Abstract
Purpose
Epidemiologic studies have documented lower rates of active smokers compared to former or non-smokers in symptomatic patients affected by coronavirus disease 2019 (COVID-19). We assessed the efficacy and safety of nicotine administered by a transdermal patch in critically ill patients with COVID-19 pneumonia.
Methods
In this multicentre, double-blind, placebo-controlled trial conducted in 18 intensive care units in France, we randomly assigned adult patients (non-smokers, non-vapers or who had quit smoking/vaping for at least 12 months) with proven COVID-19 pneumonia receiving invasive mechanical ventilation for up to 72 h to receive transdermal patches containing either nicotine at a daily dose of 14 mg or placebo until 48 h following successful weaning from mechanical ventilation or for a maximum of 30 days, followed by 3-week dose tapering by 3.5 mg per week. Randomization was stratified by centre, non- or former smoker status and Sequential Organ Function Assessment score (< or ≥ 7). The primary outcome was day-28 mortality. Main prespecified secondary outcomes included 60-day mortality, time to successful extubation, days alive and free from mechanical ventilation, renal replacement therapy, vasopressor support or organ failure at day 28.
Results
Between November 6th 2020, and April 2nd 2021, 220 patients were randomized from 18 active recruiting centers. After excluding 2 patients who withdrew consent, 218 patients (152 [70%] men) were included in the analysis: 106 patients to the nicotine group and 112 to the placebo group. Day-28 mortality did not differ between the two groups (30 [28%] of 106 patients in the nicotine group vs 31 [28%] of 112 patients in the placebo group; odds ratio 1.03 [95% confidence interval, CI 0.57–1.87]; p = 0.46). The median number of day-28 ventilator-free days was 0 (IQR 0–14) in the nicotine group and 0 (0–13) in the placebo group (with a difference estimate between the medians of 0 [95% CI -3–7]). Adverse events likely related to nicotine were rare (3%) and similar between the two groups.
Conclusion
In patients having developed severe COVID-19 pneumonia requiring invasive mechanical ventilation, transdermal nicotine did not significantly reduce day-28 mortality. There is no indication to use nicotine in this situation.
Similar content being viewed by others
Early epidemiologic studies documented lower rates of active smokers compared to former or non-smokers in symptomatic patients affected by coronavirus disease 2019 (COVID-19). It was hypothesized that nicotine may interact with SARS-CoV-2 entry in human cells by downregulating the expression of angiotensin converting enzyme 2, and might mitigate the inflammatory response induced by the virus through activation of the nicotinic cholinergic system. This multicentre, randomized, double-blind, placebo-controlled trial aimed to determine the efficacy and safety of nicotine administered by a transdermal patch in critically ill patients with COVID-19 pneumonia who were receiving invasive mechanical ventilation. The results show that transdermal nicotine did not significantly reduce day-28 mortality. 60-Day mortality, time to successful extubation, days alive and free from mechanical ventilation, renal replacement therapy, vasopressor support or organ failure were also not modified by nicotine. |
Introduction
The world population remains at risk for coronavirus disease 2019 (COVID-19), especially with the emergence of genetic variants of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with increase in transmissibility, potential for more severe disease and significant reduction in neutralization by antibodies generated during previous infection or vaccination [1, 2]. Thus, there is still an urgent need for effective, easy-to-use and safe medications for patients who develop severe forms of COVID-19.
Early epidemiologic studies documented lower rates of active smokers compared to former or non-smokers in symptomatic COVID-19 patients [3,4,5,6,7,8,9], although more severe forms of the disease were reported among smokers or former smokers once infected [10, 11]. It was hypothesized that nicotine may interact with SARS-CoV-2 entry in human cells by downregulating the expression of angiotensin converting enzyme 2 (ACE2), the principal receptor for the virus [12,13,14,15]. SARS-CoV-2 may also interact with the nicotinic cholinergic system, particularly with α7 nicotinic acetylcholine receptors (nAChRs), leading to an increased inflammatory response that might be mitigated by nicotine, a competitive agonist of these receptors [14, 16,17,18,19,20]. Nicotine may likewise mediate cholinergic anti-inflammatory effects by decreasing pro-inflammatory cytokine production through the activation of nAChRs, which are expressed on human bronchial epithelial and endothelial cells, macrophages and other immune cells [14, 15, 17, 18, 20]. Favourable effects of nicotine have indeed been reported in inflammatory syndromes such as Behcet’s disease or ulcerative colitis [21].
We designed a multicentre, randomized, double-blind, placebo-controlled trial to determine the efficacy and safety of nicotine administered by a transdermal patch in critically ill patients with COVID-19 pneumonia who were receiving invasive mechanical ventilation.
Methods
Trial design and oversight
This multicentre, double-blind, placebo-controlled randomized trial was sponsored by the Direction de la Recherche Clinique et de l’innovation (DRCI), Assistance Publique—Hôpitaux de Paris, France, with a research grant from the French Ministry of Health (Programme Hospitalier de Recherche Clinique, PHRC). An independent data and safety monitoring committee periodically reviewed trial outcomes. The members of the writing committee wrote all drafts of the manuscript. All authors approved the final version of the manuscript, and agreed to submit it for publication. They also verified the data and vouched for the completeness of the data, the accuracy of the analyses, and the fidelity of the trial to the protocol.
Pierre Fabre (Paris, France) provided nicotine patches (Nicopatchlib®). Neither Pierre Fabre nor the study sponsors participated in the study design, data collection, analysis and interpretation, or in the writing or submission of the study report. Additional information is provided in the Supplementary Appendix.
Ethical aspects
The study protocol was approved by the independent ethics committees (Comité de Protection des Personnes CPP SUD-EST VI, Clermont-Ferrand, on September 28 2020, #AU 1650) and the competent French Health Authorities (Agence Nationale de Sécurité du Médicament et des Produits de Santé, ANSM, on October 2 2020, #EudraCT 2020-003723-42). Informed consent was obtained from a close relative or surrogate prior to inclusion. In accordance with French law, when such a person was absent, the patient was randomized using deferred consent whereby the patient was asked to give consent for continuation of the trial when his/her condition allowed. The trial was registered on October 22, 2020, before the inclusion of the first patient at Clinicaltrials.gov (identifier# NCT04598594).
Patients
Patients were eligible for enrolment if they were endotracheally intubated and receiving ventilation for < 72 h, had proven COVID-19 infection and were non-smokers, non-vapers or had quit smoking/vaping for at least 12 months.
Exclusion criteria were age < 18 years; anticipated duration of mechanical ventilation ≤ 48 h; pregnant or lactating women; long-term chronic respiratory insufficiency with baseline PaCO2 > 60 mmHg or treated with oxygen therapy or non-invasive ventilation, with the exception of CPAP/BiPAP for sleep apnoea; malignancy or severe disease with life expectancy < 1 year; patient moribund on the day of randomization or with a Simplified Acute Physiology Score [22] (SAPS II) > 90; cerebral deficiency with dilated areactive pupils or irreversible neurological pathology. Other exclusion criteria are reported in the Supplement.
Trial procedures
Randomization was stratified by centre, smoker status (former or non-smoker) and Sequential Organ Function Assessment (SOFA) score (< or ≥ 7). Allocation concealment was assured through a centralized, secure, Web-based randomization system.
Patients received transdermal patches containing either nicotine at a daily dose of 14 mg (determined after an extensive review of the literature of the use of transdermal nicotine in non- or former smokers [16]) or placebo until 48 h following successful weaning from mechanical ventilation or for a maximum of 30 days, followed by 3-week dose tapering by 3.5 mg per week. The study protocol provided guidance for drug adjustment or cessation in case of suggestive signs of overdose, adverse events or the occurrence of severe renal or hepatic failure. Treatments for smoking cessation such as varenicline, bupropion or other nicotine substitute were not permitted. All the patients were treated according to local [24] and international standards [25] of care for COVID-19, which included dexamethasone, antibiotic agents, anticoagulants, remdesivir and tocilizumab, as appropriate. Patients were assessed daily while hospitalized in the intensive care unit. Follow-up visits occurred on days 28 and 60 post-randomization and 2 and 8 weeks after the first day of nicotine tapering. Prespecified reasons for permanent discontinuation of the trial intervention are described in the protocol.
Endpoints
The primary endpoint was day-28 mortality. Other endpoints included mortality at day 60; time to successful extubation, i.e. without reintubation or death in the following 48 h and for tracheotomized patients, alive and not ventilated for 48 h (with death and therapeutic limitations as competitive risks); the number of ventilator-free days between inclusion and day 28, defined as the number of days alive and free from mechanical ventilation (patients were only considered as free from mechanical ventilation if they had a successful extubation, defined as being free from mechanical ventilation for at least 48 consecutive hours and non-survivors were considered to have no ventilator-free days). Other secondary endpoints, safety outcomes related to nicotine use and health-related quality of life outcomes are detailed in the Supplement.
Statistical analysis
The expected 28-day mortality rate was 35% for the placebo group [27, 28]; to demonstrate a decrease to 20% for those receiving nicotine, for 80% power and one-sided α = 0.05, 110 participants per group had to be included. A non-binding futility analysis was planned after 50% of inclusions to stop recruitment if the probability of showing a difference in 28-day mortality greater than 15 points at the final analysis was less than 10%. Alpha and beta spending were low so no sample size inflation was needed. The futility analysis was not performed because inclusion rate was faster than expected and almost all patients were randomized before futility analysis results.
Baseline characteristics are reported as proportions (%) for categorical variables and as means (± standard deviations, SD) or medians (interquartile range, IQR) for continuous variables, as appropriate. Efficacy endpoints were analysed according to intention-to-treat principles. Safety endpoints were analysed in all patients who received at least one transdermal patch. The primary endpoint of death at day 28 was compared with the chi-square test. The ranked composite score incorporating death and days free from mechanical ventilation among survivors through day 60 were compared using Mann–Whitney test and measured with net benefit (see appendix pp 9) [30]. Two planned sensitivity analyses were performed: the first used logistic regression analysis to adjust for stratification parameters, the second regarded the per-protocol population (excluding patients receiving treatment for less than 72 h). Pre-specified subgroup analyses were also conducted (see the Supplement).
Analyses were conducted at the one-sided α risk of 5% for the primary outcome and the two-sided α risk of 5% for all other outcomes. All analyses were performed using R software (R Foundation for Statistical Computing, Vienna, Austria), version 3.5.1.
Results
Study population
Between November 6th 2020 and April 2nd 2021, 220 patients were randomized from 18 active recruiting centres. After excluding 2 patients who withdrew consent, 218 patients (152 [70%] men) were included in the analysis: 106 patients to the nicotine group and 112 to the placebo group (Fig. 1). In the placebo group, one patient did not receive the transdermal treatment and another died within less than 72 h after randomization. Baseline demographic and disease characteristics were similar between groups (Table 1). The mean (SD) age was 60 ± 12 years in the nicotine group and 62 ± 12 years in the placebo group. The mean time between symptom onset and initiation of invasive mechanical ventilation was 10 ± 5 days in both groups. The comorbidities, severity of critical illness and acute respiratory distress syndrome (ARDS) were similar between the two groups, as indicated by the absence of difference for the SAPS II and SOFA scores, vasopressor support, lung compliance, and PaO2/FiO2 ratio on admission to the intensive care unit (ICU) (Table 1). The ventilator settings did not differ between the two groups, nor did the use of corticosteroids, angiotensin conversion enzyme inhibitors or angiotensin receptor blockers and tocilizumab (Table 1). There was no missing data for the primary endpoint and very few for secondary endpoints (Table S1 in the Supplement).
Primary endpoint
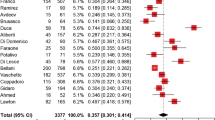
The mortality rate at day 28 in the intention-to-treat population did not differ between the two groups (30 [28%] of 106 patients in the nicotine group vs 31 [28%] of 112 patients in the placebo group; odds ratio 1.03 [95% confidence interval, CI, 0.57–1.87]; p = 0.459; Table 2, Fig. 2). Adjusting for stratification parameters did not change this result (odds ratio, 1.01 [95% CI 0.54–1.89], p = 0.973). The per-protocol sensitivity analysis (odds ratio 1.03 [95% CI 0.56–1.87], p = 0.466) and the pre-specified subgroup analyses (Fig. 3) were consistent with the main result and did not show any beneficial effect of nicotine. Noticeably, no difference in nicotine effect existed for patients included before or after Feb 17th, 2021, when the median number of patients enrolled in the trial was reached and a few days before the alpha variant of SARS-CoV-2 became dominant in France.
Secondary endpoints
The ranked composite endpoint, incorporating death and days free from mechanical ventilation through day 60, was not significantly different between treatment groups (table S1 in the Supplement). The median number of ventilator-free days at day 28 was 0 (IQR 0–14) in the nicotine group and 0 (0–12) in the placebo group (with a difference estimate between the medians of 0 [95% CI − 2–7; Table 2, figure S2 in the Supplement). The median numbers of vasopressor- and renal failure-free days and the number of patients supported by extracorporeal membrane oxygenation (ECMO) during the ICU stay were not different between the 2 groups. The rate of extubated patients at day 28, the time to successful extubation (figure S3, in the Supplement) and the median duration of invasive mechanical ventilation, length of intensive care unit and hospital stays were also similar between the two groups (Table 2).
Safety endpoints
The median number of days under nicotine in the ICU was 18 [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29] with a median daily dose of 14 mg (IQR 14–14). Nicotine was tapered over 19 [10,11,12,13,14,15,16,17,18,19,20,21] days. The number of adverse events related to nicotine was low (3%) and similar between the two groups (Table 3). There was no difference in the occurrence of ventilator-acquired pneumonia, bacteraemia, pneumothorax, need for renal replacement therapy and thromboembolism between the two groups (Table 3).
Follow-up at weeks 2 and 8 after initiation of nicotine tapering was available for 93 and 100 patients. No patient reported smoking, vaping or taking nicotine substitutes. The scores of desire to smoke, and nicotine withdrawal symptoms were not different between groups, as were the scores evaluating anxiety, depression, PTSD symptoms and insomnia (table S2, appendix p 13–14).
Discussion
In this randomized, double-blind, placebo-controlled phase 3, clinical trial involving hospitalized patients with COVID-19 pneumonia receiving invasive mechanical ventilation, transdermal nicotine did not significantly reduce mortality at day 28. No significant difference existed in any secondary outcomes evaluated, including mortality at day 60, durations of invasive mechanical ventilation, renal and cardiovascular failures, ICU and hospital stays.
The “nicotine hypothesis” linking lower than expected COVID-19 cases among active smokers to putative preventive and therapeutic effects of nicotine against SARS-CoV-2 emerged early in the course of the pandemic [3]. In the weeks following the pre-print publication of these data, social media platforms like Twitter relayed thousands of messages about the benefits of smoking or vaping in the context of COVID-19 [31, 32]. However, the effects of nicotine and cigarette smoke on SARS-CoV-2 replication and the expression of its entry receptor ACE2 remain highly controversial with recent reports of both increased [33, 34] and decreased [35] ACE2 levels. Alternatively, cumulative smoking exposure (in former or current smokers) was constantly associated with worse outcomes for COVID-19 [11, 36,37,38].
Our results demonstrate the absence of effect of nicotine in patients who had developed the most severe forms of COVID-19 pneumonia requiring invasive mechanical ventilation. Demographics, disease progression, and severity markers of our patients were in line with those of previous cohorts of mechanically ventilated COVID-19 ARDS. The 36% mortality rate at day 60 we observed is similar to that reported in the large epidemiologic French COVID-ICU cohort [27] (March to July 2020) and the ICAR randomized trial [39] (April to October 2020) evaluating intravenous immunoglobulins in COVID-19 mechanically ventilated patients, but lower than that of other large European cohorts [28, 40, 41]. It should however be noted that the SAPS II [39] and SOFA [27] scores were higher in our patients, as were the rate of patients on vasopressor [27] and ECMO [27, 41, 42] support at randomization. The trajectory of our patient during ICU stay was also similar to other recent cohorts [28, 40, 41], with long ICU and hospital stays and frequent ventilator-associated pneumonia. Reassuringly, adverse events related to nicotine patches were rare and no sign of nicotine addiction was reported in the 8 weeks following ICU discharge.
Our trial has several limitations. First, the day 28 mortality we observed was lower that the hypothesis we had made based on preliminary data on COVID-19 patients’ outcomes [27, 28, 43]. However, the complete absence of difference between the outcomes of nicotine- and placebo-treated patients argue against any effect of the molecule in this context. Second, the study was conducted when the original SARS-CoV-2 virus and its alpha variant were dominant in France. Still, our results can be extended to the latest delta and omicron variants, for which virus entry into cells and pathophysiological mechanisms of the disease has not changed. Third, we did not include current smokers in this trial. Although it may be speculated that an acute deprivation of nicotine in smokers may be associated with worse outcomes in COVID-19 patients (for example, due to an acute upregulation of ACE2 and increased secretion of proinflammatory cytokines) that may be reversed by nicotine replacement therapy, including current smokers may have introduced a major bias in the interpretation of the impact of nicotine in severe COVID-19. Additionally, nicotine replacement therapy is sometimes recommended in ICU patients to prevent withdrawal syndrome [44]. Fourth, we cannot exclude a preventive effect of nicotine, if administered earlier, on contamination by SARS-CoV-2 or on the progression to severe forms of the disease. Pertinently, the effect of remdesivir [45] administered very early after symptoms onset was associated with a larger clinical benefit than if given to patients already hospitalized for severe forms. Fourth, although transdermal nicotine has been used successfully in other populations of ICU patients [44, 46], we cannot exclude inconstant absorption of the drug, especially in septic patients treated with vasopressors and having subcutaneous vasoconstriction and oedema. Inhalation of nicotine or its administration through an oral or nasal spray may potentially be more effective. Lastly, further research is urgently needed to find drugs or strategies for patients who have developed the most severe forms of COVID-19 requiring mechanically ventilation, since, as of today, only corticosteroids [47, 48] administered after hospitalization significantly improved the survival of these patients.
In conclusion, this randomized trial showed that transdermal nicotine did not significantly improve the outcomes of patients having developed severe COVID-19 pneumonia requiring invasive mechanical ventilation. Therefore, there is no indication to use nicotine in this situation.
Abbreviations
- ACE2:
-
Angiotensin converting enzyme 2
- nAChRs:
-
Nicotinic acetylcholine receptors
- ARDS:
-
Acute respiratory distress syndrome
- ICU:
-
Intensive care unit
- MV:
-
Mechanical ventilation
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus-2
References
Centers for Disease Control and Prevention: SARS-CoV-2 Variant Classifications and Definitionshttps://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html#Concern; Last accessed, January 1st, 2022
Del Rio C, Omer SB, Malani PN (2021) Winter of omicron-the evolving COVID-19 pandemic. JAMA 2:2
Miyara M, Tubach F, Pourcher V et al (2022) Low rate of daily smokers in patients with symptomatic COVID-19: a monocentric self-report of smoking habit study. Front Med. https://doi.org/10.3389/fmed.2021.668995
Farsalinos K, Barbouni A, Niaura R (2020) Systematic review of the prevalence of current smoking among hospitalized COVID-19 patients in China: could nicotine be a therapeutic option? Intern Emerg Med 15:845–852
Guan WJ, Ni ZY, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708–1720
Simons D, Shahab L, Brown J et al (2021) The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction (Abingdon, England) 116:1319–1368
Fontanet A, Tondeur L, Grant R, et al. (2021) SARS-CoV-2 infection in schools in a northern French city: a retrospective serological cohort study in an area of high transmission, France, January to April 2020. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin 26
Paleiron N, Mayet A, Marbac V et al (2021) Impact of tobacco smoking on the risk of COVID-19: a large scale retrospective cohort study. Nicotine Tobacco Res 23:1398–1404
González-Rubio J, Navarro-López C, López-Nájera E et al (2020) A systematic review and meta-analysis of hospitalised current smokers and COVID-19. Int J Environ Res Public Health 17:2
Reddy RK, Charles WN, Sklavounos A et al (2021) The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol 93:1045–1056
Lowe KE, Zein J, Hatipoglu U et al (2021) Association of smoking and cumulative pack-year exposure with COVID-19 outcomes in the cleveland clinic COVID-19 registry. JAMA Intern Med 181:709–711
Yan R, Zhang Y, Li Y et al (2020) Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 367:1444–1448
Oakes JM, Fuchs RM, Gardner JD et al (2018) Nicotine and the renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol 315:R895-r906
Changeux JP, Amoura Z, Rey FA et al (2020) A nicotinic hypothesis for Covid-19 with preventive and therapeutic implications. CR Biol 343:33–39
Tizabi Y, Getachew B, Copeland RL et al (2020) Nicotine and the nicotinic cholinergic system in COVID-19. FEBS J 287:3656–3663
Dautzenberg B, Levi A, Adler M et al (2021) Transdermal nicotine in non-smokers: a systematic review to design COVID-19 clinical trials. Respir Med Res 80:100844
Wang H, Yu M, Ochani M et al (2003) Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Nature 421:384–388
Fujii T, Mashimo M, Moriwaki Y et al (2017) Expression and function of the cholinergic system in immune cells. Front Immunol 8:1085
Farsalinos K, Eliopoulos E, Leonidas DD et al (2020) Nicotinic cholinergic system and COVID-19: in silico identification of an interaction between SARS-CoV-2 and nicotinic receptors with potential therapeutic targeting implications. Int J Mol Sci 21:2
Gonzalez-Rubio J, Navarro-Lopez C, Lopez-Najera E et al (2020) Cytokine release syndrome (CRS) and nicotine in COVID-19 patients: trying to calm the storm. Front Immunol 11:1359
Gomes JP, Watad A, Shoenfeld Y (2018) Nicotine and autoimmunity: The lotus’ flower in tobacco. Pharmacol Res 128:101–109
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Lameire N, Levin A, Kellum JA et al (2021) Harmonizing acute and chronic kidney disease definition and classification: report of a kidney disease: improving global outcomes (KDIGO) Consensus Conference. Kidney Int 2:2
Base documentaire de l'APHP sur la COVID-19: http://covid-documentation.aphp.fr/; Last accessed, January 1st 2022
IDSA Guidelines on the Treatment and Management of Patients with COVID-19: https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/; Last accessed, January 11st 2022
Beitler JR, Sarge T, Banner-Goodspeed VM et al (2019) Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 321:846–857
(2021) COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators, Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med 47: 60–73
Grasselli G, Zangrillo A, Zanella A et al (2020) Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 323:1574–1581
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Buyse M (2010) Generalized pairwise comparisons of prioritized outcomes in the two-sample problem. Stat Med 29:3245–3257
Kamiński M, Muth A, Bogdański P (2020) Smoking, vaping, and tobacco industry during COVID-19 pandemic: twitter data analysis. Cyberpsychol Behav Soc Netw 23:811–817
Kavuluru R, Noh J, Rose SW (2021) Twitter discourse on nicotine as potential prophylactic or therapeutic for COVID-19. Int J Drug Policy 99:103470
Ghosh A, Girish V, Yuan ML et al (2021) Combustible and electronic cigarette exposures increase ACE2 activity and SARS-CoV-2 spike binding. Am J Respir Crit Care Med 2:2
Masso-Silva JA, Moshensky A, Shin J et al (2021) Chronic E-cigarette aerosol inhalation alters the immune state of the lungs and increases ACE2 expression, raising concern for altered response and susceptibility to SARS-CoV-2. Front Physiol 12:649604
Tomchaney M, Contoli M, Mayo J et al (2021) Paradoxical effects of cigarette smoke and COPD on SARS-CoV-2 infection and disease. BMC Pulm Med 21:275
Hopkinson NS, Rossi N, El-Sayed Moustafa J et al (2021) Current smoking and COVID-19 risk: results from a population symptom app in over 2.4 million people. Thorax 76:714–722
Ioannou GN, Locke E, Green P et al (2020) Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US veterans with SARS-CoV-2 infection. JAMA Netw Open 3:e2022310
Razjouyan J, Helmer DA, Lynch KE et al (2021) Smoking status and factors associated with COVID-19 in-hospital mortality among US veterans. Nicotine Tobacco Res 2:2
Mazeraud A, Jamme M, Mancusi RL, et al., (2021) Intravenous immunoglobulins in patients with COVID-19-associated moderate-to-severe acute respiratory distress syndrome (ICAR): multicentre, double-blind, placebo-controlled, phase 3 trial. Lancet Respir Med
Karagiannidis C, Mostert C, Hentschker C et al (2020) Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med 8:853–862
Patel BV, Haar S, Handslip R et al (2021) Natural history, trajectory, and management of mechanically ventilated COVID-19 patients in the United Kingdom. Intensive Care Med 47:549–565
Schmidt M, Hajage D, Lebreton G et al (2020) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med 8:1121–1131
Yang X, Yu Y, Xu J et al (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8:475–481
de Jong B, Schuppers AS, Kruisdijk-Gerritsen A et al (2018) The safety and efficacy of nicotine replacement therapy in the intensive care unit: a randomised controlled pilot study. Ann Intensive Care 8:70
Gottlieb RL, Vaca CE, Paredes R et al (2021) Early remdesivir to prevent progression to severe Covid-19 in outpatients. N Engl J Med 2:2
Gillies MA, McKenzie CA, Whiteley C et al (2012) Safety of nicotine replacement therapy in critically ill smokers: a retrospective cohort study. Intensive Care Med 38:1683–1688
Angus DC, Derde L, Al-Beidh F et al (2020) Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA 324:1317–1329
Horby P, Lim WS, Emberson JR et al (2021) Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 384:693–704
Acknowledgements
List of the NICOVID-REA Trial Group members: Jessica Palmyre: URC PSL-CFX, Pitié Salpêtrière, 47/83 Bd de l’Hôpital, Paris, France. Linda Gimeno: URC PSL-CFX, Pitié Salpêtrière, 47/83 Bd de l’Hôpital, Paris, France. Assitan Kone: URC PSL-CFX, Pitié Salpêtrière, 47/83 Bd de l’Hôpital, Paris, France. Cedric Vialette: URC PSL-CFX, Pitié Salpêtrière, 47/83 Bd de l’Hôpital, Paris, France. Ouramdane Slimi: URC PSL-CFX, Pitié Salpêtrière, 47/83 Bd de l’Hôpital, Paris, France. Juliette Chommeloux: Service de médecine intensive-réanimation, Institut de Cardiologie, APHP Hôpital Pitié–Salpêtrière, F-75013 PARIS, France; Sorbonne Université, INSERM, UMRS_1166-ICAN, Institute of Cardiometabolism and Nutrition, F-75013 PARIS, France. Lucie Lefevre: Service de médecine intensive-réanimation, Institut de Cardiologie, APHP Hôpital Pitié–Salpêtrière, F-75013 PARIS, France; Sorbonne Université, INSERM, UMRS_1166-ICAN, Institute of Cardiometabolism and Nutrition, F-75013 PARIS, France. Matthieu Schmidt: Service de médecine intensive-réanimation, Institut de Cardiologie, APHP Hôpital Pitié–Salpêtrière, F-75013 PARIS, France; Sorbonne Université, INSERM, UMRS_1166-ICAN, Institute of Cardiometabolism and Nutrition, F-75013 PARIS, France. Guillaume Hekimian: Service de médecine intensive-réanimation, Institut de Cardiologie, APHP Hôpital Pitié–Salpêtrière, F-75013 PARIS, France; Sorbonne Université, INSERM, UMRS_1166-ICAN, Institute of Cardiometabolism and Nutrition, F-75013 PARIS, France. Charles-Edouard Luyt: Service de médecine intensive-réanimation, Institut de Cardiologie, APHP Hôpital Pitié–Salpêtrière, F-75013 PARIS, France; Sorbonne Université, INSERM, UMRS_1166-ICAN, Institute of Cardiometabolism and Nutrition, F-75013 PARIS, France. Laure Stiel: Service de Médecin Intensive-Réanimation, Groupement Hospitalier Régional, Mulhouse et Sud Alsace. Anne-Florence Dureau: Service de Médecin Intensive-Réanimation, Groupement Hospitalier Régional, Mulhouse et Sud Alsace. Kuteifan Khaldoun: Service de Médecin Intensive-Réanimation, Groupement Hospitalier Régional, Mulhouse et Sud Alsace. Hanna Eid: Service de Médecin Intensive-Réanimation, Groupement Hospitalier Régional, Mulhouse et Sud Alsace. Matthieu Baldacini: Service de Médecin Intensive-Réanimation, Groupement Hospitalier Régional, Mulhouse et Sud Alsace. Cecile Zyberfajn: Centre Hospitalier René Dubos PONTOISE, 6, avenue de l’Ile de France. Julien Manson: Centre Hospitalier René Dubos PONTOISE, 6, avenue de l’Ile de France. Nathanael Charrier: Centre Hospitalier René Dubos PONTOISE, 6, avenue de l’Ile de France. Angelique Balabanian: Centre Hospitalier René Dubos PONTOISE, 6, avenue de l’Ile de France. Damien Contou: Service de réanimation, Centre Hospitalier Victor Dupouy, 69 rue du Lieutenant-Colonel Prud'hon, 95107 Argenteuil Cedex. Olivier Pajot: Service de réanimation, Centre Hospitalier Victor Dupouy, 69 rue du Lieutenant-Colonel Prud'hon, 95107 Argenteuil Cedex. Megan Fraisse: Service de réanimation, Centre Hospitalier Victor Dupouy, 69 rue du Lieutenant-Colonel Prud'hon, 95107 Argenteuil Cedex. Paul Desaint: Service de réanimation, Centre Hospitalier Victor Dupouy, 69 rue du Lieutenant-Colonel Prud'hon, 95107 Argenteuil Cedex. Florence Sarfati: Service de réanimation, Centre Hospitalier Victor Dupouy, 69 rue du Lieutenant-Colonel Prud'hon, 95107 Argenteuil Cedex. Muriel Fartoukh: Sorbonne Université, Assistance Publique—Hôpitaux de Paris, Service de Médecine Intensive Réanimation, Hôpital Tenon, 4, Rue de la Chine, 75020 Paris. Guillaume Voirot: Sorbonne Université, Assistance Publique—Hôpitaux de Paris, Service de Médecine Intensive Réanimation, Hôpital Tenon, 4, Rue de la Chine, 75020 Paris. Alexandre Elabbabi: Sorbonne Université, Assistance Publique—Hôpitaux de Paris, Service de Médecine Intensive Réanimation, Hôpital Tenon, 4, Rue de la Chine, 75020 Paris. Michel Djibre: Sorbonne Université, Assistance Publique—Hôpitaux de Paris, Service de Médecine Intensive Réanimation, Hôpital Tenon, 4, Rue de la Chine, 75020 Paris. Cyrielle Desnos: Sorbonne Université, Assistance Publique—Hôpitaux de Paris, Service de Médecine Intensive Réanimation, Hôpital Tenon, 4, Rue de la Chine, 75020 Paris. Pierre Garcon: Service de Réanimation Polyvalente, Grand Hôpital de l’Est Francilien, site de Marne-La-Vallée, 2-4 cours de la Gondoire 77600 Jossigny. Ly van Vong: Service de Réanimation Polyvalente, Grand Hôpital de l’Est Francilien, site de Marne-La-Vallée, 2-4 cours de la Gondoire 77600 Jossigny. Andrea Issad: Service de Réanimation Polyvalente, Grand Hôpital de l’Est Francilien, site de Marne-La-Vallée, 2-4 cours de la Gondoire 77600 Jossigny. Bertrand Pillot: Service de Réanimation Polyvalente, Grand Hôpital de l’Est Francilien, site de Marne-La-Vallée, 2-4 cours de la Gondoire 77600 Jossigny. Delphine Reither: Service de Réanimation Polyvalente, Grand Hôpital de l’Est Francilien, site de Marne-La-Vallée, 2-4 cours de la Gondoire 77600 Jossigny. Patrick Rouge: Hôpital Simone Veil Eaubonne, 14 Rue Saint prix, Hôpital Simone Veil, 95 600 Eaubonne. Pascale Foliot: Hôpital Simone Veil Eaubonne, 14 Rue Saint prix, Hôpital Simone Veil, 95 600 Eaubonne. Lynda Bendjamar: Hôpital Simone Veil Eaubonne, 14 Rue Saint prix, Hôpital Simone Veil, 95 600 Eaubonne. Valentin Pointurier: Service de Réanimation Médicale, CHRU de Besançon, Boulevard Fleming. Hadrien Winiszewski: Service de Réanimation Médicale, CHRU de Besançon, Boulevard Fleming. Gilles Capellier: Service de Réanimation Médicale, CHRU de Besançon, Boulevard Fleming. Jean-Christophe Navellou: Service de Réanimation Médicale, CHRU de Besançon, Boulevard Fleming. Romain Tapponnier: Service de Réanimation Médicale, CHRU de Besançon, Boulevard Fleming. Emilie Panicucci: Médecine Intensive Réanimation, Hôpital L'Archet 1, Centre Hospitalier Universitaire de Nice, 151 route Saint Antoine de Ginestière, Nice, France. Lucas Morand: Médecine Intensive Réanimation, Hôpital L'Archet 1, Centre Hospitalier Universitaire de Nice, 151 route Saint Antoine de Ginestière, Nice, France. Jean Dellamonica: Médecine Intensive Réanimation, Hôpital L'Archet 1, Centre Hospitalier Universitaire de Nice, 151 route Saint Antoine de Ginestière, Nice, France. Clement Saccheri: Médecine Intensive Réanimation, Hôpital L'Archet 1, Centre Hospitalier Universitaire de Nice, 151 route Saint Antoine de Ginestière, Nice, France. Nicolas Weiss: Médecine Intensive Réanimation à orientation Neurologique, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Clemence Marois: Médecine Intensive Réanimation à orientation Neurologique, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Loic Le Guennec: Médecine Intensive Réanimation à orientation Neurologique, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Benjamin Rohaut: Médecine Intensive Réanimation à orientation Neurologique, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Luis Ensenat: Centre hospitalier Sud Francilien (CHSF), 40 Avenue Serge Dassault. Cecilia Billiou: Centre hospitalier Sud Francilien (CHSF), 40 Avenue Serge Dassault. Maria Aroca: Centre hospitalier Sud Francilien (CHSF), 40 Avenue Serge Dassault. Marie Baron: Centre hospitalier Sud Francilien (CHSF), 40 Avenue Serge Dassault. Alexandre Demoule: Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Médecine Intensive et Réanimation (Département R3S), AP-HP, INSERM, UMRS1158 Neurophysiologie Respiratoire Expérimentale et Clinique, Sorbonne Université, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Alexandra Beurton: Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Médecine Intensive et Réanimation (Département R3S), AP-HP, INSERM, UMRS1158 Neurophysiologie Respiratoire Expérimentale et Clinique, Sorbonne Université, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Come Bureau: Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Médecine Intensive et Réanimation (Département R3S), AP-HP, INSERM, UMRS1158 Neurophysiologie Respiratoire Expérimentale et Clinique, Sorbonne Université, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Maxens Decavele: Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Médecine Intensive et Réanimation (Département R3S), AP-HP, INSERM, UMRS1158 Neurophysiologie Respiratoire Expérimentale et Clinique, Sorbonne Université, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Martin Dres: Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Médecine Intensive et Réanimation (Département R3S), AP-HP, INSERM, UMRS1158 Neurophysiologie Respiratoire Expérimentale et Clinique, Sorbonne Université, Site Pitié Salpêtrière, 47-83 bd de l’Hôpital, 75013 Paris. Frederique Bayle: Médipole Lyon Villeurbanne. Service de réanimation. 158 rue Léon Blum. 69100 VILLEURBANNE. Quoc Viet Le: Médipole Lyon Villeurbanne. Service de réanimation. 158 rue Léon Blum. 69100 VILLEURBANNE. Lionel Liron: Médipole Lyon Villeurbanne. Service de réanimation. 158 rue Léon Blum. 69100 VILLEURBANNE. Jean-Baptiste Putegnat: Médipole Lyon Villeurbanne. Service de réanimation. 158 rue Léon Blum. 69100 VILLEURBANNE. Francois Salord: Médipole Lyon Villeurbanne. Service de réanimation. 158 rue Léon Blum. 69100 VILLEURBANNE. Pascal Andreu: Department of Intensive Care, Burgundy University Hospital, Dijon, France; Lipness Team, INSERM Research Center LNC-UMR1231 and LabEx LipSTIC, University of Burgundy, Dijon, France; INSERM CIC 1432, Clinical Epidemiology, University of Burgundy, Dijon, France. Hakim Slimani: Department of Intensive Care, Burgundy University Hospital, Dijon, France; Lipness Team, INSERM Research Center LNC-UMR1231 and LabEx LipSTIC, University of Burgundy, Dijon, France; INSERM CIC 1432, Clinical Epidemiology, University of Burgundy, Dijon, France. Baptiste Roudeau: Department of Intensive Care, Burgundy University Hospital, Dijon, France; Lipness Team, INSERM Research Center LNC-UMR1231 and LabEx LipSTIC, University of Burgundy, Dijon, France; INSERM CIC 1432, Clinical Epidemiology, University of Burgundy, Dijon, France. Marie Labruyere: Department of Intensive Care, Burgundy University Hospital, Dijon, France; Lipness Team, INSERM Research Center LNC-UMR1231 and LabEx LipSTIC, University of Burgundy, Dijon, France; INSERM CIC 1432, Clinical Epidemiology, University of Burgundy, Dijon, France. Marine Jacquier: Department of Intensive Care, Burgundy University Hospital, Dijon, France; Lipness Team, INSERM Research Center LNC-UMR1231 and LabEx LipSTIC, University of Burgundy, Dijon, France; INSERM CIC 1432, Clinical Epidemiology, University of Burgundy, Dijon, France. Nadia Anguel: CHU Bicêtre, 78 Rue du Général Leclerc. Soufia Ayed: CHU Bicêtre, 78 Rue du Général Leclerc. Edgard Durand: CHU Bicêtre, 78 Rue du Général Leclerc. Laurent Guerin: CHU Bicêtre, 78 Rue du Général Leclerc. Christopher Lai: CHU Bicêtre, 78 Rue du Général Leclerc. Jerome Aboab: Service de Médecine Intensive Réanimation du Centre Hospitalier de Saint-Denis, URC—GHT Plaine de France (CHSD-CHG), 2 rue du Dr Delafontaine, 93200 SAINT DENIS. Sophie Alviset: Service de Médecine Intensive Réanimation du Centre Hospitalier de Saint-Denis, URC—GHT Plaine de France (CHSD-CHG), 2 rue du Dr Delafontaine, 93200 SAINT DENIS. Laurent Laine: Service de Médecine Intensive Réanimation du Centre Hospitalier de Saint-Denis, URC—GHT Plaine de France (CHSD-CHG), 2 rue du Dr Delafontaine, 93200 SAINT DENIS. Mathilde Azzi: Service de Médecine Intensive Réanimation du Centre Hospitalier de Saint-Denis, URC—GHT Plaine de France (CHSD-CHG), 2 rue du Dr Delafontaine, 93200 SAINT DENIS. Tazime Issoufaly: Service de Médecine Intensive Réanimation du Centre Hospitalier de Saint-Denis, URC—GHT Plaine de France (CHSD-CHG), 2 rue du Dr Delafontaine, 93200 SAINT DENIS. Laurent Tric: Institut Mutualiste Montsouris, IMM, 42 Bd Jourdan, 75014 Paris. Lyes Knani: Institut Mutualiste Montsouris, IMM, 42 Bd Jourdan, 75014 Paris. Chahrazad Bey Boumezrag: Institut Mutualiste Montsouris, IMM, 42 Bd Jourdan, 75014 Paris. Nicolas Viault: Institut Mutualiste Montsouris, IMM, 42 Bd Jourdan, 75014 Paris. Francois Barbier: Service de Médecine Intensive Réanimation, Centre Hospitalier Régional d’Orléans, CHR Orléans, 14 Avenue de l'Hôpital CS 86709, 45067 Orléans CEDEX 2, France. Thierry Boulain: Service de Médecine Intensive Réanimation, Centre Hospitalier Régional d’Orléans, CHR Orléans, 14 Avenue de l'Hôpital CS 86709, 45067 Orléans CEDEX 2, France. Toufik Kamel: Service de Médecine Intensive Réanimation, Centre Hospitalier Régional d’Orléans, CHR Orléans, 14 Avenue de l'Hôpital CS 86709, 45067 Orléans CEDEX 2, France. Mai-Anh Nay: Service de Médecine Intensive Réanimation, Centre Hospitalier Régional d’Orléans, CHR Orléans, 14 Avenue de l'Hôpital CS 86709, 45067 Orléans CEDEX 2, France. Sophie Tollec: Service de Médecine Intensive Réanimation, Centre Hospitalier Régional d’Orléans, CHR Orléans, 14 Avenue de l'Hôpital CS 86709, 45067 Orléans CEDEX 2, France, An Hung Nguyen: Unité Hospitalière d'Addictologie (ELSA), Unité de Sevrages Complexes, Hôpital Pitié Salpêtrière, APHP Sorbonne Université, Sorbonne Université, Site Pitié Salpêtrière, Bâtiment de La Force, 47-83 bd de l’Hôpital, 75013 Paris.
Funding
The trial was registered at www.clinicaltrials.gov under NCT04598594 on October 22nd 2020, before the inclusion of the first patient. The trial was sponsored in France by the Direction de la Recherche Clinique et de l’Innovation (DRCI), Assistance Publique—Hopitaux de Paris (APHP) through the Clinical Research Unit Pitié-Salpêtrière-Charles Foix, with a research grant from the French Ministry of Health (Programme Hospitalier de Recherche Clinique, PHRC). Pierre Fabre (Paris, France) provided Nicotine patches. Neither the study sponsor nor Pierre Fabre participated in the study design, data collection, analysis and interpretation, or the writing and submission of the study report.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
RG has received compensation as a member of the scientific advisory board of Janssen, Lundbeck, Roche, SOBI, Takeda. He has served as consultant and/or speaker for Astra Zeneca, Boehringer-Ingelheim, Pierre Fabre, Lilly, Lundbeck, LVMH, MAPREG, Novartis, Otsuka, Pileje, SANOFI, Servier and received compensation, and he has received research support from Servier. Co-founder and stock shareholder: Regstem. AC reported receiving grants and personal fees from Maquet, Xenios and Baxter outside the submitted work. No other disclosures were reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the COVID-REA Trial Group are listed in the Acknowledgement section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Labro, G., Tubach, F., Belin, L. et al. Nicotine patches in patients on mechanical ventilation for severe COVID-19: a randomized, double-blind, placebo-controlled, multicentre trial. Intensive Care Med 48, 876–887 (2022). https://doi.org/10.1007/s00134-022-06721-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-022-06721-1