Abstract
Purpose
Muscle wasting is common amongst patients with persistent critical illness and associated with increased urea production, but reduced creatinine production. We hypothesised that elevated urea:creatinine ratio would provide a biochemical signature of muscle catabolism and characterise prolonged intensive care (ICU) admissions after major trauma.
Methods
Using pre-specified hypotheses, we analysed two existing data sets of adults surviving ≥ 10 days following admission to ICU after major trauma. We analysed trauma-ICU admissions to the major trauma centre serving the North East London and Essex Trauma Network, with a verification cohort of trauma-ICU cases from the MIMIC-III database. We compared serum urea, creatinine, and urea:creatinine ratio (ratio of concentrations in mmol/L) between patients with persistent critical illness (defined as ICU stay of ≥ 10 days) and those discharged from ICU before day 10. In a sub-group undergoing sequential abdominal computerised tomography (CT), we measured change in cross-sectional muscle area (psoas muscle at L4 vertebral level and total muscle at L3 level) and assessed for relationships with urea:creatinine ratio and ICU stay. Results are provided as median [interquartile range].
Results
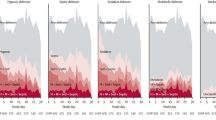
We included 1173 patients between February 1st, 2012 and May 1st, 2016. In patients with ICU stay ≥ 10 days, day 10 urea:creatinine ratio had increased by 133% [72–215], from 62 [46–78] to 141 [114–178], p < 0.001; this rise was larger (p < 0.001) than in patients discharged from ICU before day 10, 59% [11–122%], 61 [45–75] to 97 [67–128], p < 0.001. A similar separation in trajectory of urea:creatinine ratio was observed in 2876 trauma-ICU admissions from MIMIC-III. In 107 patients undergoing serial CTs, decrease in L4 psoas and L3 muscle cross-sectional areas between CTs significantly correlated with time elapsed (R2 = 0.64 and R2 = 0.59, respectively). Rate of muscle decrease was significantly greater (p < 0.001 for interaction terms) in 53/107 patients with the second CT during evolving, current or recent persistent critical illness. In this group, at the second CT urea:creatinine ratio negatively correlated with L4 psoas and L3 muscle cross-sectional areas (R2 0.39, p < 0.001 and 0.44, p < 0.001).
Conclusion
Elevated urea:creatinine ratio accompanies skeletal muscle wasting representing a biochemical signature of persistent critical illness after major trauma. If prospectively confirmed, urea:creatinine ratio is a potential surrogate of catabolism to examine in epidemiological and interventional studies.



Similar content being viewed by others
References
Iwashyna TJ, Hodgson CL, Pilcher D, Bailey M, van Lint A, Chavan S, Bellomo R (2016) Timing of onset and burden of persistent critical illness in Australia and New Zealand: a retrospective, population-based, observational study. Lancet Respir Med 4:566–573
Bagshaw SM, Stelfox HT, Iwashyna TJ, Bellomo R, Zuege D, Wang X (2018) Timing of onset of persistent critical illness: a multi-centre retrospective cohort study. Intensive Care Med 44:2134–2144
Iwashyna TJ, Viglianti EM (2018) Patient and population-level approaches to persistent critical illness and prolonged intensive care unit stays. Crit Care Clin 34:493–500
Viglianti EM, Kramer R, Admon AJ, Sjoding MW, Hodgson CL, Bellomo R, Iwashyna TJ (2018) Late organ failures in patients with prolonged intensive care unit stays. J Crit Care 46:55–57
Brohi K, Gruen RL, Holcomb JB (2019) Why are bleeding trauma patients still dying? Intensive Care Med 45:709–711
Mira JC, Gentile LF, Mathias BJ, Efron PA, Brakenridge SC, Mohr AM, Moore FA, Moldawer LL (2017) Sepsis pathophysiology, chronic critical illness, and persistent inflammation-immunosuppression and catabolism syndrome. Crit Care Med 45:253–262
Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S (2011) Long-term survival of adult trauma patients. JAMA 305:1001–1007
Friedrich O, Reid MB, Van den Berghe G, Vanhorebeek I, Hermans G, Rich MM, Larsson L (2015) The sick and the weak: neuropathies/myopathies in the critically ill. Physiol Rev 95:1025–1109
Stortz JA, Mira JC, Raymond SL, Loftus TJ, Ozrazgat-Baslanti T, Wang Z, Ghita GL, Leeuwenburgh C, Segal MS, Bihorac A, Brumback BA, Mohr AM, Efron PA, Moldawer LL, Moore FA, Brakenridge SC (2018) Benchmarking clinical outcomes and the immunocatabolic phenotype of chronic critical illness after sepsis in surgical intensive care unit patients. J Trauma Acute Care Surg 84:342–349
Gentile LF, Cuenca AG, Efron PA, Ang D, Bihorac A, McKinley BA, Moldawer LL, Moore FA (2012) Persistent inflammation and immunosuppression: a common syndrome and new horizon for surgical intensive care. J Trauma Acute Care Surg 72:1491–1501
Van den Berghe G, de Zegher F, Baxter RC, Veldhuis JD, Wouters P, Schetz M, Verwaest C, Van der Vorst E, Lauwers P, Bouillon R, Bowers CY (1998) Neuroendocrinology of prolonged critical illness: effects of exogenous thyrotropin-releasing hormone and its combination with growth hormone secretagogues. J Clin Endocrinol Metab 83:309–319
Efron PA, Mohr AM, Bihorac A, Horiguchi H, Hollen MK, Segal MS, Baker HV, Leeuwenburgh C, Moldawer LL, Moore FA, Brakenridge SC (2018) Persistent inflammation, immunosuppression, and catabolism and the development of chronic critical illness after surgery. Surgery 164:178–184
Prowle JR, Kolic I, Kirwan C (2015) SP243 divergent changes in serum creatinine and urea in survivors of prolonged critical illness. Nephrol Dial Transplant 30:iii458–iii459
Astin R, Puthucheary Z (2014) Anaemia secondary to critical illness: an unexplained phenomenon. Extrem Physiol Med 3:4
Póvoa P (2002) C-reactive protein: a valuable marker of sepsis. Intensive Care Med 28:235–243
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Leliefeld PH, Wessels CM, Leenen LP, Koenderman L, Pillay J (2016) The role of neutrophils in immune dysfunction during severe inflammation. Crit Care 20:73
Boomer JS, To K, Chang KC, Takasu O, Osborne DF, Walton AH, Bricker TL, Jarman SD, Kreisel D, Krupnick AS, Srivastava A, Swanson PE, Green JM, Hotchkiss RS (2011) Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA 306:2594–2605
Azab B, Camacho-Rivera M, Taioli E (2014) Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PLoS One 9:e112361
Nicholson JP, Wolmarans MR, Park GR (2000) The role of albumin in critical illness. Br J Anaesth 85:599–610
Haines RW, Lin SP, Hewson R, Kirwan CJ, Torrance HD, O’Dwyer MJ, West A, Brohi K, Pearse RM, Zolfaghari P, Prowle JR (2018) Acute kidney injury in trauma patients admitted to critical care: development and validation of a diagnostic prediction model. Sci Rep 8:3665
Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG (2016) MIMIC-III, a freely accessible critical care database. Sci Data 3:160035
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, Initiative S (2007) Strengthening the Reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology 18:805–835
Saour M, Klouche K, Deras P, Damou A, Capdevila X, Charbit J (2016) Assessment of modification of diet in renal disease equation to predict reference serum creatinine value in severe trauma patients: lessons from an observational study of 775 cases. Ann Surg 263:814–820
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE (2008) A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab 33:997–1006
Gunst J, Vanhorebeek I, Casaer MP, Hermans G, Wouters PJ, Dubois J, Claes K, Schetz M, Van den Berghe G (2013) Impact of early parenteral nutrition on metabolism and kidney injury. J Am Soc Nephrol 24:995–1005
Prowle JR, Kolic I, Purdell-Lewis J, Taylor R, Pearse RM, Kirwan CJ (2014) Serum creatinine changes associated with critical illness and detection of persistent renal dysfunction after AKI. Clin J Am Soc Nephrol 9:1015–1023
Puthucheary ZA, Astin R, McPhail MJW, Saeed S, Pasha Y, Bear DE, Constantin D, Velloso C, Manning S, Calvert L, Singer M, Batterham RL, Gomez-Romero M, Holmes E, Steiner MC, Atherton PJ, Greenhaff P, Edwards LM, Smith K, Harridge SD, Hart N, Montgomery HE (2018) Metabolic phenotype of skeletal muscle in early critical illness. Thorax 73:926–935
Wyss M, Kaddurah-Daouk R (2000) Creatine and creatinine metabolism. Physiol Rev 80:1107–1213
Thongprayoon C, Cheungpasitporn W, Kashani K (2016) Serum creatinine level, a surrogate of muscle mass, predicts mortality in critically ill patients. J Thorac Dis 8:E305–E311
Wang ZM, Gallagher D, Nelson ME, Matthews DE, Heymsfield SB (1996) Total-body skeletal muscle mass: evaluation of 24-h urinary creatinine excretion by computerized axial tomography. Am J Clin Nutr 63:863–869
Van den Berghe G (2016) On the neuroendocrinopathy of critical illness. perspectives for feeding and novel treatments. Am J Respir Crit Care Med 194:1337–1348
Gamrin-Gripenberg L, Sundström-Rehal M, Olsson D, Grip J, Wernerman J, Rooyackers O (2018) An attenuated rate of leg muscle protein depletion and leg free amino acid efflux over time is seen in ICU long-stayers. Crit Care 22:13
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS, Group CCCT (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–693
Arihan O, Wernly B, Lichtenauer M, Franz M, Kabisch B, Muessig J, Masyuk M, Lauten A, Schulze PC, Hoppe UC, Kelm M, Jung C (2018) Blood urea nitrogen (BUN) is independently associated with mortality in critically ill patients admitted to ICU. PLoS One 13:e0191697
Faisst M, Wellner UF, Utzolino S, Hopt UT, Keck T (2010) Elevated blood urea nitrogen is an independent risk factor of prolonged intensive care unit stay due to acute necrotizing pancreatitis. J Crit Care 25:105–111
Beier K, Eppanapally S, Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB (2011) Elevation of blood urea nitrogen is predictive of long-term mortality in critically ill patients independent of “normal” creatinine. Crit Care Med 39:305–313
Uchino S, Bellomo R, Goldsmith D (2012) The meaning of the blood urea nitrogen/creatinine ratio in acute kidney injury. Clin Kidney J 5:187–191
Rachoin JS, Daher R, Moussallem C, Milcarek B, Hunter K, Schorr C, Abboud M, Henry P, Weisberg LS (2012) The fallacy of the BUN:creatinine ratio in critically ill patients. Nephrol Dial Transplant 27:2248–2254
Yende S, D’Angelo G, Kellum JA, Weissfeld L, Fine J, Welch RD, Kong L, Carter M, Angus DC, Investigators G (2008) Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med 177:1242–1247
Acknowledgements
Royal London ACCU office, Royal London Hospital Trauma audit team, Dr. Bhavi Trivedi (powerInsight access), Prof Karim Brohi, Mr. Nigel Tai and Mr. Wayne Sapsford (Collector Trauma database access).
Author information
Authors and Affiliations
Contributions
All authors reviewed and approved the final manuscript. JP and PZ were responsible for the study concept and RH, PZ, ZP, and JP for study design. Data extraction was undertaken by RH, PZ, and JP. RH, PZ, ZP, and JP were responsible for data analysis and JP, PZ, ZP, YW, and RP provided comments and review of draft analyses.
Corresponding author
Ethics declarations
Conflicts of interest
ZP is on specialist advisor boards for GlaxoSmithkline, Fresunius Kabi and Faraday Pharmaceuticals and has given lectures and/or performed consultancy work for Lyric Pharmaceuticals, Faraday Pharmaceuticals, Orion Pharmaceuticals and Nestle. RP holds research grants, has given lectures and/or performed consultancy work for BBraun, GlaxoSmithkline, Medtronic, Intersurgical and Edwards Lifesciences. JP has given lectures and/or performed consultancy work for Fresenius Medical, Baxter, Nikkiso, Biomerieux, Abbott, Medibeacon and Quark Pharma.
Data sharing
As this study was carried out on the basis of analysis of routinely collected data by the usual care team, consent for sharing of anonymised patient level data is not available. The investigators will consider proposals for sub-analyses on a collaborative basis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haines, R.W., Zolfaghari, P., Wan, Y. et al. Elevated urea-to-creatinine ratio provides a biochemical signature of muscle catabolism and persistent critical illness after major trauma. Intensive Care Med 45, 1718–1731 (2019). https://doi.org/10.1007/s00134-019-05760-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05760-5