Abstract
Purpose
It is currently unclear whether management and outcomes of critically ill patients differ between men and women. We sought to assess the influence of age, sex and diagnoses on the probability of intensive care provision in critically ill cardio- and neurovascular patients in a large nationwide cohort in Switzerland.
Methods
Retrospective analysis of 450,948 adult patients with neuro- and cardiovascular disease admitted to all hospitals in Switzerland between 01/2012 and 12/2016 using Bayesian modeling.
Results
For all diagnoses and populations, median ages at admission were consistently higher for women than for men [75 (64;82) years in women vs. 68 (58;77) years in men, p < 0.001]. Overall, women had a lower likelihood to be admitted to an intensive care unit (ICU) than men, despite being more severely ill [odds ratio (OR) 0.78 (0.76–0.79)]. ICU admission probability was lowest in women aged > 65 years (OR women:men 0.94 (0.89–0.99), p < 0.001). Women < 45 years had a similar ICU admission probability as men in the same age category [OR women:men 1.03 (0.94–1.13)], in spite of more severe illness. The odds to die were significantly higher in women than in men per unit increase in Simplified Acute Physiology Score (SAPS) II (OR 1.008 [1.004–1.012]).
Conclusion
In the care of the critically ill, our study suggests that women are less likely to receive ICU treatment regardless of disease severity. Underuse of ICU care was most prominent in younger women < 45 years. Although our study has several limitations that are imposed by the limited data available from the registries, our findings suggest that current ICU triage algorithms could benefit from careful reassessment. Further, and ideally prospective, studies are needed to confirm our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In our analysis of 450’948 neuro- and cardiovascular patients, women, and in particular young women, had a lower likelihood to receive ICU care than men, despite being more severely ill. Although our study is limited by the number of available variables, our data suggest that health care inequalities between women and men might still exist, even in one of the highest ranked health care systems worldwide. Careful reassessment of triage algorithms and local protocols might help to ensure optimal and equitable use of critical care resources, thereby improving outcomes. |
Introduction
Cardiovascular disease (CVD) remains the most common cause of morbidity and mortality in both women and men in the Western World [1]. Since the 1980s, age-adjusted mortality for CVD has continuously declined, however to a lesser extent in women than in men [2]. Despite growing evidence regarding sex and gender differences in CVD, mechanisms behind these differences remain largely unexplored [3]. Further, significant cardiovascular health inequalities between women and men persist in the diagnostic accuracy of tests, timely and evidence-based treatment, secondary prevention, and outcomes [3,4,5,6]. Importantly, younger women with CVD have a particularly unfavorable prognosis and a plethora of unanswered questions remains in this demographic group [7,8,9,10].
The impact of gender on provision and outcomes of critical care treatment has been described in several smaller cohorts. Overall, women remain underrepresented amongst intensive care unit (ICU) patients, in particular amongst higher age groups [11,12,13,14], are less likely to receive life-supporting treatments, and have overall shorter ICU stays than men [15,16,17]. This contrasts with the fact that CVD prevalence is higher in older women than in older men with women having a higher burden of pre-existing disabilities [3, 18, 19]. With the anticipated surge in the ageing population, the prevalence of these conditions is projected to increase even further and will be set against a limited number of ICU beds and staff. As simultaneously medical technology advances, there is an urgent need to understand barriers for the provision of ICU care to ensure optimal and unbiased use of resources. Thus, we sought to assess how sex and age influence ICU admission in cardio- and neurovascular patients in a large nationwide cohort in Switzerland.
Methods
Study population
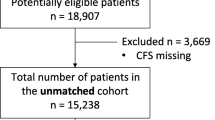
The designated primary outcome measure of this study was admission to ICU. Secondary outcome measures included advanced treatments and ICU mortality. Patients aged < 20 years, ICU readmissions within the same hospital stay, and planned ICU admissions were excluded from the analysis. Data on ICU admissions were obtained from the Swiss ICU-Registry. The Swiss ICU-Registry (MDSi—Minimal Dataset for ICUs) is owned and operated by the Swiss Society of Intensive Care Medicine (SSICM). Details of the MDSi dataset have previously been described [20]. Briefly, the database contains prospectively collected data from 86 certified Swiss ICUs including information on origin and type of admission, diagnostic group and intervention, severity of acute illness, daily process variables and discharge details comprising ICU mortality. The MDSi dataset does not contain data from intermediate care units. Data are transferred anonymously to the MDSi from each contributing ICU.
The MDSi dataset provides data on ICU patients (main diagnosis, death, sex, age) to the Swiss Federal Office of Statistics (Schweizer Bundesamt für Statistik [BfS]). For our analysis, data on ICU admissions were obtained from the MDSi database, while data on general hospital admissions were provided by the BfS. From both datasets, patients who were admitted to either ICU or normal ward between 01/2012 (begin of detailed prospective data collection by the Swiss ICU-Registry) and 12/2016 (data validation completed) with one of the following cardiovascular diagnoses were extracted: acute coronary syndrome including cardiac arrest, pulmonary embolism, acute heart failure, rhythm disturbances or stroke. We extracted demographic data, admission diagnoses codes, type of admission, the Simplified Acute Physiology Score (SAPS) II [21], the nine equivalents of nursing manpower use score (NEMS) [22], ICU length-of-stay (LOS), and ICU mortality. In both datasets, no information on the patients’ pre-admission status (comorbidities or chronic diseases) is provided. Completeness (no missing data) and high quality of the dataset were ensured using only validated data acquired between 01/2012 and 12/2016. The study was approved by the Ethics committee of Northwestern Switzerland (EKNZ UBE-15/47) as well as by the scientific committee of the SSICM.
Definitions
Unplanned ICU admissions were defined as unstable patients transferred from the emergency department, normal wards, the operating theater, or other hospitals with the need for extended medical care and monitoring. Type of admission was defined as either admission from home or from another hospital. Interventions upon admission were included when performed within 48 h prior or after admission. LOS was defined as the time from ICU admission to discharge or death, and LOS was expressed in fractions of days. The overall NEMS was normalized to LOS. ICU mortality was defined as the rate of all-cause mortality during the ICU hospitalization.
Statistical analysis
Statistical analysis was performed using R version 3.6.1 with the packages rstan, rstanarm and survival [23]. Simple group comparisons were performed using t-test, non-parametric rank sum test or chi-square test as appropriate. Bayesian models were used to estimate the hospital admission counts as a function of age and the probability of ICU admission (primary objective) [24, 25]. Frequentist analyses were performed to model the likelihood of ICU mortality (secondary objective) and to assess gender differences in advanced treatments (secondary objective) [26, 27]. Linear regression models of SAPS II and NEMS and binomial logistic regression models of death comprised the sex-dependent covariates age and diagnosis. Detailed information on statistical modeling is provided in the Supplementary Information File.
Results
Patient characteristics
Admission
450,948 patients admitted to either the ICU (n = 77,803, 17.3%) or general ward (n = 373,145, 82.7%) with the diagnoses of pulmonary embolism (n = 24,077, 5.3%), heart failure (89,326, 19.8%), rhythm disturbance (n = 72,975, 16.2%), acute coronary syndrome including cardiac arrest patients (n = 183,762, 40.8%), and stroke (n = 80,808, 17.9%) between 01/2012 and 12/2016 were included in our analysis (Table 1). Women were less often admitted to the ICU, independent of diagnoses (pulmonary embolism 10.6 vs. 12.3%, heart failure 10.0 vs. 14.5%, rhythm disturbance 11.2 vs. 13.0%, acute coronary syndrome including cardiac arrest 21.7 vs. 22.3%, stroke 16.5 vs. 19.3%, Table 1), independent of age category (Supplementary Table S1). Conversely, more women than men were admitted to the general wards (pulmonary embolism 89.4 vs. 87.7%, heart failure 90.0 vs. 85.5%, rhythm disturbance 88.8 vs. 87.0%, acute coronary syndrome 78.3 vs. 77.7%, stroke 83.5 vs. 80.7%, Table 1). Men who were transferred from another hospital were more often admitted to the ICU than women (13.5 vs. 16.1% in men, p < 0.001, Table 1), while direct ICU admissions were more frequent in women (74.6 vs. 74.0% in men, p < 0.001, Table 1).
Age at admission
In ICU patients, median age was higher in women as compared to men (75 [interquartile range [IQR] 64;82] years in women vs. 68 [IQR 58;77] years in men, p < 0.001) Accordingly, overall peak ages at admission (ICUs and general wards) were significantly higher in women as compared to men, independent of diagnosis (Fig. 1, Supplementary Table S2).
Disease severity
In ICU patients, median SAPS II was higher in women as compared to men [29 (IQR 23;40) in women and 27 (IQR 20;38) in men, p < 0.001]. Accordingly, multivariate linear regression models showed higher estimates for SAPS II in women admitted to the ICUs as compared to men [8.47 (6.71–10.23) in women and 4.06 (2.74–5.39) in men, ratio women:men 4.40 (2.20–6.61), p < 0.001]. When stratified by age, younger women < 45 years had consistently higher baseline estimates for SAPS II as compared to men; while, an opposite trend was observed at the age > 65 years (Supplementary Fig. S1). Hence, sex differences in median SAPS II were most pronounced in younger individuals, with younger women presenting with higher SAPS II than younger men (Supplementary Fig. S1). When stratified by diagnoses, baseline estimates of SAPS II were significantly higher in women across all diagnoses (Supplementary Table S3).
Probability of ICU admission (primary outcome)
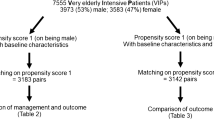
Overall, women had a lower likelihood to be admitted to the ICU than men [odds ratio (OR) 0.78 (0.76–0.79), Table 2]. Multivariate Bayesian regression analysis adjusted for admission diagnosis, age categories (< 45 years, > 65 years) and proximity to peak age revealed that the odds for ICU admission were significantly lower in women as compared to men for heart failure [women 0.17 (0.16–0.18); men 0.24 (0.23–0.25); women:men OR 0.73 (0.69–0.77)] and stroke [women 0.29 (0.28–0.31); men 0.32 (0.31–0.33); women:men OR 0.92 (0.87–0.98), Table 2]. In contrast, women presenting with an acute coronary syndrome including cardiac arrest had a higher probability than men to be admitted to the ICU [women odds 0.40 (0.39–0.42); men odds 0.37 (0.36–0.39); women:men OR 1.08 (1.03–1.14), Table 2]. When the overall study population was stratified by age categories, women < 45 years of age showed a trend towards a lower admission probability as compared to men (Fig. 2), yet the odds ratio women:men did not reach significance in the adjusted Bayesian model [admission probabilities women:men < 45 years OR 1.03 (0.94–1.13), Table 2]. Women > 65 years had a lower probability to be admitted to the ICU than men [women:men OR 0.94 (0.89–0.99), Fig. 2 and Table 2].
Calculated total probability of admission for men and women for each age category. Age categories in proximity to peak age show the lowest overall probability of admission for both sexes. Bold lines represent median probabilities. Probability of ICU admission plotted for each age group (5 year intervals). ICU intensive care unit
Secondary outcome measures
Advanced treatments
No significant sex differences were observed for NEMS in the overall population (Table 1) and in age-stratified subgroups (Supplementary Table S1). When individual components of the NEMS were analyzed, men had higher rates of mechanical ventilation (23.40 vs. 22.51% in women, p = 0.005, Table 1), while women more often received non-invasive respiratory support (73.50 vs. 71.74% in men, p < 0.001, Table 1). Men had a greater use of vasoactive substances (12.68 vs. 11.77% in women, p < 0.001 for multiple vasoactives, Table 1) and a higher rate of renal replacement therapy (RRT, 2.68 vs. 2.02%, p < 0.001, Table 1). When stratified by age, women < 45 years had higher rates of mechanical ventilation (25.25 vs. 21.02% in men, p = 0.004), received more often multiple vasoactives (14.71 vs. 11.41% in men, p = 0.004) and RRT (4.25 vs. 2.47% in men, p = 0.003) than men (Supplementary Table S1). An opposite trend was observed in women > 65 years with regard to these treatments (p < 0.001, Supplementary Table S1).
Amongst patients with an acute coronary syndrome, 21,845 patients underwent percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). Significantly more men than women underwent PCI (53.97 vs. 43.73%, p < 0.001, Table 1) or CABG (2.07 vs. 3.04%, p < 0.001, Table 1). This was also true when the study sample was stratified by age categories, with gender differences being most pronounced in the younger age group < 45 years (PCI: 13.56 vs. 33.38% in men, p < 0.001, Supplementary Table 1).
ICU mortality
Frequentist statistics revealed that ICU mortality was 6.7% in women and 6.1% in men (p < 0.001, Table 1). Women < 45 years and women aged 45–65 years died more often during ICU stay than men in the same age category (< 45 years: 7.03 vs. 5.30%, p = 0.039 and 45–65 years: 6.23 vs. 4.04%, p < 0.001, Supplementary Table S1). In contrast, in individuals > 65 years, ICU mortality was lower in women as compared to men in the same age category (6.86 vs. 7.35%; p = 0.039). Binomial logistic regression of the probability of all-cause death during ICU stay using unscaled covariates (diagnoses, age < 45 years, age > 65 years, SAPS II, NEMS /LOS) showed a significantly higher mortality in women with an acute coronary syndrome [OR 1.479 (1.21–1.81), p < 0.001, Fig. 3, Supplementary Table S4] or pulmonary embolism [OR 1.793 (1.11–2.90), p < 0.05, Fig. 3, Supplementary Table S4], as compared to men, while mortality for heart failure, rhythm disturbance, and stroke did not differ significantly between sexes (Fig. 3, Supplementary Table S4). In both sexes, a higher SAPS II was associated with a higher ICU mortality [women 1.096 (1.09–1.10), p < 0.001 and men 1.088 (1.085–1.090), p < 0.001, Fig. 3, Supplementary Table S4], but the association between increased SAPS II and the risk of death was significantly stronger in women as compared to men [OR 1.008 (1.004–1.012), p < 0.001, Fig. 3, Supplementary Table S4].
Binomial analysis of death. Odds and odds ratios are given with 95%-confidence intervals. Baseline is a diagnosis of acute coronary syndrome including cardiac arrest, an average SAPS II of 31.2 and NEMS/LOS of 99.7. P < 0.05*, < 0.01**, < 0.001***. X-axis in logarithmic scale. ICU intensive care unit; SAPS II Simplified Acute Physiology Score II; NEMS Nine Equivalents of Nursing Manpower Use Score; LOS length-of-stay
Discussion
Our nationwide analysis in 450,948 patients with cardio- and neurovascular diseases shows that women in the upper and lower extremes of age are the demographic groups most affected by inequalities in ICU care.
Recent studies report an increasing incidence and mortality rate of CVD in younger women [7,8,9,10]. Mechanisms and robust data explaining the excess risk for cardiovascular mortality in younger women are currently lacking, but data from the VIRGO study indicate that younger women have a worse overall health status than younger men [28]. In line with these data, young women < 45 years were more severely ill than men of similar age in our study. More severe illness usually requires a higher level of medical care. However, despite their more severe illness, younger women in our study were not admitted more frequently to the ICU than younger men. Instead, the probability to receive ICU care was similar in younger women and men. Unfortunately, current data are insufficient to clarify the extent to which such inequalities originate from sex differences in pathophysiology (e.g., presentation of symptoms), risk stratification (diagnostic bias), less aggressive treatment preferences by younger women or underuse of resources.
Age > 65 years was associated with a significantly lower probability of ICU admission in women as compared to men. The reason for this gender disparity remains elusive. Although social networks, family support as well as triage decisions are known to be important predictors for ICU admissions, recent studies have demonstrated that these variables were not associated with the male predominance amongst the elderly ICU population [11, 13, 14]. Recent data on treatment limitations derived from the same database show that women were more likely to have a documented patient decree upon ICU admission [29]. Accordingly, limitation decisions were more frequent in women, despite their less severe illness. This observation is consistent with previous studies reporting that female sex was an independent predictor of treatment limitation decisions in patients with sepsis [30, 31]. Accordingly, women or their surrogates had less aggressive treatment preferences in previous studies [32, 33]. Thus, the higher frequency of advanced directives in elderly women might impact the decision process of ICU admission, resulting in a selection bias. In addition, there is extreme variability in how health care providers influence end-of-life decisions [34]. Hence, there is urgent need to evaluate whether there is an unconscious bias in how critically ill elderly women and men are assessed and whether their wishes are (mis)perceived.
Our findings are consistent with previous studies derived from smaller and more heterogenous populations demonstrating a male predominance in ICU hospital admissions [11,12,13,14,15, 17]. We now extend the existing literature by showing that women hospitalized for neuro- and cardiovascular diseases were significantly older than men across all conditions. The largest sex difference in age was observed in patients presenting with an acute coronary syndrome, with a larger age gap between men and women being seen in the ICU population as compared to the general ward population. Accordingly, women presenting with an acute coronary syndrome had higher estimates of SAPS II and encountered an excess ICU mortality as compared to men in our study. However, it is notable that women with acute coronary syndrome were the only female subgroup in our study that had a higher likelihood to be admitted to the ICU than their male counterparts. The latter might be indicative of the growing attention that has been paid to health disparities in women presenting with acute coronary syndrome [8, 35]. Nevertheless, consistent with published literature, we also observed that women with an acute coronary syndrome underwent less often life-saving invasive procedures including percutaneous coronary interventions or coronary artery bypass grafting. The fact that women with CVD receive less evidence-based treatment than men was first described in 1991 and was named the’Yentl Syndrome’ [36]. Our data indicate that health care inequalities between men and women persist in contemporary practice and emphasize the need to identify barriers for the underuse of advanced treatment options in critically ill women. Indeed, while there is increasing awareness for sex and gender differences in the cardiovascular field, gender disparities in intensive care medicine are still a widely neglected topic.
Multivariate linear regression models showed higher estimates for SAPS II in women admitted to the ICUs as compared to men, independent of diagnoses. In addition, the association between increased SAPS II and the risk of death was significantly stronger in women as compared to men indicating that more severe illness in women had a greater impact on mortality than in men. Although the influence of sex on the SAPS II score’s ability to predict outcome was not specifically tested in our study, our data suggest that the SAPS II performs different in women and men. A similar observation has previously been reported for the sequential organ failure assessment (SOFA) score [37]. The fact that these prediction tools perform different in men and women is not surprising, given that none of these scores includes sex as a variable. In cardiovascular patients, the outcome predictive value of ICU scores related to sex was only explored in one recent study. In this report, the performance of currently used ICU-based risk stratification systems in predicting in-hospital mortality was limited in both women and men, especially in those subgroups of disease with the highest mortality [38]. Given the overall higher ICU mortality observed in women in our cohort, our limited knowledge regarding the influence of sex and sex-specific variables on the predictive value of ICU-based risk prediction tools is particularly remarkable. Future studies will have to assess whether sex changes how the other variables in SAPS II account for total risk estimation.
Some limitations to this study should be pointed out. First, our study is retrospective and observational, and does not provide information on underling causal mechanisms. Second, data on in- and out-of-hospital mortality were not available in our dataset. Hence, the question whether gender imbalances in ICU admission have altered these endpoints cannot be answered by our study. Third, information on patient demographics and health status prior to admission was limited in our study sample. Hence, we cannot rule out potential confounding by variables (e.g., distribution of pre-existing comorbidities and chronic diseases in different age categories, patient frailty or socio-economic variables) not accounted for in our statistical models. Fourth, SAPS II was only available as the overall score, precluding a more informative analysis as compared to the use of SAPS II subitems. Fifths, given that information on mechanical ventilation, hemodialysis and vasoactive support is included in the NEMS, the latter was used as an estimate of disease severity, although it was originally developed as a predictor for the burden of nursing care. Sixth, our dataset was dichotomized in patients being admitted to the ICU or normal ward. Patients being admitted to intermediate care units were not included in the ICU dataset which might limit the generalizability of our findings. Nevertheless, ICU mortality observed in our study is comparable with previously reported data [39] thereby indicating that our dataset is representative of a typical and contemporary ICU population. Seventh, data for cardiac arrest and acute coronary syndrome were aggregated in our study sample leading to a slightly higher overall mortality in this subgroup of patients as compared to previous studies [40].
Intensive care is expensive and demand for ICU resources often exceeds supply. Our data suggest that women, in particular young women, have to present with more severe illness to receive equal treatment as men. Thus, intensivists and emergency physicians making triage decisions should carefully reassess whether critically ill young women are at risk to fail receiving the care they need. Addressing gender biases in triage algorithms and local protocols will help to ensure equal application of intensive therapy.
While our study is limited by the number of available variables from the registries, our findings may serve as a catalyst for further research on sex disparities in the provision of ICU care. Future studies will have to identify biological and social factors influencing the decision to withhold or withdraw intensive care in women. Prospective studies delivering more detailed information on pre-admission health status are needed to confirm our findings. Finally, further education is needed to raise awareness for gender inequalities in intensive care in both healthcare professionals and patients.
Data availability
Data are available from the University Hospital Basel Institutional Data Access for researchers who meet the criteria for access to confidential data.
References
Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M (2016) Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J 37(42):3232–3245
Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C et al (2014) Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol 64(4):337–345
Haider A, Bengs S, Luu J, Osto E, Siller-Matula JM, Muka T et al (2020) Sex and gender in cardiovascular medicine: presentation and outcomes of acute coronary syndrome. Eur Heart J 41(13):1328–1336
Gruen J, Caraballo C, Miller PE, McCullough M, Mezzacappa C, Ravindra N et al (2020) Sex differences in patients receiving left ventricular assist devices for end-stage heart failure. JACC Heart Fail 8(9):770–779
Scott PE, Unger EF, Jenkins MR, Southworth MR, McDowell TY, Geller RJ et al (2018) Participation of women in clinical trials supporting FDA approval of cardiovascular drugs. J Am Coll Cardiol 71(18):1960–1969
Mauvais-Jarvis F, Bairey Merz N, Barnes PJ, Brinton RD, Carrero JJ, DeMeo DL et al (2020) Sex and gender: modifiers of health, disease, and medicine. Lancet 396(10250):565–582
Smilowitz NR, Gupta N, Guo Y, Zhong J, Weinberg CR, Reynolds HR et al (2018) Acute myocardial infarction during pregnancy and the puerperium in the United States. Mayo Clin Proc 93(10):1404–1414
Gabet A, Danchin N, Juilliere Y, Olie V (2017) Acute coronary syndrome in women: rising hospitalizations in middle-aged French women, 2004–14. Eur Heart J 38(14):1060–1065
Arora S, Stouffer GA, Kucharska-Newton AM, Qamar A, Vaduganathan M, Pandey A et al (2019) Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation 139(8):1047–1056
Vaccarino V (2019) Myocardial infarction in young women. Circulation 139(8):1057–1059
Hill A, Ramsey C, Dodek P, Kozek J, Fransoo R, Fowler R et al (2019) Examining mechanisms for gender differences in admission to intensive care units. Health Serv Res. https://doi.org/10.1111/1475-6773.13215
Samuelsson C, Sjoberg F, Karlstrom G, Nolin T, Walther SM (2015) Gender differences in outcome and use of resources do exist in Swedish intensive care, but to no advantage for women of premenopausal age. Crit Care 19:129
Larsson E, Zettersten E, Jaderling G, Ohlsson A, Bell M (2015) The influence of gender on ICU admittance. Scand J Trauma Resusc Emerg Med 23:108
Zettersten E, Jaderling G, Larsson E, Bell M (2019) The impact of patient sex on intensive care unit admission: a blinded randomized survey. Sci Rep 9(1):14222
Fowler RA, Sabur N, Li P, Juurlink DN, Pinto R, Hladunewich MA et al (2007) Sex-and age-based differences in the delivery and outcomes of critical care. CMAJ 177(12):1513–1519
Dodek P, Kozak JF, Norena M, Wong H (2009) More men than women are admitted to 9 intensive care units in British Columbia. J Crit Care. 24(4):630.e1–8
Zettersten E, Jaderling G, Bell M, Larsson E (2019) Sex and gender aspects on intensive care. A cohort study. J Crit Care 55:22–27
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP et al (2020) Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation 141(9):e139–e596
Phan HT, Blizzard CL, Reeves MJ, Thrift AG, Cadilhac DA, Sturm J et al (2019) Sex differences in long-term quality of life among survivors after stroke in the INSTRUCT. Stroke 50(9):2299–2306
Perren A, Cerutti B, Kaufmann M, Rothen HU, Swiss Society of Intensive Care M (2019) A novel method to assess data quality in large medical registries and databases. Int J Qual Health Care. https://doi.org/10.1093/intqhc/mzy249
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270(24):2957–2963
Reis Miranda D, Moreno R, Iapichino G (1997) Nine equivalents of nursing manpower use score (NEMS). Intensive Care Med 23(7):760–765
Team RC. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2019. Available: https://www.R-project.org/. Accessed 10 Nov 2020
Cowles MK (2013) Applied Bayesian statistics. Springer-Verlag, New York, p 232
Chan AB, Vasconcelos N (2012) Counting people with low-level features and Bayesian regression. IEEE Trans Image Process 21(4):2160–2177
Shahbaba B (2012) Biostatistics with R. Springer-Verlag, New York
Rezaul Karim M, Ataharul IM (2019) Reliability and Survival Analysis. Springer, Sigapore
Dreyer RP, Smolderen KG, Strait KM, Beltrame JF, Lichtman JH, Lorenze NP et al (2016) Gender differences in pre-event health status of young patients with acute myocardial infarction: a VIRGO study analysis. Eur Heart J Acute Cardiovasc Care 5(1):43–54
Kaufmann M, Perren A, Cerutti B, Dysli C, Rothen HU, Swiss Society of Intensive Care M (2020) Severity-Adjusted ICU Mortality Only Tells Half the Truth-The Impact of Treatment Limitation in a Nationwide Database. Crit Care Med. https://doi.org/10.1097/CCM.0000000000004658
Pietropaoli AP, Glance LG, Oakes D, Fisher SG (2010) Gender differences in mortality in patients with severe sepsis or septic shock. Gend Med 7(5):422–437
Block L, Petzold M, Syrous AN, Lindqvist B, Odenstedt Hergès H, Naredi S (2019) Age, SAPS 3 and female sex are associated with decisions to withdraw or withhold intensive care. Acta Anaesthesiol Scand 63(9):1210–1215
Bookwala J, Coppola KM, Fagerlin A, Ditto PH, Danks JH, Smucker WD (2001) Gender differences in older adults’ preferences for life-sustaining medical treatments and end-of-life values. Death Stud 25(2):127–149
Wenger NS, Pearson ML, Desmond KA, Harrison ER, Rubenstein LV, Rogers WH et al (1995) Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 155(19):2056–2062
Cook DJ, Guyatt GH, Jaeschke R, Reeve J, Spanier A, King D et al (1995) Determinants in Canadian health care workers of the decision to withdraw life support from the critically ill Canadian Critical Care Trials Group. JAMA 273(9):703–708
Sabbag A, Matetzky S, Porter A, Iakobishvili Z, Moriel M, Zwas D et al (2017) Sex differences in the management and 5-year outcome of young patients (<55 years) with acute coronary syndromes. Am J Med. https://doi.org/10.1016/j.amjmed.2017.05.028
Healy B (1991) The Yentl syndrome. N Engl J Med 325(4):274–276
Jacobson S, Liedgren E, Johansson G, Ferm M, Winsö O (2012) Sequential organ failure assessment (SOFA) scores differ between genders in a sepsis cohort: cause or effect? Ups J Med Sci 117(4):415–425
Herscovici R, Mirocha J, Salomon J, Merz NB, Cercek B, Goldfarb M (2020) Sex differences in crude mortality rates and predictive value of intensive care unit-based scores when applied to the cardiac intensive care unit. Eur Heart J Acute Cardiovasc Care 9(8):966–974
Weigl W, Adamski J, Goryński P, Kański A, Hultström M (2017) Mortality rate is higher in Polish intensive care units than in other European countries. Intensive Care Med 43(9):1430–1432
Radovanovic D, Seifert B, Roffi M, Urban P, Rickli H, Pedrazzini G et al (2017) Gender differences in the decrease of in-hospital mortality in patients with acute myocardial infarction during the last 20 years in Switzerland. Open Heart 4(2):e000689
Acknowledgements
The authors thank Christian Schindler (senior statistician of the Swiss Tropical and Public Health Institute, Basel, Switzerland) for providing expert advice to the statistical analysis and for critically reviewing the manuscript. The authors are grateful to Vera Regitz-Zagrosek (Charité Berlin, Germany) for critically reading the manuscript.
Funding
Open Access funding provided by Universität Basel (Universitätsbibliothek Basel). CEG was supported by grants from the Research Foundation in Anesthesiology and Intensive Care Medicine, University Hospital Basel, the Research Fund of the University of Basel and the Swiss National Science Foundation (SNSF). CG was supported by grants from the SNSF, the Olga Mayenfisch Foundation, Switzerland, the OPO Foundation, Switzerland, the Novartis Foundation, Switzerland, the Swissheart Foundation, the Helmut Horten Foundation, Switzerland, the EMDO Foundation, Switzerland, the Iten-Kohaut Foundation/University Hospital Zurich Foundation, Switzerland, and the LOOP-Zurich, Switzerland. KA has received a research grant from the Swiss Academy of Medical Sciences and the Gottfried and Julia Bangerter-Rhyner-Foundation, Switzerland. SB was supported by the UZH Foundation, Switzerland, and the Swissheart Foundation. AH was supported by the UZH Foundation, Switzerland. RS received research grants from the Swiss National Foundation (No 320030_169379), the Research Fund of the University Basel, the Scientific Society Basel, and the Gottfried Julia Bangerter-Rhyner Foundation. He received personal grants from UCB-pharma and holds stocks from Novartis, Roche, Alcon, and Johnson & Johnson.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
CG has received speakers’ fees from Sanofi Genzyme, travel support from Siemens Healthineers, and research support from the Novartis Foundation, Switzerland, and Bayer Pharmaceuticals. The Department of Nuclear Medicine, University Hospital Zurich, holds a research contract with GE Healthcare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Todorov, A., Kaufmann, F., Arslani, K. et al. Gender differences in the provision of intensive care: a Bayesian approach. Intensive Care Med 47, 577–587 (2021). https://doi.org/10.1007/s00134-021-06393-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-021-06393-3