Abstract
Multiple organ failure following a septic event derives from immune dysregulation. Many of the mediators of this process are humoral factors (cytokines), which could theoretically be cleared by direct adsorption through a process called hemoperfusion. Hemoperfusion through devices, which bind specific molecules like endotoxin or theoretically provide non-specific adsorption of pro-inflammatory mediators has been attempted and studied for several decades with variable results. More recently, technological evolution has led to the increasing application of adsorption due to more biocompatible and possibly more efficient biomaterials. As a result, new indications are developing in this field, and novel tools are available for clinical use. This narrative review will describe current knowledge regarding technical concepts, safety, and clinical results of hemoperfusion. Finally, it will focus on the most recent literature regarding adsorption applied in critically ill patients and their indications, including recent randomized controlled trials and future areas of investigation.
Graphical abstract
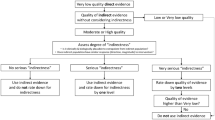
Clinical trials for the assessment of efficacy of hemoperfusion in septic patients should apply the explanatory approach. This includes a highly selected homogenous patient population. Enrichment criteria such as applying genetic signature and molecular biomarkers allows the identification of subphenotypes of patients. The intervention must be delivered by a multidisciplinary team of trained personnel. The aim is to maximize the signals for efficacy and safety. In a homogenous cohort, confounding uncontrolled variables are less likely to exist. Trials with highly selected populations have a high internal validity but poor generalizability. The parallel design described in the figure is robust and usually is required by regulatory agencies for the approval of a new treatment. Allocation concealment and randomization are key to minimize bias such as confirmation bias, observer bias. The intervention should be delivered following a strict protocol. Deviations from the protocol might negatively influence the potential effects of the therapies. Surrogates such as cytokine measurement are adequate primary outcomes in phase 3 trials with small sample size because there is a higher likelihood of finding positive results concerning surrogate markers than in respect with clinical outcomes. Once a trial shows positive results concerning surrogate markers, a rationale for another phase 3 trial exploring clinical outcomes is built, justifying the allocation of financial sources to the intended trial.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although technology has significantly evolved and current cartridges for hemoperfusion can be safely used with many potential applications, current evidence is insufficient to recommend routine use in all patients presenting indications. Further research is needed, including a better refinement of the indications for extracorporeal blood purification techniques and improved selectivity of target solutes, especially once immunophenotypes of septic patients can be specifically identified and monitored. |
Pathophysiology of sepsis
Sepsis is a complex clinical and biological syndrome defined as life-threatening organ dysfunction caused by a dysregulated host response to infection [1]. It begins as an infection that produces an inflammatory response in the host, triggered by the interaction between multiple soluble mediators [2]. The inflammatory response to infection by innate immunity is usually controlled, localized, and protective [3]. The interaction between resistance (inflammatory response) and resilience (limiting inflammation by the adaptive immunity) is the key to survival, but in some circumstances not completely understood, this complex and delicate balance is lost, and sepsis syndrome may develop. In this process of dysregulated response, both the infected and distal organs may be injured, leading to a life-threatening clinical condition [1]. Such a process tends to cause excessive production or suppression of cytokines and other mediators that affect vital organ function and triggers further inflammatory and counter-inflammatory pathways [4, 5]. The dominant clinical phenotypes of these biological events are sepsis and septic shock where patients may die due to intractable inflammation or persistent immunoparalysis.
The blood purification hypothesis
Blocking or attenuating the impact of soluble mediators offers protection in acute animal models of fulminant infections [6]. Thus, manipulating the soluble components of the host response is theoretically attractive. This approach represents the target of several studies although remaining controversial [3]. Previous attempts to modulate the immune response by targeting single cytokines have failed [7]. Thus, the blood purification concept based on the non-specific manipulation of several mediators’ plasma levels has been proposed [8, 9]. Hemoperfusion can theoretically deliver non-specific treatment, as discussed below.
The rationale for hemoperfusion
Insufficient clearance of soluble pro-inflammatory mediators may be one of the reasons for the lack of significant evidence of clinical efficacy of adjuvant extracorporeal blood purification for sepsis [10]. One may speculate that direct contact of blood with highly adsorptive resins in an extracorporeal circuit (hemoperfusion) should logically increase clearance compared to indirect removal by dialysis or hemofiltration-based approaches. Hemoperfusion is a modality for blood purification in which solute removal is achieved by binding molecules to adsorbent materials [11] although the evidence supporting this approach is inconclusive, so far. This mechanism is only partially present during continuous renal replacement therapies (CRRT) but its clinical relevance is likely negligible, except, perhaps, for membranes with specific designs, like polymethylmethacrylate or oXiris® (Baxter, Meyzieu, France) [12].
Clearance of specific substances does not only depend on perfusion but also on the surface characteristics of the materials used and their interaction with specific substances. Devices containing sorbent beds present large surface areas and optimal biocompatibility and provide highly efficient removal of solutes especially in the middle to high molecular weight range [13]. Extracorporeal blood purification can be performed by direct hemoperfusion or by plasma-perfusion after plasma separation. The possibility of conducting such hemoperfusion or a plasma-perfusion treatment depends on the biocompatibility of the sorbent particles and the possibility to place the sorbent in direct contact with the cellular component of blood without causing cell damage [14].
Technical concepts of adsorption
Sorbents can be composed of natural (e.g., carbons) or synthetic materials (e.g., polymers) [12] (Table 1). Sorbents are generally prepared as beads, granules, flakes, fibers, spheres, cylindric pellets ranging from 50 μm to 1.2 cm. They are characterized by a high surface area to mass ratio, varying from 300 to 1200 m2/g, which helps to magnify their adsorptive capacity [15]. Beads are contained in a plastic cartridge provided with ports for plasma/blood inflow and outflow and specific screens to avoid dissemination of particles into the circulation. Once the solvent flows into the sorbent, solute removal occurs through several phases (Fig. 1): (a) the convective movement from the bulk fluid to the external surface of the bead, which requires a further diffusive step through a “boundary layer”; (b) the internal mass transfer of the solute from the outer surface of the sorbent into the internal porous structure through a diffusive mechanism, and (c) the final binding (adsorption) of the solute onto the porous surface [15].
The process of adsorption of a solute dissolved or dispersed in the fluid phase (blood) occurs in subsequent steps: (1) Permeation of blood into the interparticle space available inside the cartridge. This is the space between the beads and corresponds to a series of tortuous channels in parallel characterized by the dimensions of the beads and the packing density of the sorbent. The flow condition depends on the interparticle porosity and the viscosity of blood, the blood flow and the relative blood flow velocity in each cross section of the cartridge. This step is governed by complex physical laws such as Darcy’s law and the Karmann–Cozeny equation. (2) The external (interphase) mass transfer of the solute from the bulk fluid by convection through a thin film or boundary layers, to the outer surface of the sorbent. (3) The internal (intraphase) mass transfer of the solute by pore diffusion from the outer surface of the adsorbent to the inner surface of the internal porous structure. This also implies a surface diffusion along the porous surface and adsorption of the solute onto the porous surface
The final binding is governed by the density and diameter of the pores of the sorbent structure (pore diameter ranges generally 20–500 Å). Hydrophobic binding is the main mechanism of solute removal from the extracorporeal circulation [14]. Although other forces are involved such as van der Waals and ionic bonds, the hydrophobic affinity of the sorbent with the target solutes represents the main mechanism of currently available sorbent cartridges [15]. Once binding is complete, this part of the cartridge is saturated and is no longer available for blood purification, which is why sorbents have a limited lifespan and should be changed once fully saturated. The analysis of adsorption isotherms describes the phase of saturation as a dynamic equilibrium between adsorption and desorption (i.e., the release of adsorbed compound). This turnover however represents a small component of the dynamic process that occurs when van der Waals forces and ionic bonds are involved. Because these forces are not as strong as the hydrophobic forces, the links can be reversible, and part of the adsorbed solute can return to the fluid phase if the equilibrium for diffusion and the chemical gradients favor this process. However, this is of limited biological impact, and the sites become saturated immediately again. Dynamic turnover (adsorption/desorption) represents in most cases 5–7% of total mass removal [14, 15].
The design of each sorbent cartridge should consider several aspects, such as the cost of the polymers, high resistance to fouling, maximal biocompatibility, and the absence of undesirable side effects. Furthermore, the combination of porosity, polymers, and internal pathways inside the cartridge should be designed to maximize the mass transfer along the sorbent bed [15]. Another important aspect to consider is the flow rate into the cartridge. In most cases, suggested blood flow ranges between 100 and 200 mL/min, but the role of different blood flows in affecting system efficiency should be further elucidated. Finally, the selectivity of the adsorption for the target solutes is a fundamental aspect of this technology. All these aspects (i.e., polymer type, design, packing of the sorbent, flow, saturation) can be varied and combined into different products, significantly affecting the clinical effects of adsorption-based extracorporeal blood purification and their indications [16].
Available sorbents
Charcoal and resins
The first applications of sorbent hemoperfusion in acute patients have been in the treatment of drug intoxication and poisoning because, in specific cases, adsorption is by far more efficient than hemodialysis [17]. Generally, this has been achieved with charcoal adsorption or resins. Such devices typically contain between 100 and 300 g of activated charcoal or between 300 and 650 g of resin. The blood flow for efficient drug removal is approximately 300 mL/min, up to 450 mL/min and intermittent hemoperfusion is usually performed for 4 h. Beyond this treatment time, additional clearance is unlikely to occur due to device saturation and double pool kinetics in the body.
Retrospective studies have shown that hemoperfusion is associated with increased survival in case of paraquat ingestion when performed early [18], and that hemoperfusion sometimes provides better clearance than high-flux hemodialysis [19]. Hemoperfusion can also be indicated in other intoxications, including Amanita phalloides mushroom intoxication, overdose with barbiturates, valproic acid, theophylline, aluminum, and carbamazepine [20]. Nevertheless, hemodialysis may be of some benefit for theophylline [21], valproic acid [22] barbiturates [23], and carbamazepine [24] intoxication.
Polymyxin B hemoperfusion
An adsorbent cartridge composed of polystyrenic fibers bound to polymyxin B (PMX)® (Toray Medical Co.Ltd., Tokyo, Japan) has been marketed in Japan and in Europe for the removal of endotoxins during sepsis and septic shock [25]. Endotoxin levels decrease in vitro within minutes after starting PMX hemoperfusion (PMX-HP) [26]. This treatment requires sessions of 2 h of hemoperfusion and heparin anticoagulation to deliver a complete treatment without circuit clotting with a blood flow rate ranging between 80 and 120 mL/min. The first randomized controlled trial (EUPHAS) of PMX HP enrolled 64 patients with septic shock and intra-abdominal Gram-negative infections and showed improvements in hemodynamics (mean arterial pressure, catecholamine dose), respiratory function, sepsis-related organ failure scores and mortality in treated patients [27]. The second trial (ABDOMIX) included 243 septic shock patients with peritonitis [28]: during this study, patients were randomized based of the presence of an abdominal infection and regardless of the presence of Gram-negative bacteria. This study reported a non-significant difference in mortality rate of 27% in the PMX HP group and 19.5% in the conventional group. This study however was questioned due to low mortality in the control group and low percentage of patients completing the intervention in the studied group. Finally, a third large randomized, double-blind, controlled trial (EUPHRATES) found no mortality benefits with this therapy [29]. For the first time, this study applied, as a criterion to enroll patients, the estimation of circulating endotoxin levels through a point-of-care test (endotoxin activity assay [EAA]). This interesting approach makes this treatment potentially open to monitoring because a laboratory endpoint can be repeatedly measured and targeted during therapy. In fact, the measurement of endotoxin may be more important than the type of bacteria in determining response to therapy. For example, in the EUPHRATES study, 20% of patients had an infection with Gram-positive bacteria and still displayed endotoxemia and many patients without bacterial isolates had a positive EAA and some clinical benefit from the therapy [29].
A recent post-hoc study, published after the results of the EUPHRATES randomized trial, showed a 10% reduction in 28-day mortality, after adjusting for organ failure scores and baseline mean arterial pressure, for patients with EAA values from 0.6 to 0.89 [30]. Patients with EAA reductions above 13% were shown to have improved mortality. However, there was no difference in EAA reductions between patients undergoing PMX-HP and controls, raising questions about the clinical impact of this strategy and the utilization of EAA as a reliable endpoint [30] (Table 2).
In response to the above findings, a further randomized controlled trial is being conducted in North America (the TIGRIS trial, ClinicalTrials.gov Identifier: NCT03901807). The study has planned for a sample size of 150 patients specifically including those with EAA within the range of ≥ 0.60 to < 0.90. In light of the above considerations, until the data from such a trial is available, PMX-HP efficacy on mortality is still under discussion.
In addition, a recent observation with a mass spectrometry methodology, found that a "lipopolysaccharide burden”, presumably translocated from the human gut, is also present in healthy controls [31]. However, spikes of endotoxemia appear to occur in septic shock critically ill patients, possibly because of a higher bacterial load, vascular-gut barrier alteration, or a decrease in lipopolysaccharide clearance capacity [31]. Improved opportunities to monitor specific septic clinical states and severity with biomarkers might significantly optimize the application of extracorporeal blood purification. In fact, a specific and sensitive biomarker could theoretically improve our capacity to apply these treatments in a selective and timely manner, track their clinical effectiveness over time, and allow timely cessation of the extracorporeal circulation.
Coupled plasma filtration adsorption
Although initial encouraging results were obtained with this technique, coupled plasma filtration adsorption (CPFA) is not currently recommended in patients with septic shock or hyperinflammation after the negative results of the COMPACT [32] and COMPACT-2 [33] trials. Such studies, in fact, showed no significant benefit of CPFA and possible potential harm, particularly in patients without acute kidney injury or CRRT requirements.
CytoSorb® hemoperfusion
The CytoSorb® (CytoSorb®, CytoSorbents Inc, New Jersey, USA) device is a cartridge intended for direct hemoperfusion that has repeatedly displayed a high safety profile in terms of biocompatibility and ease of use [34]. It is composed of polystyrene divinylbenzene and polyvinylpyrrolidone copolymers and targets molecules in the 5–50 kDa range, which includes the molecular mass of several cytokines [35]. Treatment with CytoSorb®, according to the Food and Drug Administration, can be prolonged up to 24 h with the view that solute spillover is negligible even with such prolonged treatment time. Maximum effectiveness in terms of sorbent saturation has been reported at around 12 h [https://www.fda.gov/media/136866/download]. The recommended blood flow rate is 150–500 mL/min, and the device can be run both as a stand-alone treatment and in series with CRRT. The cartridge can also be applied during extracorporeal membrane oxygenation (ECMO) or cardiopulmonary bypass. In this case, CytoSorb® placement should be in a shunt which comes off the main flow component of the circuit as is current practice with hemoconcentrators, and flow monitoring (≤ 700 mL/min.) is recommended.
A decrease in cytokine levels in septic patients treated with CytoSorb® has been reported [36], and interleukin-6 (IL-6) has been identified as a diagnostic tool and, frequently, as a potential clinical target of CytoSorb® treatment [37, 38]. However, many of these studies have been uncontrolled, and the ultimate demonstration of CytoSorb® effects should be tested in a large, controlled, adequately sized trial verifying the target solute modification in treated patients versus controls. Such evidence is currently lacking. A propensity study by Scharf et al. showed that the decrease in IL-6 in critically ill patients with hypercytokinemia was not significantly different between patients treated with CytoSorb® and those managed without [39]. Nevertheless, it is possible that this heterogenous patient population may need to be further stratified in terms of specific indications, risk of death, and clinical and laboratory endpoints [40, 41]. Of interest, CytoSorb® can be used as a second element in series into another extracorporeal circuit, such as CRRT [42], cardiopulmonary bypass [43], ECMO [44]. However, a longitudinal cytokine profiling study before and after ECMO start in patients with coronavirus disease 2019 (COVID-19) found that ECMO does not imply a significant cytokine increase and that, even if patients seem to show a decrease in IL-6, IL-10, and TNF-gamma, patients without CytoSorb® hemoperfusion also display a decrease in cytokine concentration [45]. This study clearly revealed our inadequate understanding of cytokine kinetics in different clinical conditions, and the need for improved knowledge to optimize the modulation of cytokine levels. In fact, the treatment of COVID-19 patients with extracorporeal blood purification and specifically with CytoSorb® hemoadsorption has been recently investigated [46, 47], discussed and questioned [48].
Even if several case series have shown promising results [35, 44], at least four randomized trials have not shown any benefit in terms of mortality [37, 43, 46, 49], and two prospective studies (a matched controlled one and a randomized trial) have described potential harm [41, 47] (Table 2). According to the above studies, CytoSorb® does not appear to significantly affect vasopressor requirement, measured cytokine levels, organ dysfunction, and mortality of adult critically ill patients with signs of hyperinflammation due to cardiac surgery, infection, sepsis, or COVID-19. In response to the above findings of such studies, a recent editorial openly criticized public funding of CytoSorb® treatment in Germany and highlighted the absence of convincing literature supporting its effectiveness and unjustified costs [50].
Some reports have recently described the application of hemoadsorption in the pediatric setting. Both DH-PMX [51] and CytoSorb® have been safely used in cases series of septic shock [52], hemophagocytic lymphohistiocytosis [53], and multi-organ failure (MOF) [54], but pediatric randomized trials are not currently planned. More information on this delicate population will need to be provided by large prospective databases.
Both in children and in adults, CytoSorb® has been used to significantly and effectively reduce bilirubin and myoglobin serum concentrations, proving itself as a potential tool for patients with different forms of liver failure with hyperbilirubinemia [55, 56] and rhabdomyolysis [57, 58].
Jafron HA series for hemoperfusion/plasmaperfusion
A group of novel cartridges for hemoperfusion have recently been developed: neutro-macroporous resins made of styrene–divinylbenzene copolymer, called HA130, HA230, and HA330 (Jafron Biomedical, Guangdong, China) [59]. The pore size distributions of the resins are 500 D–40 kD in HA130, 200 D–10 kD in HA230, and 500 D–60 kD in HA330/HA380. HA130 is mainly used in chronic conditions in combination with hemodialysis during one or more sessions of the week. In such conditions, the additional role of adsorption seems to induce a significant benefit in symptoms such as pruritus, muscular weakness, appetite, and anemia [59]. The HA230 is mostly indicated in acute intoxications especially in cases of a drug overdose, pesticides, and industrial toxin poisoning [59]. The HA330 and HA380 cartridges are mostly indicated in acute inflammatory conditions such as sepsis, trauma, burns, pancreatitis and various cytokine release syndromes (CAR-T cell therapy, severe COVID-19, hemophagocytic syndrome) [59]. A small, randomized study in subjects with sepsis and acute lung injury and treated for 3 days with 2 h-long sessions of HA330, compared with usual care, selected cytokine levels fell. Moreover, the study showed significant improvements in patient oxygenation and 28-day mortality (67% in treated patients vs 28% in control patients) [60]. Similar results but with no effect on mortality were shown in another small, randomized trial where the treatment was combined with pulse high-volume hemofiltration [61]. Blood flow rate with HA330 cartridge is typically the same than the flow used during routine CRRT and can therefore range from 150 to 250 mL/min.
It should be noted that a specific adsorbing resin for bilirubin and bile acids is incorporated into a cartridge to be used in a technique called DPMAS (double plasmafiltration molecular adsorption system). This sorbent has been used alone or in combination with the HA330-II cartridge to achieve the removal of cytokines and bilirubin /bile acids in acute liver failure and fulminant hepatitis in adults and children [62, 63]
Seraph-100 microaffinity pathogen binder
Of particular interest, the Seraph-100® (ExThera, Martinez, CA) cartridge was designed to remove pathogens from the bloodstream [64]. It contains ultra-high molecular weight polyethylene beads with end-point-attached heparin, which is considered able to immobilize pathogens similarly to the action of heparan sulfate on the cell surface [65]. It can be run both as a standalone treatment and in series with a CRRT circuit. Blood flow rates range from 150 to 350 mL/min and treatment time may be extended up to 24 h at the discretion of the attending clinicians [https://www.fda.gov/media/137105/download]. If future controlled studies confirm its effectiveness in septic patients and those with complicated COVID-19 infections, it could warrant a multi-modal approach to the treatment of dysregulated inflammation, not only by removing cytokines from the bloodstream but also by acting on bacteremia and viremia (including damage associated molecular patterns, associated with cytokine hyperproduction).
Open questions: research methodology, unwanted drug clearance, timing, dose, duration, anticoagulation, and costs
More research is needed to establish the real and effective role of extracorporeal blood purification therapies in the critical care setting. The evidence for the clinical effectiveness of adsorption therapies requires a well-structured research agenda. We should also consider that initial randomized controlled trials should assess different primary endpoints rather than mortality to also assess other important effects of extracorporeal blood purification such as ventilation-free days, vasopressor-therapy-free days, invasive organ support-free days or intensive care unit-free days (Fig. 2). More mechanistic studies must be conducted to better understand which molecules should be targeted in a specific clinical condition. Some authors suggest that variability in host immune-phenotypes and clinical responses should be fully appraised and urgently considered as the focus of future investigations in this setting [48]. Another important black box is the removal of protein-bound molecules vs free molecules. Until these issues have been clearly addressed, positive randomized trials of hemoperfusion seem unlikely.
Clinical trials for the assessment of efficacy of hemoperfusion in septic patients should apply the explanatory approach. This includes a highly selected homogenous patient population. Enrichment criteria such as applying genetic signature and molecular biomarkers allow the identification of clinical subphenotypes. The intervention must be delivered by a multidisciplinary team of trained personnel. The aim is to maximize the signals for efficacy and safety. In a homogenous cohort, confounding uncontrolled variables are less likely to exist. Trials with highly selected populations have a high internal validity but poor generalizability. The parallel design described in the figure is robust and usually is required by regulatory agencies for the approval of a new treatment. Allocation concealment and randomization are key to minimize bias such as confirmation bias, observer bias. The Intervention should be delivered following strict protocols. Any deviation from the protocol negatively influences the potential effects of the therapies. Surrogates such as cytokine measurement are adequate primary outcomes in phase 3 trials with small sample size because there is a higher likelihood of finding positive results. Once a trial shows positive results concerning surrogate markers, a rationale for another phase 3 trial exploring clinical outcomes is built, justifying the allocation of financial sources to the intended trial
A recent updated systematic review on extracorporeal cytokine adsorption therapy [66] explicitly concluded that the efficacy and safety of this strategy in combination with standard care in patients with sepsis/septic shock and undergoing cardiac surgery has not been established.
Evidence assessing the pharmacokinetic behavior of antibiotics typically used in patients undergoing hemoperfusion is limited, and only a few data exist coming from small and heterogeneous studies [67,68,69,70,71,72]. Due to the critical importance of optimal antimicrobial treatment in sepsis, it seems crucial to understand and compensate for such extracorporeal loss during hemoperfusion. Unselective solute clearance and the potential benefit of hemoperfusion “rebalancing immunity” can be neutralized by side effects where the indiscriminate removal of “good” solutes may play a central role in determining patient outcomes. Such unselected drug clearance in patients with sepsis is an under-researched area. In 2002, an investigation assessed a biocompatible sorbent cartridge (Betasorb®, Renal Tech) [67], specifically manufactured for high-efficiency removal of substances in the middle molecular weight range, like ß2-microglobulin and cytokines [68]. It applied such treatment to uremic blood and found effective removal of glycopeptides and other non-antimicrobial agents (digoxin, theophylline, phenobarbital, phenytoin, carbamazepine, valproic acid, tacrolimus, and cyclosporine A). In contrast, aminoglycosides were less affected by the cartridge. A recent in vitro study evaluated the adsorption capacity of CytoSorb® for many common antimicrobial drugs: vancomycin, gentamicin, meropenem, flucloxacillin, piperacillin, ciprofloxacin, rifampicin, fluconazole and voriconazole [67]. The study showed that all investigated drugs were adsorbed to the surface of the CytoSorb® cartridge in a non-linear fashion leading to saturation of the adsorbent surface and a progressive reduction in clearance over time. Consequently, additional extra doses of antimicrobials must be administered within the first few hours of initiation of hemoperfusion to maintain a clinically adequate steady-state serum concentration. A recent prospective observational study, designed to quantify the adsorption of vancomycin (as a continuous infusion with a preceding loading dose over 2 h) by CytoSorb®, demonstrated significant adsorption of vancomycin with a linear decrease during CytoSorb® treatment [69]. A total of 160 vancomycin serum samples from 7 patients with septic shock were included in the analysis and 15% of the samples were collected during CytoSorb® treatment. The study showed significant adsorption of vancomycin by the CytoSorb® device (max. 572 mg) and the necessity to administer extra doses to achieve therapeutic exposure. An interventional experimental study investigated hemoadsorption performed with CytoSorb® on 17 drugs: clindamycin, fluconazole, linezolid, meropenem, piperacillin, anidulafungin, ganciclovir, clarithromycin, posaconazole, teicoplanin, tobramycin, ceftriaxone, ciprofloxacin, metronidazole, liposomal amphotericin B, flucloxacillin and cefepime [70]. The only drug not affected by hemadsorption was ganciclovir. The remaining drugs had an effective clearance, declined over time, considered as moderate for fluconazole (282%) and linezolid (115%), mild for liposomal amphotericin B (75%), posaconazole (32%) and teicoplanin (31%) and negligible for all other drugs. Finally, it has been demonstrated in vitro that many other drugs can be actively eliminated by Cytosorb® including remdesivir, dabigatran, edoxaban, rivaroxaban, and ticagrelor [71, 72].
Another open question related to the dosing of hemoperfusion. It is possible that some patients would require “higher doses” and repeated cycles of adsorption [73], with frequent and sequential changes of the cartridges. Again, we currently do not know how early and how long the treatment session should be (i.e., the timing to start and the timing to stop), nor whether the anticoagulation regime has an impact (e.g., by ensuring effective perfusion, prolonging cartridge use, or reducing inflammatory triggering through the coagulation cascade). Finally, the high cost of these devices must be definitively justified in terms of clinical effectiveness (i.e., reduction of hospital-centered outcomes), particularly in times of economic restraints.
Considering current limited knowledge and available evidence regarding hemoperfusion techniques and devices, we should strongly recommend a focused research agenda. Some patients may benefit from adsorption-based extracorporeal blood purification, but we need to identify such individuals or group of patients using adequate biomarkers or phenotype identification techniques. For the moment these technologies should probably be considered experimental and in the context of a specific research protocol.
Conclusion
Evolution of extracorporeal blood purification has proceeded constantly over the last two decades. Hemoperfusion and the design of biocompatible cartridges with the potential for customizing the target solutes and implementing safe and selective treatments are currently driving the development of the latest generation of blood purification devices. Our understanding of critical care pathophysiology and hyperinflammatory diseases has also evolved, and it is now clear that each patient requires a tailored approach. It appears likely that hemoperfusion research will switch from large-scale randomized trials to tailored, adaptive studies that include only patients meeting specific and objective criteria (i.e., biomarkers, clinical phenotypes) that offer plausible indications for treatment and/or endpoints for the assessment of the biological efficacy of blood purification.
References
Singer M, Deutschman CS, Seymour CW et al (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315:801–810
Denning NL, Aziz M, Gurien SD, Wang P (2019) Damps and nets in sepsis. Front Immunol 10:1–15. https://doi.org/10.3389/fimmu.2019.02536
Van Der Poll T, Van De Veerdonk FL, Scicluna BP, Netea MG (2017) The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol 17:407–420
Delano MJ, Ward PA (2016) The immune system’s role in sepsis progression, resolution, and long-term outcome. Immunol Rev 274:330–353. https://doi.org/10.1111/imr.12499
Hotchkiss R, Monneret G, Payen D (2013) Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol 13:862–874. https://doi.org/10.1038/nri3552.Sepsis-induced
Wiersinga WJ, Leopold SJ, Cranendonk DR, van der Poll T (2014) Host innate immune responses to sepsis. Virulence 5:36–44. https://doi.org/10.4161/viru.25436
Deans KJ, Haley M, Natanson C et al (2005) Novel therapies for sepsis: a review. J Trauma Inj Infect Crit Care 58:867–874. https://doi.org/10.1097/01.TA.0000158244.69179.94
Barzilay E, Kessler D, Berlot G, Gullo A, Geber D, Ben Zeev I (1989) Use of extracorporeal supportive techniques as additional treatment for septic-induced multiple organ failure patients. Crit Care Med 17:634–637
Rimmelé T, Kellum JA (2011) Clinical review: blood purification for sepsis. Crit Care 15:1–10. https://doi.org/10.1186/cc9411
Ankawi G, Neri M, Zhang J et al (2018) Extracorporeal techniques for the treatment of critically ill patients with sepsis beyond conventional blood purification therapy: the promises and the pitfalls. Crit Care 22:1–16. https://doi.org/10.1186/s13054-018-2181-z
Clark WR, Gao D, Lorenzin A, Ronco C (2018) Membranes and Sorbents. Contrib Nephrol 194:70–79. https://doi.org/10.1159/000485603
Feri M (2019) “In vitro comparison of the adsorption of inflammatory mediators by blood purification devices”: a misleading article for clinical practice? Intensive Care Med Exp. https://doi.org/10.1186/s40635-018-0214-1
Clark WR, Ferrari F, La Manna G, Ronco C (2017) Extracorporeal sorbent technologies: basic concepts and clinical application. Contrib Nephrol 190:43–57. https://doi.org/10.1159/000468911
Ronco C, Bordoni V, Levin NW (2002) Adsorbents: from basic structure to clinical application. Contrib Nephrol 137:158–164. https://doi.org/10.1159/000060242
Ferrari F, Clark W (2018) Ronco C (2018) Sorbents: from basic structure to clinical application. In: Ronco C, Bellomo R, Kellum JA, Ricci Z (eds) Crit. Care Nephrol., 3rd edn. Elsevier
Ankawi G, Fan W, Pomarè Montin D et al (2019) A new series of sorbent devices for multiple clinical purposes: current evidence and future directions. Blood Purif 47:94–100. https://doi.org/10.1159/000493523
Winchester J, Harbord N, Charen E, Ghannoum M (2015) Use of dialysis and hemoperfusion in treatment of poisioning. In: Daugirdas JT, Blake PG, Ing TS (eds) Handb. Dial., 5th edn. Lippincott
Rao R, Bhat R, Pathadka S et al (2017) Golden hours in severe paraquat poisoning-the role of early haemoperfusion therapy. J Clin Diagnostic Res 11:OC06–OC08. https://doi.org/10.7860/JCDR/2017/24764.9166
Li C, Hu D, Xue W et al (2018) Treatment outcome of combined continuous venovenous hemofiltration and hemoperfusion in acute paraquat poisoning: a prospective controlled trial. Crit Care Med 46:100–107. https://doi.org/10.1097/CCM.0000000000002826
Winchester JF (2002) Dialysis and hemoperfusion in poisoning. Adv Ren Replace Ther 9:26–30. https://doi.org/10.1053/jarr.2002.30470
Ghannoum M, Wiegand TJ, Liu KD et al (2015) Extracorporeal treatment for theophylline poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol 53:215–229. https://doi.org/10.3109/15563650.2015.1014907
Ghannoum M, Laliberté M, Nolin TD et al (2015) Extracorporeal treatment for valproic acid poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol 53:454–465. https://doi.org/10.3109/15563650.2015.1035441
Mactier R, Laliberté M, Mardini J et al (2014) Extracorporeal treatment for barbiturate poisoning: recommendations from the EXTRIP workgroup. Am J Kidney Dis 64:347–358. https://doi.org/10.1053/j.ajkd.2014.04.031
Ghannoum M, Yates C, Galvao TF et al (2014) Extracorporeal treatment for carbamazepine poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol 52:993–1004. https://doi.org/10.3109/15563650.2014.973572
Cruz DN, Perazella MA, Bellomo R et al (2007) Effectiveness of polymyxin B-immobilized fiber column in sepsis: a systematic review. Crit Care 11:1–12. https://doi.org/10.1186/cc5780
Shimizu T, Miyake T, Tani M (2017) History and current status of polymyxin B-immobilized fiber column for treatment of severe sepsis and septic shock. Ann Gastroenterol Surg 1:105–113. https://doi.org/10.1002/ags3.12015
Cruz D, Antonelli M, Fumagalli R et al (2009) Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA 301:2445–2452
Payen DM, Guilhot J, Launey Y, ABDOMIX Group et al (2015) Early use of polymyxin B hemoperfusion in patients with septic shock due to peritonitis: a multicenter randomized control trial. Intensive Care Med 41:975–984
Dellinger RP, Bagshaw SM, Antonelli M et al (2018) Effect of targeted polymyxin B hemoperfusion on 28-day mortality in patients with septic shock and elevated endotoxin level: the EUPHRATES randomized clinical trial. JAMA - J Am Med Assoc 320:1455–1463. https://doi.org/10.1001/jama.2018.14618
Klein DJ, Foster D, Walker PM et al (2018) Polymyxin B hemoperfusion in endotoxemic septic shock patients without extreme endotoxemia: a post hoc analysis of the EUPHRATES trial. Intensive Care Med 44:2205–2212. https://doi.org/10.1007/s00134-018-5463-7
Dargent A, Pais De Barros JP et al (2019) Improved quantification of plasma lipopolysaccharide (LPS) burden in sepsis using 3-hydroxy myristate (3HM): a cohort study. Intensive Care Med 45:1678–1680
Livigni S, Bertolini G, Rossi C et al (2014) Efficacy of coupled plasma filtration adsorption (CPFA) in patients with septic shock: a multicenter randomised controlled clinical trial. BMJ Open 4:e003536
Garbero E, Livigni S, Ferrari F et al (2021) High dose coupled plasma filtration and adsorption in septic shock patients. results of the COMPACT-2: a multicentre, adaptive, randomised clinical trial. Intensive Care Med 47:1303–1311
Ronco C, Bellomo R (2022) Hemoperfusion: technical aspects and state of the art. Crit Care 26:135
Köhler T, Schwier E, Praxenthaler J et al (2021) Therapeutic modulation of the host defense by hemoadsorption with cytosorb®—basics, indications and perspectives—a scoping review. Int J Mol Sci. https://doi.org/10.3390/ijms222312786
Harm S, Schildböck C, Hartmann J (2020) Cytokine removal in extracorporeal blood purification: an in vitro study. Blood Purif 49:33–43. https://doi.org/10.1159/000502680
Schädler D, Pausch C, Heise D et al (2017) The effect of a novel extracorporeal cytokine hemoadsorption device on IL-6 elimination in septic patients: a randomized controlled trial. PLoS ONE 12:1–19. https://doi.org/10.1371/journal.pone.0187015
Mat-Nor MB, Ralib MDA, Abdulah NZ, Pickering JW (2016) The diagnostic ability of procalcitonin and interleukin-6 to differentiate infectious from noninfectious systemic inflammatory response syndrome and to predict mortality. J Crit Care 33:245–251. https://doi.org/10.1016/j.jcrc.2016.01.002
Scharf C, Schroeder I, Paal M et al (2021) Can the cytokine adsorber CytoSorb® help to mitigate cytokine storm and reduce mortality in critically ill patients? A propensity score matching analysis. Ann Intensive Care. https://doi.org/10.1186/s13613-021-00905-6
Kogelmann K, Hübner T, Schwameis F et al (2021) Article first evaluation of a new dynamic scoring system intended to support prescription of adjuvant cytosorb hemoadsorption therapy in patients with septic shock. J Clin Med. https://doi.org/10.3390/jcm10132939
Wendel Garcia PD, Hilty MP, Held U et al (2021) Cytokine adsorption in severe, refractory septic shock. Intensive Care Med 47:1334–1336. https://doi.org/10.1007/s00134-021-06512-0
Hakemi MS, Nassiri AA, Nobakht A et al (2022) Benefit of hemoadsorption therapy in patients suffering sepsis-associated acute kidney injury: a case series. Blood Purif. https://doi.org/10.1159/000521228
Diab M, Lehmann T, Bothe W et al (2022) cytokine hemoadsorption during cardiac surgery versus standard surgical care for infective endocarditis (REMOVE): results from a multicenter randomized controlled trial. Circulation 145:959–968
Träger K, Skrabal C, Fischer G et al (2020) Hemoadsorption treatment with CytoSorb ® in patients with extracorporeal life support therapy: a case series. Int J Artif Organsartif Organs 43:422–429
Lebreton G, Dorgham K, Quentric P, Combes A, Gorochov G, Schmidt M (2021) Longitudinal cytokine profiling in patients with severe COVID-19 on extracorporeal membrane oxygenation and hemoadsorption. Am J Respir Crit Care Med 203:1433–1435
Stockmann H, Thelen P, Stroben F et al (2022) CytoSorb rescue for COVID-19 patients with vasoplegic shock and multiple organ failure: a prospective, open-label, randomized controlled pilot study. Crit Care Med 50:964–976
Supady A, Weber E, Rieder M et al (2021) Cytokine adsorption in patients with severe COVID-19 pneumonia requiring extracorporeal membrane oxygenation (CYCOV): a single centre, open-label, randomised, controlled trial. Lancet Respir Med 9:755–762
Ostermann M, Koyner J (2022) Extracorporeal Blood Purification Is Appropriate in Critically Ill Patients with COVID-19 and Multiorgan Failure: COMMENTARY. Kidney 360(3):419–422. https://doi.org/10.34067/kid.0007382020
Supady A, Zahn T, Kuhl M et al (2022) Cytokine adsorption in patients with post-cardiac arrest syndrome after extracorporeal cardiopulmonary resuscitation (CYTER)—a single-centre, open-label, randomised, controlled trial. Resuscitation 173:169–178. https://doi.org/10.1016/j.resuscitation.2022.02.001
Kielstein JT, Zarbock A (2022) Is this the beginning of the end of cytokine adsorption? Crit Care Med 50:1026–1029
Yaroustovsky M, Abramyan M, Rogalskaya E, Komardina E (2021) Selective polymyxin hemoperfusion in complex therapy of sepsis in children after cardiac surgery. Blood Purif 50:222–229. https://doi.org/10.1159/000510126
Bottari G, Lorenzetti G, Severini F et al (2021) Role of hemoperfusion with CytoSorb associated with continuous kidney replacement therapy on renal outcome in critically iii children with septic shock. Front Pediatr 9:1–9. https://doi.org/10.3389/fped.2021.718049
Bottari G, Murciano M, Merli P et al (2021) Hemoperfusion with CytoSorb to manage multiorgan dysfunction in the spectrum of hemophagocytic lymphohistiocytosis syndrome in critically ill children. Blood Purif. https://doi.org/10.1159/000517471
Steurer LM, Schlager G, Sadeghi K et al (2021) Hemadsorption as rescue therapy for patients with multisystem organ failure in pediatric intensive care—report of two cases reports and review of the literature. Artif Organs 45:1582–1593. https://doi.org/10.1111/aor.14047
Scharf C, Liebchen U, Paal M et al (2021) Successful elimination of bilirubin in critically ill patients with acute liver dysfunction using a cytokine adsorber and albumin dialysis: a pilot study. Sci Rep 11:1–7. https://doi.org/10.1038/s41598-021-89712-4
Ocskay K, Tomescu D, Faltlhauser A et al (2021) Hemoadsorption in ‘liver indication’—analysis of 109 patients’ data from the cytosorb international registry. J Clin Med 10:1–10. https://doi.org/10.3390/jcm10215182
Scharf C, Liebchen U, Paal M et al (2021) Blood purification with a cytokine adsorber for the elimination of myoglobin in critically ill patients with severe rhabdomyolysis. Crit Care 25:1–9. https://doi.org/10.1186/s13054-021-03468-x
Moresco E, Rugg C, Ströhle M, Thoma M (2022) Rapid reduction of substantially increased myoglobin and creatine kinase levels using a hemoadsorption device (CytoSorb ® )—a case report. Clin Case Rep 10:1–4. https://doi.org/10.1002/ccr3.5272
Pomarè Montin D, Ankawi G, Lorenzin A et al (2018) Biocompatibility and cytotoxic evaluation of new sorbent cartridges for blood hemoperfusion. Blood Purif 46:187–195. https://doi.org/10.1159/000489921
Huang Z, Wand S, Yang Z, Liu J (2013) Effect on extrapulmonary sepsis-induced acute lung injury by hemoperfusion with neutral microporous resin column. Ther Apher Dial 17:454–461
Chu L, Li G, Yu Y et al (2020) Clinical effects of hemoperfusion combined with pulse high-volume hemofiltration on septic shock. Medicine 99:e19058
Lei Y, Liang Y, Zhang X et al (2021) Alternating therapeutic plasma exchange (TPE) with double plasma molecular adsorption system (DPMAS) for the treatment of fulminant hepatic failure (FHF). Clin Case Rep 9(12):e05220
Wu M, Zhang H, Huang Y, Wu W, Huang J, Yan D (2021) Efficiency of double plasma molecular absorption system on the acute severe cholestatic hepatitis. Blood Purif 50:876–882
Schmidt JJ, Borchina DN, van’t Klooster M et al (2022) Interim analysis of the COSA (COVID-19 patients treated with the Seraph® 100 Microbind® Affinity filter) registry. Nephrol Dial Transplant 37:673–680
Seffer MT, Cottam D, Forni LG, Kielstein JT (2021) Heparin 2.0: a new approach to the infection crisis. Blood Purif 50:28–34. https://doi.org/10.1159/000508647
Goetz G, Hawlik K, Wild C (2021) Extracorporeal cytokine adsorption therapy as a preventive measure in cardiac surgery and as a therapeutic add-on treatment in sepsis: an updated systematic review of comparative efficacy and safety. Crit Care Med 49:1347–1357
Reiter K, Bordoni Dall’Olio VG, Ricatti MG, Soli M, Ruperti S et al (2002) In vitro removal of therapeutic drugs with a novel adsorbent system. Blood Purif 20:380–388
Konig C, Rohr AC, Frey OR, Brinkmann A, Roberts JA, Wichmann D et al (2019) In vitro removal of anti-infective agents by a novel cytokine adsorbent system. Int J Artif Org 42:57–64
Scharf C et al (2022) Does the cytokine adsorber CytoSorb® reduce vancomycin exposure in critically ill patients with sepsis or septic shock? a prospective observational study. Ann Intensive Care 12:44
Schneider AG et al (2021) Pharmacokinetics of anti-infective agents during CytoSorb hemoadsorption. Sci Rep 11(1):10493. https://doi.org/10.1038/s41598-021-89965-z
Biever P et al (2021) Hemoadsorption eliminates remdesivir from the circulation: Implications for the treatment of COVID-19. Pharmacol Res Perspect 9(2):e00743. https://doi.org/10.1002/prp2.743
Angheloiu AA, Angheloiu GO (2019) Removal of dabigatran using sorbent hemadsorption. Int J Cardiol 293:73–75
Schultz P, Schwier E, Eickmeyer C et al (2021) High-dose CytoSorb hemoadsorption is associated with improved survival in patients with septic shock: a retrospective cohort study. J Crit Care 64:184–192. https://doi.org/10.1016/j.jcrc.2021.04.011
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
ZR declares he received grants from BBraun. SR declares he received grants from Baxter an BBraun. TR has received funding for lectures, and been consultant or advisory board member for AstraZeneca, BBraun, Baxter, bioMérieux, Contatti Medical (CytoSorbents), Eurofarma, Jafron, Life Pharma, and Nova Biomedical. RB has received unrestricted research grants to investigate drug clearance with hemoperfusion and payment for advisory committee work by Jafron Biomedical Co Ltd. CR has been receiving honoraria, grants for studies or has been part of the advisory board and speaker bureau of the following companies in the last 3 years: Astute medical, Aferetica, Astrazeneca, Asahi Medical, Biomerieux, Baxter, Cytosorbents, Fresenius Medical Care, GE, ESTOR, Jafron, Medica, Medtronic, Novartis, Toray.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ricci, Z., Romagnoli, S., Reis, T. et al. Hemoperfusion in the intensive care unit. Intensive Care Med 48, 1397–1408 (2022). https://doi.org/10.1007/s00134-022-06810-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-022-06810-1