Abstract
Purpose
Severe Pneumocystis jirovecii pneumonia (PJP) requiring intensive care has been the subject of few prospective studies. It is unclear whether delayed curative antibiotic therapy may impact survival in these severe forms of PJP. The impact of corticosteroid therapy combined with antibiotics is also unclear.
Methods
This multicentre, prospective observational study involving 49 adult intensive care units (ICUs) in France was designed to evaluate the severity, the clinical spectrum, and outcomes of patients with severe PJP, and to assess the association between delayed curative antibiotic treatment and adjunctive corticosteroid therapy with mortality.
Results
We included 158 patients with PJP from September 2020 to August 2022. Their main reason for admission was acute respiratory failure (n = 150, 94.9%). 12% of them received antibiotic prophylaxis for PJP before ICU admission. The ICU, hospital, and 6-month mortality were 31.6%, 35.4%, and 40.5%, respectively. Using time-to-event analysis with a propensity score-based inverse probability of treatment weighting, the initiation of curative antibiotic treatment after 96 h of ICU admission was associated with faster occurrence of death [time ratio: 6.75; 95% confidence interval (95% CI): 1.48–30.82; P = 0.014]. The use of corticosteroids for PJP was associated with faster occurrence of death (time ratio: 2.48; 95% CI 1.01–6.08; P = 0.048).
Conclusion
This study showed that few patients with PJP admitted to intensive care received prophylactic antibiotic therapy, that delay in curative antibiotic treatment was common and that both delay in curative antibiotic treatment and adjunctive corticosteroids for PJP were associated with accelerated mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hospital and 6-month mortality of patients with Pneumocystis jirovecii pneumonia admitted to the intensive care unit is high, especially among patients not infected by human immunodeficiency virus, with delays in treatment linked to poorer survival. |
Lack of antibiotic prophylaxis in immunocompromised patients is notable, and adjunctive corticosteroid therapy may adversely affect outcomes. |
Introduction
Pneumocystis jirovecii pneumonia (PJP) is an opportunistic infection affecting immunocompromised patients, and its incidence has risen in recent decades [1,2,3,4]. It now affects more patients not infected by human immunodeficiency virus (HIV) than HIV patients [5, 6]. PJP is potentially severe and is linked to a hospital mortality of about 5–15% in patients with HIV infection [7, 8]. Mortality escalates significantly beyond 50% when affecting patients with cancer, haematologic malignancy, pre-existing heart or respiratory failure, or is associated with the acute respiratory distress syndrome (ARDS) or septic shock requiring admission to intensive care [7, 9,10,11,12,13,14].
Evidence from the past 15 years indicates that patients with autoimmune rheumatic or vascular inflammatory diseases, among others, are increasingly susceptible due to immunosuppressive treatments [11, 15]. Within this specific population, antibiotic prophylaxis demonstrates divergent practices without a unified consensus [3, 16,17,18,19,20,21,22,23]. In immunocompromised individuals, PJP should be suspected in cases of diffuse pneumonia, with or without respiratory distress [24,25,26]. However, studies have underscored delays in initiating treatment among a subset of these patients during the initial hospitalization, potentially impacting in-hospital survival rates [11, 13, 27,28,29].
While corticosteroid therapy for PJP with hypoxemia in HIV patients has shown efficacy [30], uncertainties persist regarding its benefits in non-HIV patients [31,32,33,34,35].
There is a paucity of studies specifically dedicated to patients admitted to the intensive care unit (ICU) with PJP, leading to imprecise estimates of hospital mortality, long-term outcomes, and required supportive care for patients with the most severe forms of PJP.
In this context, we initiated a multicentre prospective observational study to describe ICU admission conditions for PJP patients, their clinical presentation, estimate the prevalence of prophylaxis, and finally, determine prevalence of delayed antibiotic treatment and corticosteroids use, and assess their association with 6-month mortality following ICU admission.
Methods
In January 2020, 100 French intensive care units (ICUs), all members of the French Intensive Care Society (SRLF) and/or the CRICS-TRIGGERSEP clinical research network (https://www.crics-triggersep.org/en), were invited to participate, of which 49 agreed. The study was conducted from September 1, 2020, to August 31, 2022. During this period, consecutive adult patients (≥ 18 years old) admitted to these ICUs with proven or probable PJP or diagnosed with PJP during ICU stay were prospectively included. Collected data included patient baseline clinical characteristics, type of immunocompromising disease, pre-ICU trajectory, reason for ICU admission, prophylaxis against PJP, diagnostic procedures for PJP, respiratory support, timing of curative antibiotic PJP treatment initiation, corticosteroids therapy for PJP, presence of lung co-infection, decisions of withholding or withdrawing therapy, and ICU, hospital, and 6-month mortality. The vital status at 6 months was obtained from hospital records or via direct contact with patients, their family, or their general practitioner, or by checking the national online database of deceased individuals at https://deces.matchid.io/about.
Patients and families received both verbal and written information about the study upon PJP identification, with the option to consent or decline participation. The study protocol received approval from the ethics committee of the French Intensive Care Society on May 20, 2020 (#CE SRLF 20–48).
Definitions
In this prospective study, investigators were asked to include only patients with proven or probable PJP based on specific biological tests and concordant clinical and radiologic presentations, as per the European definition [36, 37]. In every case, PJP diagnosis was retained after diagnostic workup had ruled out alternative plausible diagnoses. Cases where P. jirovecii was detected through non-quantitative polymerase chain reaction (PCR) in oral or lower respiratory tract samples, or via quantitative PCR with high cycle threshold values [38] (determined by the clinician’s judgment) and lacked corresponding clinical and radiological features, should not be included.
Investigators gathered data on prior or ongoing prophylaxis of PJP upon ICU admission or upon PJP diagnosis, through interviews with patients, family members, or their primary care providers. The prophylaxis included oral trimethoprim/sulfamethoxazole (TMP-SMX), atovaquone, dapsone, or aerosolized pentamidine, without specific differentiation in the data collection regarding the type of prophylaxis.
Data were gathered on the current or recent (within 4 weeks before ICU admission) use of immunosuppressive or immunomodulatory medications (including corticosteroid therapy) and the specific type of medication utilized. The criterion for defining corticosteroid-induced immunosuppression was established as a daily dosage of ≥ 15 mg of prednisone-equivalent for a period of ≥ 4 weeks, or the receipt of a bolus of ≥ 500 mg within the preceding 3 months.
Statistical analysis
The sample size was determined to assess the association of late treatment of PJP on patient mortality 6 months post-admission to the ICU. Given the available literature [11, 24, 28, 29], we opted to compare patients receiving the first dose of curative antibiotic treatment for PJP before or on the fourth day of ICU stay with those treated after the fourth day. Based on an anticipated 55% overall mortality rate at 6 months and a death hazard ratio of 2.4 for the late treatment cohort, a total of 103 patients were required with a type I alpha risk set at 5%, and a 90% statistical power.
To assess the association of late treatment of PJP with patient mortality, we excluded patients who had received curative treatment for PJP before ICU admission due to uncertainty regarding the exact time of PJP onset. We set time zero at the exact time of ICU admission. Since the variable “early/late curative treatment” violated the proportional hazards assumption, we used an accelerated failure time (AFT) model with a Weibull distribution [39] to estimate the time ratio, representing the relative change in the mean time to death associated with a given independent variable. We used stabilized propensity score-based inverse probability of treatment weighting (PS-IPW) [40] to estimate the average treatment effect (ATE). We adjusted our analysis (1) for established predictors of mortality in ICU patients, i.e., age, sex, Simplified Acute Physiology Score (SAPS II) [41], and Sequential Organ Failure Assessment (SOFA) score [42] on Day 1, and (2) for covariables that still were unbalanced between groups after weighing (imbalance was defined as a standardized difference > 0.1). The propensity score (PS), reflecting the likelihood of receiving curative PJP treatment after the fourth day in the ICU, was computed via multivariable logistic regression using all available baseline covariates upon ICU admission as independent variables (see electronic supplementary material [ESM] for details). We trimmed extreme PS values at the 2.5 and 97.5% percentiles [43].
The association of the use of corticosteroids with 6-month mortality was analyzed using the same approach but used the entire study population from which we excluded 2 patients who were enrolled in a multicentre, double-blind randomized trial comparing corticosteroids to placebo (ClinicalTrials.gov identifier: NCT02944045). Time zero was set at the time of first administration of curative antibiotic treatment for PJP. Whether patients were on corticosteroids before PJP onset was added to the list of covariables used for adjustment. A specific PS was calculated for estimating the probability of receiving corticosteroids during treatment of PJP. We classified patients in the corticosteroids group when they either received adjunctive corticosteroid therapy specifically for PJP as declared by investigators, or when they received corticosteroid therapy (≥ 40 mg/prednisone-equivalent) during at least the first week of treatment of PJP for other reasons.
We performed several exploratory subgroup analyses.
Continuous variables are summarized using median and interquartile range (IQR) (i.e., 25th and 75th percentiles). Groups were compared by Pearson χ2, Fisher, Kruskal–Wallis, or Mann–Whitney U tests as appropriate.
The analyses were conducted using R software version 4.1.3 (R Foundation for Statistical Computing). A two-tailed P value < 0.05 was considered significant. However, analyses were not adjusted for multiple testing.
Results
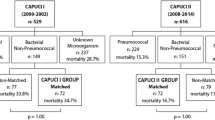
During the 2-year study period, 36 out of 49 participating ICUs (see their location on the French territory in Figure S1 of ESM) admitted a total of 158 patients with PJP. These patients had a mean age of 62 years (IQR 48–71), with 62% being male. Figure 1 provides an overview of the patient trajectory before ICU admission. The primary reason for ICU admission was acute respiratory failure, accounting for 150 (94.9%) patients. Table S1 of ESM summarizes other causes of ICU admission. Patients’ characteristics and outcomes are summarized in Table 1. One hundred and forty-five (91.8%) patients underwent lung high-resolution computed tomography (CT) scan within the first week of ICU stay. The various biological/clinical scenarios that led to PJP diagnosis are outlined in Fig. 1 and further details are provided in Table S2. Notably, upon data review, it was observed that 70 cases (44.3%) could not be definitively classified as proven or probable PJP. However, these cases had been classified as such by bedside clinicians, and thus, for the sake of thorough analysis, were retained in the dataset.
Flow chart. ARDS acute respiratory distress syndrome, ICU intensive care unit, IQR interquartile range, LOS length of stay, PCR polymerase chain reaction (either conventional i.e., not quantitative or quantitative), PJP Pneumocystis jirovecii pneumonia, qPCR quantitative PCR. ARDS was defined according to the Berlin definition [47]. aDiagnostic of PJP made by the pathologist using microscopy and specific staining (modified Toluidine Blue O, Grocott-Gomori methenamine silver, or Immunofluorescent-antibody staining). bIn every case, the diagnosis of PJP was based on a positive quantitative or non-quantitative PCR test performed on oral wash (%) or on lower respiratory tract sample, and serum (1–3)-b-d-glucan positivity (threshold for positivity left to the appreciation of the attending intensivist) [48], but also on the presence of bilateral interstitial pneumonia and a diagnostic workup that ruled out other diagnoses. cIn every case, the diagnosis of PJP was based on a positive quantitative PCR test with sufficiently low cycle threshold (Ct) (left to the appreciation of the attending intensivist), but also on the presence of bilateral interstitial pneumonia and a diagnostic workup that ruled out other diagnoses. dIn every case, the diagnosis of PJP was based on a positive non-quantitative PCR test performed on oral wash (%) or on lower respiratory tract sample, but also on the presence of either bilateral interstitial infiltrates on chest X-ray or bilateral ground glass opacities on high-resolution lung computed tomography and a diagnostic workup that ruled out other diagnoses. eAmong the 36 participating ICUs, 18 were in university affiliated hospitals. f13 ICUs, including 6 ICUs in university affiliated hospitals, did not admit any patient with PJP during the study period
Lung co-infections (bacterial, viral or fungal, either documented or only suspected, see Table 1) were common (69/158, 43.7%) during treatment of PJP.
Cause of immunosuppression
Upon ICU admission, 105 patients (66.5%) were on ongoing or recent immunosuppressive drug therapy, including corticosteroids. Of these, 66 patients (41.8%) were using more than one type of immunosuppressive drug, and 29 patients (18.4%) were on more than two. Immunosuppression was associated with various conditions: solid-organ cancer or haematologic malignancies in 66 (41.8%) patients (details are provided in Table S3 and S4), HIV infection in 29 (18.4%) patients, and solid-organ transplant in 14 (8.9%) patients. Among the remaining 49 (31%) patients, 36 (73.5%) presented diverse inflammatory/autoimmune diseases (details in Table S5), 7 (14.3%) were solely on corticosteroid therapy causing immunosuppression, and 6 (12.2%) had no identified cause of immunosuppression.
Prophylaxis
Nineteen patients out of 158 (12%) were prescribed and consistently adhered to prophylaxis for PJP before ICU admission. The proportion of patients under such prophylaxis varied notably among different causes of immunosuppression (Table 1).
Respiratory support
Ninety-three (58.9%) patients required invasive mechanical ventilation during ICU stay. Patients with HIV infection were less frequently mechanically ventilated than organ transplant receivers (P = 0.027) or patients with other immunocompromising conditions than solid-organ or haematologic neoplasms (P = 0.008) (Table 1). Acute respiratory distress syndrome occurred in 82 (88.2%) of patients who required invasive mechanical ventilation.
Mortality
Overall, the ICU, hospital, and 6-month mortality rates were 31.6%, 35.4%, and 40.5%, respectively (Table 1).
Mortality at 6 months was lower for patient with HIV infection (3/29, 10.3%) than for patients with malignancies (31/66, 47.0%) (P = 0.001), organ transplant recipients (9/14, 64.3%) (P = 0.0005) or other causes of immunosuppression (21/49, 2.9%) (P = 0.006).
Forty-six (29.1%) patients underwent treatment withholding or withdrawal, with the lowest incidence observed among those with HIV infection (Table 1) (see details in Table S6).
Timing of antibiotic treatment of PJP
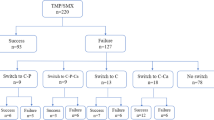
One patient had a documented allergy to TMP-SMX and received treatment with atovaquone. Among the remaining 157 patients initially treated with TMP-SMX, one patient was switched to pentamidine due to toxidermia, and another patient was switched to atovaquone due to bone marrow toxicity; both adverse events resolved subsequently without any lasting effects.
For the 112 patients whose curative treatment began in the ICU (while others started treatment on regular wards), initiation occurred at a median of 4 h (IQR 16–69) following ICU admission. Patients with immunosuppression classified as “other” (Table 1), mainly patients with autoimmune/inflammatory diseases (Table S5), had significantly delayed treatment initiation (23 h [IQR 6–85]) compared to those with solid-organ or hematologic malignancies (4 h [IQR 16–69]) (P = 0.040). All patients with HIV infection whose curative treatment commenced in the ICU (n = 21) were administered the first dose before the 96th hour. Decision of treatment withholding or withdrawing occurred in 8 (40%) patients treated late and in 22 (23.9%) patients treated earlier (P = 0.23). Terminal extubation occurred in two (10%) patients treated late and in eight (8.7%) patients treated earlier (P > 0.99). Lung co-infection was present during the first week of treatment of PJP for 10/20 (50%) patients treated late and for 42/92 (45.6%) patients treated earlier (P = 0.92).
Six-month mortality was 55% (11/20) for patients who started curative treatment late, and 30.4% (28/92) for patients treated earlier (P = 0.06 by χ2 test). Time-to-event analysis with PS-IPW revealed that initiating curative treatment late was linked to a time ratio of 6.75 (95% confidence interval [95% CI]: 1.48–30.82) (P = 0.014). This indicates that, on average, patients receiving late treatment had a 6.75 times faster occurrence of death (i.e., shorter survival) compared to those treated early. Results of the full AFT model are provided in Table S7. Weighted Kaplan–Meier survival curves are shown in Fig. 2. When restricted to the 91 patients without HIV infection, time-to-event analysis still showed an accelerated time to death in the late treatment group (time ratio = 6.24 [95% CI 1.39–28.00]; P = 0.017) (see Figure S2 detailing subgroup exploratory analyses). Patients classified as proven or probable cases (Table S2) had a 6-month mortality of 55.6% (5/9) when treated late and 28% (14/50) when treated earlier (P = 0.13). The other cases had a 6-month mortality of 55.5% (6/11) when treated late and 33.3% (14/42) when treated earlier.
Survival probability according to early or late (after the 96th hour of ICU) curative antibiotic treatment of PJP. The upper panel shows the weighted Kaplan–Meier curves for each group obtained by propensity score-based inverse probability of treatment weighting (PS-IPW, see “Methods” for details). In contrast, the risk table (lower panel) shows raw numbers at risk for each group (i.e., not in the weighted population constructed by PS-IPW for statistical analysis). The P value is the one obtained by accelerated failure time modeling (see “Methods”) for the comparison of late versus early treatment. Time zero was the time of ICU admission
Corticosteroid therapy
The proportion of patients who received corticosteroid therapy during their curative antibiotic treatment of PJP was 64.6% (102/158), with the highest proportion seen in patients with HIV infection (24/29 [82.8%]). In 71 (45.5%) cases, corticosteroids were given specifically for PJP (or for PJP but also other reason), as declared by investigators, at a median daily dose of 80 (IQR 60–95) mg prednisone-equivalent. When given exclusively for other reason (see details in Table S8), corticosteroids were administered at a median daily dose of 75 (IQR 50–131) mg prednisone-equivalent.
Decision of treatment withholding or withdrawing occurred in 32 (31.4%) patients treated with corticosteroids and in 14 (25.4%) not treated with corticosteroids (P = 0.60). Terminal extubation occurred in 10 (9.7%) patients of the corticosteroids group and in seven (12.7%) patients not receiving corticosteroids (P = 0.75). Lung co-infection was present during the first week of treatment of PJP for 46/102 (45.1%) and 23/54 (42.6%) patients of the corticosteroids and no corticosteroids groups, respectively (P = 0.90).
The 6-month mortality was not different between patients receiving or not receiving corticosteroids (40.2% [41/102] and 40.7% [22/54], respectively; P > 0.99]. Time-to-event analysis revealed that the use of corticosteroids during treatment of PJP was linked to a time ratio of 2.48 (95% CI 1.01–6.08) (P = 0.048), meaning that, on average, patients receiving corticosteroids had a 2.48 times faster occurrence of death compared to those not receiving corticosteroids. Results of the full AFT model are provided in Table S6. Weighted Kaplan–Meier survival curves are shown in Fig. 3. The use of corticosteroids was not associated with faster occurrence of death in the 29 patients with HIV infection (time ratio: 0.26 [95% CI 0.02–3.7], P = 0.32) but still showed a significant association in the 127 patients without HIV infection (time ratio: 2.56 [95% CI 1.03–6.39], P = 0.043) (see Figure S3 detailing subgroup exploratory analyses). Additionally, within the subgroup of patients classified as proven or probable PJP cases (as detailed in Table S2), the use of corticosteroids was significantly associated with faster occurrence of death (time ratio: 5.71 [95% CI 1.85–17.61], P = 0.003) (Figure S3).
Survival probability according to the use of adjunctive corticosteroid therapy for PJP in the whole study population (N = 158). The upper panel shows the weighted Kaplan–Meier curves for each group obtained by propensity score-based inverse probability of treatment weighting (PS-IPW, see “Methods” for details). In contrast, the risk table (lower panel) shows raw numbers at risk for each group (i.e., not in the weighted population constructed by PS-IPW for statistical analysis). The P value is the one obtained by accelerated failure time modeling (see “Methods”) for the comparison of use of adjunctive corticosteroid therapy versus no use. Time zero was the time at which curative antibiotic treatment for PJP was started. Patients were right censored at Day 180 after the beginning of curative treatment. Note that one patient of the no corticosteroids group could be followed up only until the 178th day
Discussion
The present study confirms that mortality associated with PJP is high, with severe PJP requiring ICU admission now primarily affecting non-HIV patients. Notably, a significant proportion (88%) of immunocompromised patients did not receive antibiotic prophylaxis. Delays in curative antibiotic therapy were common and associated with faster occurrence of death. Finally, corticosteroid treatment, once the diagnosis of PJP is confirmed, might be linked to faster occurrence of death.
The few studies exclusively focused on patients with PJP admitted to ICU [9, 10, 44,45,46] have been retrospective and are now dated. One focused exclusively on patients with HIV infection [44] and two exclusively on patients without [9, 45]. Therefore, comparing our results with these studies may pose challenges in interpretation, potentially influenced by changes in the epidemiology of PJP patients admitted to ICU and shifts in the overall approach to care, particularly in the management of ARDS. Our findings confirm that the proportion of patients with HIV infection requiring ICU admission for PJP is no longer predominant. The observed proportion of 18.4% in our study is lower than the roughly 29% observed in the early 2000s [10], but it remains non-negligible and appears stable when compared with data from 2016 to 2020 (19.5%) [45], highlighting the ongoing nature of the HIV infection epidemic.
Our findings also confirm that beyond the increasing proportions of patients with solid or hematologic cancer and organ transplant recipients, patients with inflammatory/ autoimmune diseases constitute more than 30% of PJP cases admitted to the ICU.
The observed ICU mortality in our study among non-HIV patients was high (32.3%), aligning with some observations [45] but considerably lower than reported by others, ranging from 48% to roughly 60% [9, 10]. Similarly, our overall 6-month mortality rate was 40.5%, whereas the most recent retrospective study reported a 90-day mortality rate of 67% [46].
An unexpected result was that only 12% of patients were under prophylaxis, despite being almost immunocompromised and potentially eligible for prophylaxis according to current guidelines [23]. This situation may have improved since the 2000s–2010s, as the proportion of patients under prophylaxis was reported to be 1.1–3.6% [45, 46], results that should be considered with caution given the retrospective nature of these studies.
The second unexpected finding was that a non-negligible proportion of patients received the first dose of curative antibiotic treatment for PJP late: among patient not yet treated upon ICU admission, 12.7% received the first dose after the 96th hour. This is in line with what was reported years ago [11, 24, 27,28,29], suggesting that the practices of intensivists may not have evolved since then. Despite a rich literature emphasizing the high index of suspicion of PJP when caring for immunocompromised patients with diffuse pneumonia, there still remains a considerable gap between theory and practice. Our study further suggests that early treatment is of paramount importance, as it reveals that a delay of 4 days accelerated the time to death by a factor 6.75. This aligns with findings from earlier retrospective studies [24, 28, 29] and one prospective study, encompassing all PJP cases, whether requiring intensive care admission or not. That study demonstrated an increased risk of mortality of 1.11 for each day of delayed treatment [11]. For obvious ethical reasons, a randomized controlled trial comparing early versus delayed treatment is not feasible. Our study, utilizing propensity score weighting, represents the highest methodological standard achievable in this scenario. Hence, based on common sense (early treatment seems inherently preferable) and our study’s findings, along with prior evidence, the question appears settled: PJP should be treated as soon as the suspicion stage, and should be systematically considered in immunocompromised individuals presenting to the ICU with pneumonia and/or acute respiratory failure.
Adjunctive corticosteroid therapy in non-HIV patients with PJP has been the subject of several studies, all retrospective, some of which suggesting that corticosteroids, akin to their effects in HIV-infected patients, might improve survival, while others found no significant impact [31,32,33,34,35, 45]. Two recent studies, one monocentric including 130 patients [34], and the other multicentric including 172 solid-organ transplant receivers [35], used PS-IPW as we did, and found no difference in mortality between patients treated with corticosteroids at the initiation of curative antibiotic treatment and those either untreated with corticosteroids or treated late. Our results, on the other hand, suggest that corticosteroid therapy may be associated with a twofold faster occurrence of death. Therefore, to date, there is still no unequivocal answer to the question of adjunctive corticosteroid therapy for PJP in non-HIV patients. A definitive answer may come from a recently completed randomized trial, the results of which are pending (NCT02944045).
Our study has several limitations. First, despite being prospective and encompassing 49 ICUs, our investigation cannot claim to accurately depict the epidemiology of severe PJP in France, as it only involves approximately one-fifth of French ICUs. Secondly, like previous studies in this area, our investigation faces limitations in assessing the effects of delayed antibiotic treatment on patient outcomes due to its observational design (i.e., non-randomized). This prohibits complete certainty in controlling for all potential confounding factors, particularly within the heterogeneous population of immunocompromised patients characterized by diverse clinical profiles and case mixes. In this context, distinguishing confirmed (proven or probable cases) from equivocal cases of PJP is complicated. Third, the assessment of the utility of adjunctive corticosteroid therapy faces similar methodological limitations.
Conclusions
This prospective observational study pinpoints that few patients with PJP admitted to the ICU had benefited from antibiotic prophylaxis despite being highly immunocompromised, that delayed antibiotic treatment is frequent and associated with faster occurrence of death, and suggests that adjunctive corticosteroid therapy for PJP in non-HIV patients may also be associated with faster occurrence of death.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Pereira-Díaz E, Moreno-Verdejo F, de la Horra C, Guerrero JA, Calderón EJ, Medrano FJ (2019) Changing trends in the epidemiology and risk factors of pneumocystis pneumonia in Spain. Front Public Health 7:275. https://doi.org/10.3389/fpubh.2019.00275
Grønseth S, Rogne T, Hannula R, Åsvold BO, Afset JE, Damås JK (2021) Epidemiological and clinical characteristics of immunocompromised patients infected with Pneumocystis jirovecii in a twelve-year retrospective study from Norway. BMC Infect Dis 21:659. https://doi.org/10.1186/s12879-021-06144-1
Kolbrink B, Scheikholeslami-Sabzewari J, Borzikowsky C, von Samson- Himmelstjerna FA, Ullmann AJ, Kunzendorf U (2022) Schulte K (2022) Evolving epidemiology of pneumocystis pneumonia: findings from a longitudinal population-based study and a retrospective multi-center study in Germany. Lancet Reg Health Eur 18:100400. https://doi.org/10.1016/j.lanepe.2022.100400
Pates K, Periselneris J, Russell MD, Mehra V, Schelenz S, Galloway JB (2023) Rising incidence of Pneumocystis pneumonia: a population-level descriptive ecological study in England. J Infect 86:385–390. https://doi.org/10.1016/j.jinf.2023.02.014
Bienvenu A-L, Traore K, Plekhanova I, Bouchrik M, Bossard C, Picot S (2016) Pneumocystis pneumonia suspected cases in 604 non-HIV and HIV patients. Int J Infect Dis 46:11–17
Ricciardi A, Gentilotti E, Coppola L, Maffongelli G, Cerva C, Malagnino V et al (2017) Infectious disease ward admission positively influences P. jiroveci pneumonia (PjP) outcome: a retrospective analysis of 116 HIV positive and HIV-negative immunocompromised patients. PLoS ONE 12:e0176881
Cillóniz C, Dominedò C, Álvarez-Martínez MJ, Moreno A, García F, Torres A, Miro JM (2019) Pneumocystis pneumonia in the twenty-first century: HIV-infected versus HIV-uninfected patients. Expert Rev Anti Infect Ther 17:787–801. https://doi.org/10.1080/14787210.2019.1671823
Elango K, Mudgal M, Murthi S, Yella PR, Nagrecha S, Srinivasan V, Sekar V, Koshy M, Ramalingam S, Gunasekaran K (2022) Trends in the epidemiology and outcomes of pneumocystis pneumonia among human immunodeficiency virus (HIV) hospitalizations. Int J Environ Res Public Health 19:2768. https://doi.org/10.3390/ijerph19052768
Festic E, Gajic O, Limper AH, Aksamit TR (2005) Acute respiratory failure due to pneumocystis pneumonia in patients without human immunodeficiency virus infection: outcome and associated features. Chest 128:573–579. https://doi.org/10.1378/chest.128.2.573
Monnet X, Vidal-Petiot E, Osman D, Hamzaoui O, Durrbach A, Goujard C, Miceli C, Bourée P, Richard C (2008) Critical care management and outcome of severe Pneumocystis pneumonia in patients with and without HIV infection. Crit Care 12:R28. https://doi.org/10.1186/cc6806
Roux A, Canet E, Valade S, Gangneux-Robert F, Hamane S, Lafabrie A, Maubon D, Debourgogne A, Le Gal S, Dalle F, Leterrier M, Toubas D, Pomares C, Bellanger AP, Bonhomme J, Berry A, Durand-Joly I, Magne D, Pons D, Hennequin C, Maury E, Roux P, Azoulay É (2008) Pneumocystis jirovecii pneumonia in patients with or without AIDS, France. Emerg Infect Dis 20:1490–1497. https://doi.org/10.3201/eid2009.131668
Schmidt JJ, Lueck C, Ziesing S, Stoll M, Haller H, Gottlieb J, Eder M, Welte T, Hoeper MM, Scherag A, David S (2018) Clinical course, treatment and outcome of Pneumocystis pneumonia in immunocompromised adults: a retrospective analysis over 17 years. Crit Care 22:307. https://doi.org/10.1186/s13054-018-2221-8
Kim TO, Lee JK, Kwon YS, Kim YI, Lim SC, Kim MS, Kho BG, Park CK, Oh IJ, Kim YC, Park HY, Shin HJ (2021) Clinical characteristics and prognosis of patients with Pneumocystis jirovecii pneumonia without a compromised illness. PLoS ONE 16:e0246296. https://doi.org/10.1371/journal.pone.0246296
Burghi G, Biard L, Roux A, Valade S, Robert-Gangneux F, Hamane S, Maubon D, Debourgogne A, Le Gal S, Dalle F, Leterrier M, Toubas D, Pomares C, Bellanger AP, Bonhomme J, Berry A, Iriart X, Durand-Joly I, Magne D, Pons D, Hennequin C, Maury E, Azoulay E, Lemiale V (2021) Characteristics and outcome according to underlying disease in non-AIDS patients with acute respiratory failure due to Pneumocystis pneumonia. Eur J Clin Microbiol Infect Dis 40:1191–1198. https://doi.org/10.1007/s10096-020-04118-w
Ghembaza A, Vautier M, Cacoub P, Pourcher V, Saadoun D (2020) Risk factors and prevention of Pneumocystis jirovecii pneumonia in patients with autoimmune and inflammatory diseases. Chest 158:2323–2332. https://doi.org/10.1016/j.chest.2020.05.558
Schmajuk G, Jafri K, Evans M, Shiboski S, Gianfrancesco M, Izadi Z, Patterson SL, Aggarwal I, Sarkar U, Dudley RA, Yazdany J (2019) Pneumocystis jirovecii pneumonia (PJP) prophylaxis patterns among patients with rheumatic diseases receiving high-risk immunosuppressant drugs. Semin Arthritis Rheum 48:1087–1092. https://doi.org/10.1016/j.semarthrit.2018.10.018
Wolfe RM, Beekmann SE, Polgreen PM, Winthrop KL, Peacock JE Jr (2019) Practice patterns of pneumocystis pneumonia prophylaxis in connective tissue diseases: a survey of infectious disease physicians. Open Forum Infect Dis 6:ofz315. https://doi.org/10.1093/ofid/ofz315
Vieujean S, Moens A, Hassid D, Rothfuss K, Savarino EV, Vavricka SR, Reenaers C, Jacobsen BA, Allez M, Ferrante M, Rahier JF (2023) Pneumocystis jirovecii pneumonia in patients with inflammatory bowel disease—a case series. J Crohns Colitis 17:472–479. https://doi.org/10.1093/ecco-jcc/jjac153
Sierra CM, Daiya KC (2022) Prophylaxis for Pneumocystis jirovecii pneumonia in patients with inflammatory bowel disease: a systematic review. Pharmacotherapy 42:858–867. https://doi.org/10.1002/phar.2733
Weyant RB, Kabbani D, Doucette K, Lau C, Cervera C (2021) Pneumocystis jirovecii: a review with a focus on prevention and treatment. Expert Opin Pharmacother 22:1579–1592. https://doi.org/10.1080/14656566.2021.1915989
Alsayed AR, Al-Dulaimi A, Alkhatib M, Al Maqbali M, Al-Najjar MAA, Al- Rshaidat MMD (2022) A comprehensive clinical guide for Pneumocystis jirovecii pneumonia: a missing therapeutic target in HIV-uninfected patients. Expert Rev Respir Med 16:1167–1190. https://doi.org/10.1080/17476348.2022.2152332
Fragoulis GE, Dey M, Zhao S, Schoones J, Courvoisier D, Galloway J, Hyrich KL, Nikiphorou E (2022) Systematic literature review informing the 2022 EULAR recommendations for screening and prophylaxis of chronic and opportunistic infections in adults with autoimmune inflammatory rheumatic diseases. RMD Open 8:e002726. https://doi.org/10.1136/rmdopen-2022-002726
Zhou S, Aitken SL (2023) Prophylaxis against Pneumocystis jirovecii pneumonia in adults. JAMA 330:182–183. https://doi.org/10.1001/jama.2023.9844
Li MC, Lee NY, Lee CC, Lee HC, Chang CM, Ko WC (2014) Pneumocystis jiroveci pneumonia in immunocompromised patients: delayed diagnosis and poor outcomes in non-HIV-infected individuals. J Microbiol Immunol Infect 47:42–47. https://doi.org/10.1016/j.jmii.2012.08.024
Fillâtre P, Revest M, Belaz S, Robert-Gangneux F, Zahar JR, Roblot F, Tattevin P (2016) Pneumocystose chez les patients immunodéprimés non infectés par le VIH [Pneumocystosis in non-HIV-infected immunocompromised patients]. Rev Med Interne 37(5):327–336. https://doi.org/10.1016/j.revmed.2015.10.002
Ramirez JA, Musher DM, Evans SE, Dela Cruz C, Crothers KA, Hage CA et al (2020) Treatment of community-acquired pneumonia in immunocompromised adults: a consensus statement regarding initial strategies. Chest 158:1896–1911. https://doi.org/10.1016/j.chest.2020.05.598
Kovacs JA, Hiemenz JW, Macher AM, Stover D, Murray HW, Shelhamer J, Lane HC, Urmacher C, Honig C, Longo DL et al (1984) Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med 100:663–671. https://doi.org/10.7326/0003-4819-100-5-663
Asai N, Motojima S, Ohkuni Y, Matsunuma R, Nakashima K, Iwasaki T, Nakashita T, Otsuka Y, Kaneko N (2012) Early diagnosis and treatment are crucial for the survival of Pneumocystis pneumonia patients without human immunodeficiency virus infection. J Infect Chemother 18:898–905. https://doi.org/10.1007/s10156-012-0441-4
Song S, Zhang Y, Yu J, Xie C, Chen Y, Zhang X (2022) Time to trimethoprim/sulfamethoxazole initiation among patients with rheumatic disease complicated by Pneumocystis jirovecii pneumonia: impact on 90-day mortality. BMC Infect Dis 22:961. https://doi.org/10.1186/s12879-022-07940-z
Ewald H, Raatz H, Boscacci R, Furrer H, Bucher HC, Briel M (2015) Adjunctive corticosteroids for Pneumocystis jiroveci pneumonia in patients with HIV infection. Cochrane Database Syst Rev 2015(4):006150. https://doi.org/10.1002/14651858.CD006150
Fujikura Y, Manabe T, Kawana A, Kohno S (2017) Adjunctive corticosteroids for Pneumocystis jirovecii pneumonia in non-HIV infected patients: a systematic review and meta-analysis of observational studies. Arch Bronconeumol 53:55–61. https://doi.org/10.1016/j.arbres.2016.06.016
Wieruszewski PM, Barreto JN, Frazee E, Daniels CE, Tosh PK, Dierkhising RA, Mara KC, Limper AH (2018) Early corticosteroids for pneumocystis pneumonia in adults without HIV are not associated with better outcome. Chest 154:636–644. https://doi.org/10.1016/j.chest.2018.04.026
Inoue N, Fushimi K (2019) Adjunctive corticosteroids decreased the risk of mortality of non-HIV pneumocystis pneumonia. Int J Infect Dis 79:109–115. https://doi.org/10.1016/j.ijid.2018.12.001
Assal M, Lambert J, Chow-Chine L, Bisbal M, Servan L, Gonzalez F, de Guibert JM, Faucher M, Vey N, Sannini A, Mokart D (2021) Prognostic impact of early adjunctive corticosteroid therapy in non-HIV oncology or haematology patients with Pneumocystis jirovecii pneumonia: a propensity score analysis. PLoS ONE 16(4):e0250611. https://doi.org/10.1371/journal.pone.0250611
Hosseini-Moghaddam SM, Kothari S, Humar A, Albasata H, Yetmar ZA, Razonable RR, Neofytos D, D’Asaro M, Boggian K, Hirzel C, Khanna N, Manuel O, Mueller NJ, Imlay H, Kabbani D, Tyagi V, Smibert OC, Nasra M, Fontana L, Obeid KM, Apostolopoulou A, Zhang SX, Permpalung N, Alhatimi H, Silverman MS, Guo H, Rogers BA, MacKenzie E, Pisano J, Gioia F, Rapi L, Prasad GVR, Banegas M, Alonso CD, Doss K, Rakita RM, Fishman JA (2023) Adjunctive glucocorticoid therapy for Pneumocystis jirovecii pneumonia in solid organ transplant recipients: a multicenter cohort, 2015–2020. Am J Transpl S1600–6135(23):00858–00864. https://doi.org/10.1016/j.ajt.2023.11.003
Lagrou K, Chen S, Masur H, Viscoli C, Decker CF, Pagano L, Groll AH (2021) Pneumocystis jirovecii disease: basis for the revised EORTC/MSGERC invasive fungal disease definitions in individuals without human immunodeficiency virus. Clin Infect Dis 72(Suppl 2):S114–S120. https://doi.org/10.1093/cid/ciaa1805
Kanne JP, Yandow DR, Meyer CA (2012) Pneumocystis jiroveci pneumonia: high-resolution CT findings in patients with and without HIV infection. AJR Am J Roentgenol 198:W555-561
Fauchier T, Hasseine L, Gari-Toussaint M, Casanova V, Marty PM, Pomares C (2016) Detection of Pneumocystis jirovecii by quantitative PCR to differentiate colonization and pneumonia in immunocompromised HIV positive and HIV-negative patients. J Clin Microbiol 54(6):1487–1495. https://doi.org/10.1128/JCM.03174-15
Wei LJ (1992) The accelerated failure time model: a useful alternative to the Cox regression model in survival analysis. Stat Med 11:1871–1879
Desai RJ, Franklin JM (2019) Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ 367:l5657. https://doi.org/10.1136/bmj.l5657
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963. https://doi.org/10.1001/jama.270.24.2957
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710. https://doi.org/10.1007/BF01709751
Stürmer T, Webster-Clark M, Lund JL, Wyss R, Ellis AR, Lunt M, Rothman KJ, Glynn RJ (2021) Propensity score weighting and trimming strategies for reducing variance and bias of treatment effect estimates: a simulation study. Am J Epidemiol 190:1659–1670. https://doi.org/10.1093/aje/kwab041
Bruneel F, Veziris N, Chevret S, Wolff M, Bedos JP (2009) Retrospective review of Pneumocystis jirovecii pneumonia in a French intensive care unit (1994–2000). Int J STD AIDS 20:441–442. https://doi.org/10.1258/ijsa.2009.009107
Lemiale V, Debrumetz A, Delannoy A, Alberti C, Azoulay E (2013) Adjunctive steroid in HIV-negative patients with severe Pneumocystis pneumonia. Respir Res 14(1):87. https://doi.org/10.1186/1465-9921-14-87
- Giacobbe DR, Dettori S, Di Pilato V, Asperges E, Ball L, Berti E, et al; JIR-ICU investigators (collaborators); Critically Ill Patients Study Group of the European Society of Clinical Microbiology and Infectious Diseases (ESGCIP), and the Fungal Infection Study Group of the European Society of Clinical Microbiology and Infectious Diseases (EFISG) (2023) Pneumocystis jirovecii pneumonia in intensive care units: a multicenter study by ESGCIP and EFISG. Crit Care 27:323. https://doi.org/10.1186/s13054-023-04608-1
Definition Task Force ARDS, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E et al (2012) Acute respiratory distress syndrome: the Berlin definition. JAMA 307:2526–2533
Desoubeaux G, Chesnay A, Mercier V, Bras-Cachinho J, Moshiri P, Eymieux S, De Kyvon MA, Lemaignen A, Goudeau A, Bailly É (2019) Combination of β-(1, 3)-D-glucan testing in serum and qPCR in nasopharyngeal aspirate for facilitated diagnosis of Pneumocystis jirovecii pneumonia. Mycoses 62:1015–1022. https://doi.org/10.1111/myc.12997
Wettstein RB, Shelledy DC, Peters JI (2005) Delivered oxygen concentrations using low-flow and high-flow nasal cannulas. Respir Care 50:604–609
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, Pearl R, Silverman H, Stanchina M, Vieillard-Baron A, Welte T (2007) Weaning from mechanical ventilation. Eur Respir J 29:1033–1056. https://doi.org/10.1183/09031936.00010206
Acknowledgements
The authors wish to thank all the following members of the PCP-MULTI Study group who contributed to patient enrolment: Auchabie Johann, Service de Médecine Intensive Réanimation, Centre hospitalier de Cholet, Cholet; Beuret Pascal, Service de Médecine Intensive Réanimation, Centre hospitalier de Roanne, Roanne; Darreau Cédric, Réanimation Médico-Chirurgicale, Centre hospitalier du Mans, Le Mans; Desmeulles Isabelle, Service de réanimation polyvalente, Centre hospitalier public du Cotentin, Cherbourg-en-Cotentin; Guervilly Christophe, Service de Médecine Intensive Réanimation APHM Hôpital Nord, Marseille; Hong Tuan Ha Vivien, Réanimation polyvalente, Grand Hôpital de l’Est Francilien, Meaux; Jochmans Sébastien, Service de Médecine Intensive Réanimation, Centre hospitalier de Meulin, Melun; Jozwiak Mathieu, Service de Médecine Intensive Réanimation, CHU de Nice; Louis Guillaume, Service de Médecine Intensive Réanimation Centre hospitalier régional Metz-Thionville, Metz; Navellou Jean-Christophe, Service de Médecine Intensive Réanimation, CHU Jean Minjoz, Besançon; Neuville Mathilde, Réanimation polyvalente, Hôpital Foch, Suresnes; Pichon Nicolas, Service de Médecine Intensive Réanimation, Centre Hospitalier Dubois, Brive La Gaillarde; Sagnier Anne, Réanimation Polyvalente, CH de beauvais, Beauvais; Schnell David, Réanimation polyvalente, Centre hospitalier d’Angoulême, Angoulême.
Funding
Financial support was provided only by the Centre Hospitalier Universitaire d’Orléans, Orléans, France. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Role of the funder/sponsor: the funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval.
Author information
Authors and Affiliations
Consortia
Contributions
TK and TB had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All the authors give their agreement to be accountable for all aspects of the work and ensure the accuracy and integrity of any part of the work. Concept and design: TK and TB. Acquisition, analysis, or interpretation of data: all the authors. Drafting of the manuscript: TK and TB. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: TB. Administrative, technical, or material support: TK and TB. Supervision: TK and TB. The corresponding author (TB) attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Conflicts of interest
There are no competing interests for any author concerning the submitted work.
Ethics approval and consent to participate
This study adhered to French legal regulations for prospective non-interventional studies and was conducted in accordance with the Declaration of Helsinki and its later amendments. Patients and families received both verbal and written information about the study upon patient eligibility, with the option to consent or decline participation. The study protocol received approval from the ethics committee of the French Intensive Care Society on May 20, 2020 (#CE SRLF 20-48).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the PCP-MULTI Study group are listed in the Acknowledgements Section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kamel, T., Janssen-Langenstein, R., Quelven, Q. et al. Pneumocystis pneumonia in intensive care: clinical spectrum, prophylaxis patterns, antibiotic treatment delay impact, and role of corticosteroids. A French multicentre prospective cohort study. Intensive Care Med 50, 1228–1239 (2024). https://doi.org/10.1007/s00134-024-07489-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-024-07489-2