Abstract
Purpose
Data on the benefit or or harmful effects of oxygen level on ischemic reperfusion injuries in cardiac surgery are insufficient. We hypothesized that hyperoxia during cardiopulmonary bypass decreases the incidence of postoperative atrial fibrillation (POAF) and ventricular fibrillation, and therefore decreases cardiovascular morbidity (CARDIOX study).
Methods
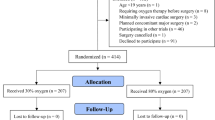
An open-label, randomized clinical trial including adults undergoing elective cardiac surgery, i.e. cardiopulmonary bypass (CPB) randomized 1:1 to an intervention group or standard group at two French University Hospitals from June 2016 to October 2018. The intervention consisted in delivering of an inspired fraction of oxygen of one to one during CPB. The standard care consisted in delivering oxygen to achieve a partial arterial blood pressure less than 150 mmHg. The primary endpoint was the occurrence of POAF and/or ventricular tachycardia/ventricular fibrillation (VT/VF) within the 15 days following cardiac surgery. The secondary endpoint was the occurrence of major adverse cardiovascular events (MACCE: in-hospital mortality, stroke, cardiac arrest, acute kidney injury, and mesenteric ischemia).
Results
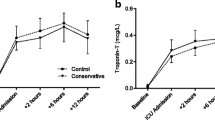
330 patients were randomly assigned to either the intervention group (n = 161) or the standard group (n = 163). Mean PaO2 was 447 ± 98 mmHg and 161 ± 60 mmHg during CPB, for the intervention and standard group (p < 0.0001) respectively. The incidence of POAF or VT/VF were similar in the intervention group and the standard group (30% [49 of 161 patients] and 30% [49 of 163 patients], absolute risk reduction 0.4%; 95% CI, − 9.6–10.4; p = 0.94). MACCE was similar between groups with, an occurrence of 24% and 21% for the intervention group and the standard groups (absolute risk reduction 3.4%; 95% CI, − 5.7–12.5; p = 0.47) respectively. After adjustment, the primary and secondary endpoints remained similar for both groups.
Conclusion
Hyperoxia did not decrease POAF and cardiovascular morbidity following cardiac surgery with CPB.
Clinicaltrial.gov identifier
NCT02819739.


Similar content being viewed by others
References
D’Agostino RS, Jacobs JP, Badhwar V et al (2018) The society of thoracic surgeons adult cardiac surgery database: 2018 update on outcomes and quality. Ann Thorac Surg 105:15–23. https://doi.org/10.1016/j.athoracsur.2017.10.035
Murphy GS, Hessel EA, Groom RC (2009) Optimal perfusion during cardiopulmonary bypass: an evidence-based approach. Anesth Analg 108:1394–1417. https://doi.org/10.1213/ane.0b013e3181875e2e
Heinrichs J, Grocott HP (2018) Pro: hyperoxia should be used during cardiac surgery. J Cardiothorac Vasc Anesth. https://doi.org/10.1053/j.jvca.2018.02.015
Thomson AJ, Drummond GB, Waring WS et al (2006) Effects of short-term isocapnic hyperoxia and hypoxia on cardiovascular function. J Appl Physiol 101:809–816. https://doi.org/10.1152/japplphysiol.01185.2005
Farquhar H, Weatherall M, Wijesinghe M et al (2009) Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J 158:371–377. https://doi.org/10.1016/j.ahj.2009.05.037
Chu DK, Kim LH-Y, Young PJ et al (2018) Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet 391:1693–1705. https://doi.org/10.1016/S0140-6736(18)30479-3
Tähepold P, Valen G, Starkopf J et al (2001) Pretreating rats with hyperoxia attenuates ischemia-reperfusion injury of the heart. Life Sci 68:1629–1640
Tähepõld P, Ruusalepp A, Li G et al (2002) Cardioprotection by breathing hyperoxic gas-relation to oxygen concentration and exposure time in rats and mice. Eur J Cardiothorac Surg 21:987–994
Foadoddini M, Esmailidehaj M, Mehrani H et al (2011) Pretreatment with hyperoxia reduces in vivo infarct size and cell death by apoptosis with an early and delayed phase of protection. Eur J Cardiothorac Surg 39:233–240. https://doi.org/10.1016/j.ejcts.2010.05.036
Heinrichs J, Lodewyks C, Neilson C et al (2018) The impact of hyperoxia on outcomes after cardiac surgery: a systematic review and narrative synthesis. Can J Anaesth 65:923–935. https://doi.org/10.1007/s12630-018-1143-x
Toulouse E, Masseguin C, Lafont B et al (2018) French legal approach to clinical research. Anaesth Crit Care Pain Med 37:607–614. https://doi.org/10.1016/j.accpm.2018.10.013
Jammer I, Wickboldt N, Sander M et al (2015) Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol 32:88–105. https://doi.org/10.1097/EJA.0000000000000118
Thygesen K, Alpert JS, Jaffe AS et al (2019) Fourth universal definition of myocardial infarction (2018). Eur Heart J 40:237–269. https://doi.org/10.1093/eurheartj/ehy462
Nashef SA, Roques F, Michel P et al (1999) European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 16:9–13. https://doi.org/10.1016/s1010-7940(99)00134-7
Echahidi N, Pibarot P, O’Hara G, Mathieu P (2008) Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol 51:793–801. https://doi.org/10.1016/j.jacc.2007.10.043
LaPar DJ, Speir AM, Crosby IK et al (2014) Postoperative atrial fibrillation significantly increases mortality, hospital readmission, and hospital costs. Ann Thorac Surg 98:527–533. https://doi.org/10.1016/j.athoracsur.2014.03.039
Aranki SF, Shaw DP, Adams DH et al (1996) Predictors of atrial fibrillation after coronary artery surgery. Current trends and impact on hospital resources. Circulation 94:390–397
Jeong E-M, Liu M, Sturdy M et al (2012) Metabolic stress, reactive oxygen species, and arrhythmia. J Mol Cell Cardiol 52:454–463. https://doi.org/10.1016/j.yjmcc.2011.09.018
Tsoporis JN, Fazio A, Rizos IK et al (2018) Increased right atrial appendage apoptosis is associated with differential regulation of candidate MicroRNAs 1 and 133A in patients who developed atrial fibrillation after cardiac surgery. J Mol Cell Cardiol 121:25–32. https://doi.org/10.1016/j.yjmcc.2018.06.005
Roffe C, Nevatte T, Sim J et al (2017) Effect of routine low-dose oxygen supplementation on death and disability in adults with acute stroke: the stroke oxygen study randomized clinical trial. JAMA 318:1125. https://doi.org/10.1001/jama.2017.11463
Hofmann R, James SK, Jernberg T et al (2017) Oxygen therapy in suspected acute myocardial infarction. N Engl J Med 377:1240–1249. https://doi.org/10.1056/NEJMoa1706222
Smit B, Smulders YM, de Waard MC et al (2016) Moderate hyperoxic versus near-physiological oxygen targets during and after coronary artery bypass surgery: a randomised controlled trial. Crit Care 20:55. https://doi.org/10.1186/s13054-016-1240-6
Inoue T, Ku K, Kaneda T et al (2002) Cardioprotective effects of lowering oxygen tension after aortic unclamping on cardiopulmonary bypass during coronary artery bypass grafting. Circ J 66:718–722
Abdel-Rahman U, Aybek T, Moritz A et al (2003) Graded reoxygenation limits lipid peroxidation during surgical reperfusion. Med Sci Monit 9:389–391
Spiess BD (2011) Critical oxygen delivery: the crux of bypass with a special look at the microcirculation. J Extra Corpor Technol 43:P10–P16
Wanderer JP, Rathmell JP (2017) Cardiopulmonary bypass, renal oxygenation, & acute kidney injury. Anesthesiology 126:A21. https://doi.org/10.1097/ALN.0000000000001503
Lannemyr L, Bragadottir G, Krumbholz V et al (2017) Effects of cardiopulmonary bypass on renal perfusion, filtration, and oxygenation in patients undergoing cardiac surgery. Anesthesiology 126:205–213. https://doi.org/10.1097/ALN.0000000000001461
Hafner S, Beloncle F, Koch A et al (2015) Hyperoxia in intensive care, emergency, and peri-operative medicine: Dr. Jekyll or Mr. Hyde? A 2015 update. Ann Intensive Care 5:42. https://doi.org/10.1186/s13613-015-0084-6
Asfar P, Singer M, Radermacher P (2015) Understanding the benefits and harms of oxygen therapy. Intensive Care Med 41:1118–1121. https://doi.org/10.1007/s00134-015-3670-z
Acknowledgements
Data were collected by representatives of Clinical Research Divisions of Amiens (Estelle Josse) and Dijon University Hospital (Clémence Beauvalot). The first draft of the manuscript was written by Dr Osama Abou-Arab, Dr Pierre Huette and Pr Pierre-Grégoire Guinot with review and revision by the others authors. Statistical analysis was performed by Mr Momar Diouf. The authors would like to thank CARDIOX participating centers: Centre hospitalier universitaire de Picardie (Yazine Mahjoub, MD, PhD; Mathieu Guilbart, MD; Patricia Besserve, MD; Beatris Labont, MD; Abdel Hchikat, MD; Amar Ben-Ammar, MD; Hervé Dupont, MD, PhD; Thierry Caus, MD, PhD; Jean-Paul Remadi, MD) and Centre hospitalier universitaire de Dijon (Anis Missaoui, MD; Omar Ellouze, MD; Tiberiu Constandache, MD; Sandrine Grosjean, MD; Vivien Berthoud, MD; Jean-Philippe Parthiot, MD; Jean-Pierre Merle, MD).
Funding
The study was sponsored by Amiens University Hospital.
Author information
Authors and Affiliations
Contributions
OAA: study design, performing the procedure, writing the first manuscript and revising the manuscript; PH: study design, performing the procedure and revising the manuscript; PGG: study design, performing the procedure, and revising the manuscript; MD: statistical analysis; EL: study design and revising the manuscript; CB: performing the procedure; EJ: data collection; CB: performing the procedure; all the authors: revision and final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflicts of interest
All authors report no conflict of interest.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the local research ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abou-Arab, O., Huette, P., Martineau, L. et al. Hyperoxia during cardiopulmonary bypass does not decrease cardiovascular complications following cardiac surgery: the CARDIOX randomized clinical trial. Intensive Care Med 45, 1413–1421 (2019). https://doi.org/10.1007/s00134-019-05761-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05761-4