Abstract
Purpose
Venous thromboembolism (VTE) prophylaxis is effective in reducing VTE events; however, it is underutilized in critically ill patients. We examined trends and risk factors for omission of early thromboprophylaxis within the first 24 h after admission in Australian and New Zealand intensive care units (ICUs) between 2009 and 2020.
Methods
Retrospective analysis of data from the Australian New Zealand Intensive Care Society Adult Patient Database. Data were obtained for 1,465,020 adult admissions between 2009 and 2020. Mixed effects logistic regression modeling (accounting for the random effects of the contributing ICUs) was used to identify factors associated with omission of early thromboprophylaxis.
Results
A total of 107,486 (7.3%) ICU patients did not receive any form of thromboprophylaxis within the first 24 h after ICU admission without obvious reasons. Omission of early thromboprophylaxis declined from 13.7% in 2009 to 4% in 2020 (by 70.8%) (P < 0.001). Younger patients were more like to miss out on VTE prophylaxis (odds ratios (OR)per 10-year increase 0.94, 95% CI 0.95–0.99). A documented process for monitoring VTE prophylaxis (ORs 0.90, 95% CI 0.87–0.93) and having a medical lead, dedicated for coordinating ICU quality (ORper 0.1 increase in full-time equivalent 0.97, 95% CI 0.93–0.99), are associated with less omission of VTE prophylaxis.
Conclusion
Omission of thromboprophylaxis within the first 24 h after ICU admission has declined steadily over the past decade. Documented process for monitoring VTE prophylaxis and having a medical lead for coordinating quality of ICU care could be potential targets for sustaining the improvement in VTE prophylaxis use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this study of more than 1.4 million critically ill patients, omission of thromboprophylaxis within the first 24 h after admission in intensive care unit (ICU) has declined by 70.8% between 2009 and 2020. Potentially modifiable factors, including documented process for monitoring venous thromboembolism (VTE) prophylaxis and having a medical lead for coordinating quality of ICU care could be potential targets for sustaining the improvement in VTE prophylaxis use. |
Introduction
Venous thromboembolism (VTE) which includes deep vein thrombosis (DVT) and pulmonary embolism (PE) is a major clinical and public health concern. Globally, there are about 10 million cases of VTE every year (79 to 269 per 100,000 population), and a mortality rate in untreated patients of 12–50% [1,2,3]. The incidence of VTE is even higher in intensive care unit (ICU) patients, ranging from 13 to 31%, often due to additional risk factors typically associated with ICU admission, such as sedation, immobilization, mechanical ventilation, and central venous catheters [4, 5]. VTE care also imposes a significant economic burden on patients and the healthcare system [2]. In Australia, more than 17,000 people develop VTE each year, and costs patients and the health system $1.72 billion annually [6].
The use of VTE prophylaxis reduces the risk of VTE by 50–70% in a broad range of medical or surgical patients [7,8,9]. Practice guidelines recommend that all patients should be assessed for the risk of VTE and that most should receive appropriate VTE prophylaxis within the first 24 h after ICU admission [6, 10]. Nevertheless, a significant proportion of patients at risk of VTE do not receive VTE prophylaxis as recommended in guidelines [8, 11], and there are substantial differences in VTE risk assessment and use of thromboprophylaxis [11]. A survey of 358 hospitals across 32 countries showed that, of the 52% of hospitalized patients who were at risk for VTE as per the American College of Chest Physicians (ACCP) guidelines, only 50% received the recommended VTE prophylaxis, with a range of 0–83% [11]. Delay or omission of thromboprophylaxis within the first 24 h of ICU admission without obvious reasons is associated with a significantly higher risk of VTE and mortality [12, 13]. A study of approximately 80,000 trauma patients reported that a delay of 24–48 h, and beyond 48 h in initiating VTE prophylaxis is associated with a 1.26- and 2.35-fold increased risk of VTE events, respectively [12].
Significant progress has been made in improving VTE prevention and making VTE prevention a priority in health care [9]. Standard VTE risk assessment tools and resources have been developed to reliably guide VTE prophylaxis and improve awareness and compliance with VTE prophylaxis guidelines [8, 9, 14]. Electronic alerts and decision support systems have become more common due to the use of electronic health records [15]. However, whether the proportion of omission of thromboprophylaxis within the first 24 h after ICU admission has declined over time and whether risk factors for omission of early thromboprophylaxis are amenable to intervention remain unclear.
We investigated trends in omission of thromboprophylaxis within the first 24 h after ICU admission, and identified factors associated with omission of VTE prophylaxis.
Methods
Data sources and participants
We analyzed data from the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) and Critical Care Resources survey, binational clinical quality registry datasets run by the ANZICS Centre for Outcome and Resource Evaluation (CORE).
The ANZICS APD contains data from over 2 million patient episodes collected from 203 ICUs, representing more than 90% of Australia and New Zealand ICU admissions, and is one of the largest single datasets on intensive care in the world. The ANZICS CORE participating ICUs contribute de-identified data. Each contributing ICU allows subsequent data use as appropriate, understanding procedures and in compliance with the ANZICS CORE terms of reference and with a waiver of the need for informed consent. The development and details of the ANZICS APD have been described in detail elsewhere [16].
Early thromboprophylaxis
Thromboprophylaxis status within the first 24 h of ICU admission was captured in a standard precoded response: “Yes,” “No,” “Contraindicated,” or “Not indicated.” Consistent with a previous study using the same database [13], patients who received one or more of the following methods of thromboprophylaxis, including unfractionated heparin, low molecular-weight heparin, pneumatic compression devices, compression stockings, or inferior vena cava filter, within the first 24 h after ICU admission were considered to have received early thromboprophylaxis. Omission of early thromboprophylaxis included patients who did not receive any method of thromboprophylaxis within the first 24 h after ICU admission without obvious reasons or contraindications to pharmacologic or mechanical thromboprophylaxis, as stated by their attending clinicians. Thromboprophylaxis was considered contraindicated for patients who were at risk of bleeding and had physical injuries to their lower extremities, unless an inferior vena cava filter was inserted within the first 24 h after ICU admission. Patients who did not receive any form of thromboprophylaxis within the first 24 h after ICU admission because they were assessed to have a very low risk of VTE by the attending clinical were considered as “not indicated” for early thromboprophylaxis [13]. The Acute Physiology and Chronic Health Evaluation II (APACHE II) scoring system was used to assess the severity illness.
ICU level process of care indicators
We analyzed data from annual ANZICS Critical Care Resources surveys from 2009 to 2020 to examine the relationship between ICU level processes of care indicators and use of VTE thromboprophylaxis. Participating ICUs reported process of care indicators, including documentation of VTE prophylaxis, number and type of staff available for ICU care, and weekly rounds.
The study was approved by the Alfred Health Human Research Ethics Committee (Project No: 276/21).
Statistical analysis
Demographic and clinical characteristics were summarized by early thromboprophylaxis status. We calculated the annual proportion of omission of early thromboprophylaxis stratified by sex. We assessed the trends in omission of early thromboprophylaxis using a time series design with Autoregressive Integrated Moving Average (ARIMA) model.
Autocorrelation functions (ACF), partial autocorrelation functions (PACF), and Bayesian Information Criteria (BIC) were used to identify the best fitted model for analysis. The quarterly percentage change in omission of early thromboprophylaxis was used to remove the trend component of the time series before fitting into ARIMA models. Finally, the coefficient of the quarterly changes in percentage of omission of early thromboprophylaxis from the ARIMA model was annualized to obtain the annual percentage change. Mixed effects logistic regression modeling (accounting for the random effects of the contributing ICUs) was used to identify factors associated with omission of early thromboprophylaxis. Variables with P < 0.25 in the univariate analysis were included in the multivariable analysis along with other predictors previously reported as being significantly associated with omission of VTE prophylaxis. Generalized linear model with a binomial distribution and a probit link was used to assess factors associated with ICU level proportion of omission of VTE prophylaxis. P < 0.05 was considered significant in 2-sided tests. In the multivariate analysis, we examined the significance of the interaction terms between predictor variables included in the model. The proportion of missing data was negligible, and therefore, data imputation was not necessary. Analyses were carried out using Stata version 16 (StataCorp, College Station, TX, USA).
Results
Study subjects
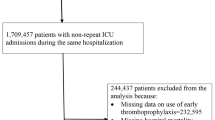
A total of 1,794,267 patients aged 18 years or older were admitted to 203 ICUs in Australia and New Zealand during the study period, and 1,465,020 patients (median age 65.3 ± 17.5 years) who have early thromboprophylaxis data were included in the analysis (Fig. 1). Patient characteristics by early thromboprophylaxis status are provided in Table 1. Overall, patient characteristics were comparable between those with and without missing data on early thromboprophylaxis (Supplementary Table S1).
Trends in omission of early thromboprophylaxis
Thromboprophylaxis was used in 1,260,785 (86.1%) of ICU patients within the first 24 h after ICU admission, considered as contraindicated in 55,025 (3.8%), and not indicated in 41,724 patients (2.9%). The remainder 107,486 (7.3%) ICU patients did not receive any form of thromboprophylaxis within the first 24 h after ICU admission. Compared to those who received early thromboprophylaxis, those who did not receive early thromboprophylaxis were more likely to be male (55.8% vs 44.2%), slightly younger, and they were less frequently admitted due to elective (35.9 vs 43.6) or surgical admissions (32.7 vs 43). The mean APACHE II score and admission diagnosis were comparable in both groups (Table 1). As shown in Fig. 2, omission of early thromboprophylaxis declined from 13.7% in 2009 to 4% in 2020 (by 70.8%), or 9.6% per year on average (P < 0.001). This decline was consistent across gender, different types of pre-existing condition and diagnosis at admission (Table 2, Supplemental Tables S2–S5).
Characteristics associated with omission of early thromboprophylaxis
In the confounder adjusted analysis, patients who have higher APACHE II scores (OR 1.03, 95% CI 1.02–1.07), chronic liver diseases (OR 1.42, 95% CI 1.36–1.50) and admitted to ICUs in New Zealand (OR 2.21, 95% CI 1.12–4.36) were more likely to miss early thromboprophylaxis. On the other hand, age (ORper 10-year increase 0.94, 95% CI 0.95, 0.99) and year of ICU admission (ORper calendar year 0.86, 95% CI 0.85, 0.96) were inversely associated with omission of early thromboprophylaxis. There was no significant association between omission of early thromboprophylaxis with patients’ sex, hospital type, admission diagnosis or source of ICU admission (Table 3).
Association between process of care indicators and omission of early thromboprophylaxis
Over the study period, a total of 1737 reports on 32 process indicators were reported by 144 ICUs on average, per year. The number of ICUs that have a documented process for monitoring VTE prophylaxis has almost doubled between 2010 (55.5%, 81/146) and 2020 (95%, 160/168). Overall, 38% of ICUs have a medical staff dedicated for coordinating quality of ICU care, employed on average (standard deviation) at 0.18 (0.5) full-time equivalent (FTE). The number of ICUs that had a medical staff dedicated for coordinating quality of ICU care has increased by 17% between 2013 (30.1%, 44/146) and 2018 (47%, 79/168) (Supplemental Fig. 1).
After adjusting for other covariates including patient volume, only documentation of VTE prophylaxis (OR= 0.90, 95%CI: 0.87-0.93), and full time equivalent (FTE) of medical staff dedicated for coordinating ICU quality activities (OR per 0.1 increase in FTE = 0.97, 95%CI: 0.93-0.99) were significantly associated with decline in omission of early thromboprophylaxis (Table 4). There was no significant association between having a pharmacist on ward round, adverse event minoring system, regular ICU patient or relative satisfaction survey with the omission of early thromboprophylaxis.
Discussion
Our data demonstrate that omission of thromboprophylaxis within the first 24 h after ICU admission declined by 70.8% between 2009 and 2020, and the decline is consistent across sex, different types of pre-existing chronic condition and diagnosis at admission. While younger patients are more likely to miss out on VTE prophylaxis, ICUs that have a medical quality lead dedicated for coordinating ICU have less omission of VTE prophylaxis.
The significant decline in omission of early thromboprophylaxis may be explained by improvement in VTE prevention practices [9, 17]. VTE prevention in hospitalized patients has become a national and international priority as a means of reducing avoidable hospital deaths [8, 18]. Standardized tools and resources have been developed and used in practice, in Australia and elsewhere, to standardize VTE risk assessment and provision of risk-appropriate thromboprophylaxis [9, 14, 17]. For example, the use of the multifaceted Australian National Inpatient Medication Chart (NIMC) encompassing VTE risk stratification, VTE prophylaxis guidance and prescription prompt has been associated with increased VTE prophylaxis prescription from 52.7 to 66.5% in medical patients [19]. Several VTE prevention strategies and initiatives, including provider education, regular audit, and feedback to medical and hospital staff have been implemented to promote and facilitate the uptake of VTE prophylaxis guidelines and improve awareness [14, 18, 20]. Recent studies have also shown improvement in the prevention of VTE and adherence to VTE prophylaxis guidelines in Australia [21, 22] and elsewhere [9]. Our findings of the significant decline in omission of early thromboprophylaxis were consistent across all ages, sex, admission diagnosis and pre-existing chronic diseases, suggesting a robust generalizability across sites and patient groups.
The faster rate of decline in omission of early thromboprophylaxis among ICUs that have increased availability of medical quality lead, and routinely document VTE prophylaxis is an important finding. A systematic review of experimental and observational studies has shown that availability of a practitioner dedicated to VTE quality improvement was associated with increased compliance to VTE clinical practice guidelines [23]. The documentation of VTE prophylaxis provides an opportunity for monitoring of compliance with VTE prevention guidelines and can assist hospitals in tracking the success of their efforts to prevent VTE [23, 24]. Our study specifically focused on omission of administration of early thromboprophylaxis and did not include data on VTE risk assessment and medication management. This is one possible reason for the absence of significant association between some of the individual components of the process of care indicators, including pharmacist on ward round, availability of allied health and nursing staff with omission of thromboprophylaxis. Furthermore, despite improvements during the study period, the implementation of most process indicators was low. On the other hand, it has been suggested that the current VTE-related quality measures used worldwide do not sufficiently characterize and represent a range of VTE prevention efforts in hospitals [15].
The findings that younger ICU patients were more likely to miss VTE prophylaxis than older patients suggest that younger ICU patients represent a potential target for initiatives to reduce the burden of VTE. The risk of VTE increases exponentially with age, doubling with each decade of life after the age of 40 years [9, 25], and as such older patients are more likely to receive VTE prophylaxis. However, approximately 50% of all VTE events are related to current or recent hospital admission [26], and therefore, the risk of VTE in middle-aged ICU patients should not be underestimated. The lower risk of VTE in younger ages could be one of the reasons for the frequent omission of thromboprophylaxis in younger ICU patients [27]. Some tests and diagnostics for screening the risk of VTE and bleeding are also not frequently used in younger patients, including to avoid increasing the lifetime cancer risks from exposure to radiation, possibly underestimating the risk of VTE [28, 29].
Our findings have potential implications for VTE prevention in ICU patients. The findings that younger patients are more like to miss out on VTE prophylaxis provides an opportunity to efficiently target younger critically ill patients for VTE prevention. Further research may consider if additional clinical or laboratory parameters can be leveraged to improve identification of younger patients at risk of VTE who would benefit from VTE prophylaxis. The findings also suggest that compliance with VTE process of care indicators, such as documented process for monitoring VTE prophylaxis and medical lead dedicated for coordinating ICU quality, provides an opportunity for system improvements to reduce the burden of potentially preventable VTE.
This study has some limitations that should be noted. The ANZICS APD does not collect data on additional variables which are potentially important for understanding VTE prophylaxis, including the outcome of VTE risk assessment, reasons for not receiving thromboprophylaxis, regimen, dose and duration of anticoagulant. Contextual factors such as local expert opinion, clinician awareness of thromboprophylaxis and the involvement of the patient in the decision-making process that potentially influence decision‐making about anticoagulant prescription were not collected.
Conclusions
In summary, our findings suggest that in critically ill patients in Australia and New Zealand omission of early thromboprophylaxis within the first 24 h after ICU admission has declined by 70.8% between or 9.6% 2009 and 2020. The decline was consistent across gender, different types of pre-existing condition and diagnosis at admission. Allocating a medical lead dedicated to coordinating ICU quality offers one of the most promising strategies for optimizing VTE prevention in hospitalized patients.
References
Di Nisio M, van Es N, Büller HR (2016) Deep vein thrombosis and pulmonary embolism. Lancet 388(10063):3060–3073. https://doi.org/10.1016/S0140-6736(16)30514-1
Wendelboe AM, Raskob GE (2016) Global burden of thrombosis. Circ Res 118(9):1340–1347. https://doi.org/10.1161/CIRCRESAHA.115.306841
Søgaard KK, Schmidt M, Pedersen L, Horváth-Puhó E, Sørensen HT (2014) 30-Year mortality after venous thromboembolism. Circulation 130(10):829–836. https://doi.org/10.1161/CIRCULATIONAHA.114.009107
Ejaz A, Ahmed MM, Tasleem A et al (2018) Thromboprophylaxis in intensive care unit patients: a literature review. Cureus 10(9):e3341. https://doi.org/10.7759/cureus.3341
Minet C, Potton L, Bonadona A et al (2015) Venous thromboembolism in the ICU: main characteristics, diagnosis and thromboprophylaxis. Crit Care 19(1):287. https://doi.org/10.1186/s13054-015-1003-9
Tran HA, Gibbs H, Merriman E et al (2019) New guidelines from the Thrombosis and Haemostasis Society of Australia and New Zealand for the diagnosis and management of venous thromboembolism. Med J Aust 210(5):227–235. https://doi.org/10.5694/mja2.50004
Fernando SM, Tran A, Cheng W et al (2022) Venous thromboembolism prophylaxis in critically ill adults: a systematic review and network meta-analysis. Chest. https://doi.org/10.1016/j.chest.2021.08.050
Henke PK, Kahn SR, Pannucci CJ et al (2020) Call to action to prevent venous thromboembolism in hospitalized patients: a policy statement from the American Heart Association. Circulation 141(24):e914–e931. https://doi.org/10.1161/cir.0000000000000769
Nicholson M, Chan N, Bhagirath V, Ginsberg J (2020) Prevention of venous thromboembolism in 2020 and beyond. J Clin Med 9(8):2467. https://doi.org/10.3390/jcm9082467
Kahn SR, Lim W, Dunn AS et al (2012) Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141(2 Suppl):e195S-e226S. https://doi.org/10.1378/chest.11-2296
Cohen AT, Tapson VF, Bergmann J-F et al (2008) Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 371(9610):387–394. https://doi.org/10.1016/S0140-6736(08)60202-0
Hecht JP, Han EJ, Cain-Nielsen AH, Scott JW, Hemmila MR, Wahl WL (2021) Association of timing of initiation of pharmacologic venous thromboembolism prophylaxis with outcomes in trauma patients. J Trauma Acute Care Surg 90(1):54–63. https://doi.org/10.1097/ta.0000000000002912
Ho KM, Chavan S, Pilcher D (2011) Omission of early thromboprophylaxis and mortality in critically ill patients: a multicenter registry study. Chest 140(6):1436–1446. https://doi.org/10.1378/chest.11-1444
Australian Commission on Safety and Quality in Health Care (2020) Implementation guide: Venous Thromboembolism Prevention Clinical Care Standard. ACSQHC, Sydney. https://www.safetyandquality.gov.au/sites/default/files/2020-12/implementation_guide_venous_thromboembolism_prevention_december_2020.pdf. Accessed 29 Aug 2021
Lau BD, Haut ER (2014) Practices to prevent venous thromboembolism: a brief review. BMJ Qual Saf 23(3):187–195. https://doi.org/10.1136/bmjqs-2012-001782
Stow PJ, Hart GK, Higlett T et al (2006) Development and implementation of a high-quality clinical database: the Australian and New Zealand Intensive Care Society Adult Patient Database. J Crit Care 21(2):133–141. https://doi.org/10.1016/j.jcrc.2005.11.010
Roberts LN, Durkin M, Arya R (2017) Annotation: developing a national programme for VTE prevention. Br J Haematol 178(1):162–170. https://doi.org/10.1111/bjh.14769
Australian Commission on Safety and Quality in Health Care (2020) Venous thromboembolism prevention clinical care standard. ACSQHC, Sydney. https://www.safetyandquality.gov.au/sites/default/files/2020-01/venous_thromboembolism_prevention_clinical_care_standard_-_jan_2020_2.pdf. Accessed 27 Aug 2020
Liu DSH, Lee MMW, Spelman T et al (2012) Medication chart intervention improves inpatient thromboembolism prophylaxis. Chest 141(3):632–641. https://doi.org/10.1378/chest.10-3162
Kahn SR, Morrison DR, Diendéré G et al (2018) Interventions for implementation of thromboprophylaxis in hospitalized patients at risk for venous thromboembolism. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008201.pub3
Schaden E, Metnitz PG, Pfanner G et al (2012) Coagulation Day 2010: an Austrian survey on the routine of thromboprophylaxis in intensive care. Intensive Care Med 38(6):984–990. https://doi.org/10.1007/s00134-012-2533-0
Aziz H, Mills D, Newbury J (2019) Adherence to antithrombotic therapy guidelines and atrial fibrillation in a rural hospital: a clinical audit. Rural Remote Health 19(1):4342. https://doi.org/10.22605/rrh4342
Gaston S, White S, Misan G (2012) Venous thromboembolism (VTE) risk assessment and prophylaxis: a comprehensive systematic review of the facilitators and barriers to healthcare worker compliance with clinical practice guidelines in the acute care setting. JBI Evid Synth 10(57):3812–3893
Rowswell HR, Nokes TJC (2017) Significant reduction in hospital-acquired thrombosis: impact of national risk assessment and real-time feedback. Open Heart 4(2):e000653. https://doi.org/10.1136/openhrt-2017-000653
Bell EJ, Lutsey PL, Basu S et al (2016) Lifetime risk of venous thromboembolism in two cohort studies. Am J Med 129(3):339.e19–26. https://doi.org/10.1016/j.amjmed.2015.10.014
Schünemann HJ, Cushman M, Burnett AE et al (2018) American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv 2(22):3198–3225. https://doi.org/10.1182/bloodadvances.2018022954
Azu MC, McCormack JE, Scriven RJ, Brebbia JS, Shapiro MJ, Lee TK (2005) Venous thromboembolic events in pediatric trauma patients: is prophylaxis necessary? J Trauma Acute Care Surg 59(6):1345–1349
Stein PD, Hull RD, Kayali F, Ghali WA, Alshab AK, Olson RE (2004) Venous thromboembolism according to age: the impact of an aging population. Arch Intern Med 164(20):2260–2265. https://doi.org/10.1001/archinte.164.20.2260
Konstantinides SV, Meyer G, Becattini C et al (2019) 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): the Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J 2019. https://doi.org/10.1183/13993003.01647-2019
Acknowledgements
The authors and the ANZICS CORE management committee would like to thank clinicians, data collectors and researchers at the contributing sites (Supplementary Table S6).
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The authors declare that no funding was received for the present study. James D. McFadyen is supported by an NHMRC Early Career Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest relevant to the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sahle, B.W., Pilcher, D., Peter, K. et al. Trends and risk factors for omission of early thromboprophylaxis in Australian and New Zealand ICUs between 2009 and 2020. Intensive Care Med 48, 590–598 (2022). https://doi.org/10.1007/s00134-022-06672-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-022-06672-7