84. https://doi.org/10.1123/jsr.2020-0518
Noyes FR, Barber-Westin SD, Sipes L (2021) Blood flow restriction training can improve peak torque strength in chronic atrophic postoperative quadriceps and hamstrings muscles. Arthroscopy 37(9):2860–2869. https://doi.org/10.1016/j.arthro.2021.03.040
Koc BB, Truyens A, Heymans MJLF et al (2022) Effect of low-load blood flow restriction training after anterior cruciate ligament reconstruction: a systematic review. Intl J Sports Phys Ther 17(3):334–346. https://doi.org/10.26603/001c.33151
Colapietro M, Portnoff B, Miller SJ et al (2022) Effects of blood flow restriction training on clinical outcomes for patients with ACL reconstruction: a systematic review. Sports Health. https://doi.org/10.1177/19417381211070834
Telfer S, Calhoun J, Bigham JJ et al (2021) Biomechanical effects of blood flow restriction training after ACL reconstruction. Med Sci Sports Exerc 53(1):115–123
Saatmann N, Zaharia O‑P, Loenneke JP et al (2021) Effects of blood flow restriction exercise and possible applications in type 2 diabetes. Trends Endocrinol Metab 32(2):106–117
Volga Fernandes R, Tricoli V, Garcia Soares A et al (2022) Low-load resistance exercise with blood flow restriction increases hypoxia-induced angiogenic genes expression. J Hum Kinet 84:82–91. https://doi.org/10.2478/hukin-2022-0101
Li S, Li S, Wang L et al (2022) The effect of blood flow restriction exercise on angiogenesis-related factors in skeletal muscle among healthy adults: a systematic review and meta-analysis. Front Physiol 13:814965. https://doi.org/10.3389/fphys.2022.814965
Doessing S, Heinemeier KM, Holm L et al (2010) Growth hormone stimulates the collagen synthesis in human tendon and skeletal muscle without affecting myofibrillar protein synthesis. J Physiol 588(2):341–351. https://doi.org/10.1113/jphysiol.2009.179325
Fortier LA, Lust G, Mohammed HO et al (1999) Coordinate upregulation of cartilage matrix synthesis in fibrin cultures supplemented with exogenous insulin-like growth factor‑I. J Orthop Res 17(4):467–474
Strong DD, Beachler AL, Wergedal JE et al (1991) Insulinlike growth factor II and transforming growth factor beta regulate collagen expression in human osteoblastlike cells in vitro. J Bone Miner Res 6(1):15–23
Schmidmaier G, Wildemann B, Bail H et al (2000) Die lokale Freisetzung von IGF‑I und TGF-beta 1 aus einer biodegradierbaren Poly(D,L-Lactid) Beschichtung von Implantaten beschleunigt die Frakturheilung. Chirurg 71(9):1016–1022
Sartori-Cintra AR, de Mara CS, Argolo DL et al (2012) Regulation of hypoxia-inducible factor-1α (HIF-1α) expression by interleukin-1β (IL‑1 β), insulin-like growth factors I (IGF-I) and II (IGF-II) in human osteoarthritic chondrocytes. Clinics (Sao Paulo) 67(1):35–40
Bobes Álvarez C, Issa-Khozouz Santamaría P, Fernández-Matías R et al (2020) Comparison of blood flow restriction training versus non-occlusive training in patients with anterior cruciate ligament reconstruction or knee osteoarthritis: a systematic review. J Clin Med. https://doi.org/10.3390/jcm10010068
Chen Y, Wang J, Li S et al (2022) Acute effects of low load resistance training with blood flow restriction on serum growth hormone, insulin-like growth factor‑1, and testosterone in patients with mild to moderate unilateral knee osteoarthritis. Heliyon 8(10):e11051. https://doi.org/10.1016/j.heliyon.2022.e11051
Berven S, Tay BK, Kleinstueck FS et al (2001) Clinical applications of bone graft substitutes in spine surgery: consideration of mineralized and demineralized preparations and growth factor supplementation. Eur Spine J 10(2):S169–77
Herrera Millar VR, Mangiavini L, Polito U et al (2021) Hypoxia as a stimulus for the maturation of meniscal cells: highway to novel tissue engineering strategies? Int J Mol Sci. https://doi.org/10.3390/ijms22136905
Shi S, Mercer S, Eckert GJ et al (2009) Growth factor regulation of growth factors in articular chondrocytes. J Biol Chem 284(11):6697–6704. https://doi.org/10.1074/jbc.M807859200
Gustafsson T, Puntschart A, Kaijser L et al (1999) Exercise-induced expression of angiogenesis-related transcription and growth factors in human skeletal muscle. Am J Physiol 276(2):H679–85
Hurst JH (2016) William Kaelin, Peter Ratcliffe, and Gregg Semenza receive the 2016 Albert Lasker Basic Medical Research Award. J Clin Invest 126(10):3628–3638. https://doi.org/10.1172/JCI90055
Patterson SD, Brandner CR (2018) The role of blood flow restriction training for applied practitioners: a questionnaire-based survey. J Sports Sci 36(2):123–130. https://doi.org/10.1080/02640414.2017.1284341
de Queiros VS, Dantas M, Neto GR et al (2021) Application and side effects of blood flow restriction technique: a cross-sectional questionnaire survey of professionals. Medicine 100(18):e25794
Franz A, Berndt F, Raabe J et al (2020) Invasive assessment of hemodynamic, metabolic and ionic consequences during blood flow restriction training. Front Physiol 11:617668. https://doi.org/10.3389/fphys.2020.617668
Mori N, Kimura S, Onodera T et al (2016) Use of a pneumatic tourniquet in total knee arthroplasty increases the risk of distal deep vein thrombosis: a prospective, randomized study. Knee 23(5):887–889. https://doi.org/10.1016/j.knee.2016.02.007
Nakajima T, Takano H, Kurano M et al (2007) Effects of KAATSU training on haemostasis in healthy subjects. Int J KAATSU Ttaining Res 3(1):11–20
Clark BC, Manini TM, Hoffman RL et al (2011) Relative safety of 4 weeks of blood flow-restricted resistance exercise in young, healthy adults. Scand J Med Sci Sports 21(5):653–662. https://doi.org/10.1111/j.1600-0838.2010.01100.x
Fry CS, Glynn EL, Drummond MJ et al (2010) Blood flow restriction exercise stimulates mTORC1 signaling and muscle protein synthesis in older men. J Appl Physiol (1985) 108(5):1199–1209. https://doi.org/10.1152/japplphysiol.01266.2009
Loenneke JP, Wilson JM, Wilson GJ et al (2011) Potential safety issues with blood flow restriction training. Scand J Med Sci Sports 21(4):510–518. https://doi.org/10.1111/j.1600-0838.2010.01290.x
Spranger MD, Krishnan AC, Levy PD et al (2015) Blood flow restriction training and the exercise pressor reflex: a call for concern. Am J Physiol Heart Circ Physiol 309(9):H1440–52. https://doi.org/10.1152/ajpheart.00208.2015
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Franz, A. Praetorius, C. Raeder, A. Hirschmüller, and M. Behringer declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information

Scan QR code & read article online
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Franz, A., Praetorius, A., Raeder, C. et al. Blood flow restriction training in the pre- and postoperative phases of joint surgery. Arthroskopie 36, 252–260 (2023). https://doi.org/10.1007/s00142-023-00615-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00142-023-00615-0