Abstract
Purpose
Long-term data are urgently needed in children after intensive care. The aim of this study was to measure health-related quality of life 6 years after intensive care in a paediatric intensive care population.
Methods
This national, multicentre study enrolled all children and young people admitted to intensive care units (ICUs) in Finland in 2009 and 2010. The data concerning ICU stay were collected retrospectively from the ICU data registries and combined with prospective data from Paediatric Quality of Life Inventory (PedsQL 4.0) questionnaires, the generic 15D, 16D or 17D instrument, and data regarding children’s chronic diagnoses and need for healthcare support.
Results
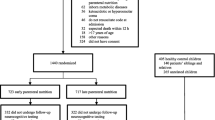
The questionnaires were answered by 1109 of 3682 living children and adolescents admitted to an ICU, response rate was 30.1%. Among the responders, 90 children (8.4%) had poor (under − 2 SD) PedsQL scores. Children with low scores had a higher rate of chronic diagnoses (94.4% vs. 47.6%), medication on a daily basis (78.7% vs. 29.4%) and a greater need for healthcare services (97.7% vs. 82.2%) than those with normal scores. Diagnoses associated with poor quality of life were asthma, epilepsy, cerebral palsy and other neurological diseases, chromosomal alterations, cancer and long-term pain. These children were mostly admitted electively, and less frequently on an emergency basis, but no other significant differences were found during the intensive care stay.
Conclusions
The long-term quality of life after paediatric intensive care is good for the majority of children and young people, and it is dependent on the number of chronic diagnoses and the burden of the chronic disease, especially neurological diseases.



Similar content being viewed by others
References
Aspesberro F, Mangione-Smith R, Zimmerman JJ (2015) Health-related quality of life following pediatric critical illness. Intensive Care Med 41:1235–1246. https://doi.org/10.1007/s00134-015-3780-7
Herrup EA, Wieczorek B, Kudchadkar SR (2017) Characteristics of post intensive care syndrome in survivors of pediatric critical illness: a systematic review. World J Crit Care Med 6:124–134
Ong C, Lee JH, Leow MKS, Puthucheary ZA (2016) Functional outcomes and physical impairments in pediatric critical care survivors: a scoping review. Pediatr Crit Care Med 17:e247–e259
Pollack MM, Holubkov R, Funai T et al (2014) Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med 15:821–827
Namachivayam P, Taylor A, Montague T, Moran K, Barrie J, Delzoppo C, Butt W (2012) Long-stay children in intensive care: long-term functional outcome and quality of life from a 20-yr institutional study. Pediatr Crit Care Med 13:520–528. https://doi.org/10.1097/PCC.0b013e31824fb989
Conlon NP, Breatnach C, O’Hare BP, Mannion DW, Lyons BJ (2009) Health-related quality of life after prolonged pediatric intensive care unit stay. Pediatr Crit Care Med 10:41–44. https://doi.org/10.1097/PCC.0b013e31819371f6
Taylor A, Butt W, Ciardulli M (2003) The functional outcome and quality of life of children after admission to an intensive care unit. Intensive Care Med 29:795–800
Pinto N (2017) Long-term function after critical illness: results from the survivor outcomes study. Pediatr Crit Care Med. https://doi.org/10.1097/pcc.0000000000001070
Choong K, Fraser D, AlHarbi S et al (2018) Functional recovery in critically ill children, the “WeeCover” multicenter study. Pediatr Crit Care Med 19:145–154
Rennick JE, Childerhose JE (2015) Redefining success in the PICU: new patient populations shift targets of care. Pediatrics 135:e289–e291
Edwards JD, Houtrow AJ, Vasilevskis EE, Rehm RS, Markovitz BP, Graham RJ, Dudley RA (2012) Chronic conditions among children admitted to US pediatric intensive care units: their prevalence and impact on risk for mortality and prolonged length of stay. Crit Care Med 40:2196–2203
Varni JW, Burwinkle TM, Seid M, Skarr D (2003) The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 3:329–341
Sintonen H (2001) The 15D instrument of health-related quality of life: properties and applications. Ann Med 33:328–336
Apajasalo M, Sintonen H, Holmberg C et al (1996) Quality of life in early adolescence: a sixteen-dimensional health-related measure (16D). Qual Life Res 5:205–221
Apajasalo M, Rautonen J, Holmberg C et al (1996) Quality of life in pre-adolescence: a 17-dimensional health-related measure (17D). Qual Life Res 5:532–538
Aspesberro F, Fesinmeyer MD, Zhou C, Zimmerman JJ, Mangione-Smith R (2016) Construct validity and responsiveness of the pediatric quality of life inventory 4.0 generic core scales and infant scales in the PICU. Pediatr Crit Care Med 17:e272–e279
Colville GA, Pierce CM (2013) Children’s self-reported quality of life after intensive care treatment. Pediatr Crit Care Med 14:e85–e92
Suominen PK, Vahatalo R, Sintonen H, Haverinen A, Roine RP (2011) Health-related quality of life after a drowning incident as a child. Resuscitation 82:1318–1322
Peltoniemi OM, Rautiainen P, Kataja J, Ala-Kokko T (2016) Pediatric intensive care in PICUs and adult ICUs: a 2-year cohort study in Finland. Pediatr Crit Care Med 17:43–49. https://doi.org/10.1097/PCC.0000000000000587
Mestrovic J, Kardum G, Sustic A, Polic B, Mestrovic M, Markic J, Zanchi J (2007) Neurodevelopmental disabilities and quality of life after intensive care treatment. J Paediatr Child Health 43:673–67622
Gemke RJ, Bonsel GJ, van Vught AJ (1995) Long-term survival and state of health after paediatric intensive care. Arch Dis Child 43:673–676
Odetola FO, Gebremariam A, Davis MM (2010) Comorbid illnesses among critically ill hospitalized children: impact on hospital resource use and mortality, 1997–2006. Pediatr Crit Care Med 11:457–463. https://doi.org/10.1097/PCC.0b013e3181c514fa
Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM (2010) Increasing prevalence of medically complex children in US hospitals. Pediatrics 126:638–646
Morrison AL, Gillis J, O’Connell AJ, Schell DN, Dossetor DR, Mellis C (2002) Quality of life of survivors of pediatric intensive care. Pediatr Crit Care Med 3:1–5
Gunn ME, Mort S, Arola M, Taskinen M, Riikonen P, Mottonen M, Lahteenmaki PM (2016) Quality of life and late-effects among childhood brain tumor survivors: a mixed method analysis. Psychooncology 6:677–683
Mort S, Salantera S, Matomaki J, Salmi TT, Lahteenmaki PM (2011) Cancer related factors do not explain the quality of life scores for childhood cancer survivors analysed with two different generic HRQL instruments. Cancer Epidemiol 35:202–210
Solans M, Pane S, Estrada M et al (2008) Health-related quality of life measurement in children and adolescents: a systematic review of generic and disease-specific instruments. Value Health 11:742–764
Kenzik KM, Tuli SY, Revicki DA, Shenkman EA, Huang I (2014) Comparison of 4 pediatric health-related quality-of-life instruments: a study on a medicaid population. Med Decis Mak 34:590–602
Acknowledgements
This study was funded in part by the Päivikki and Sakari Sohlberg Foundation and the Alma and K. A. Snellman Foundation. We acknowledge the collaborators of participating units for delivering the patient identification data: Saija Rissanen, Kuopio University Hospital; Sari Karlsson, Tampere University Hospital; Ilkka Soikkeli, Lapland Central Hospital; Tuula Pelimanni, Kemi Central Hospital; Sirkku Malinen, Kainuu Central Hospital; Tadeusz Kaminski, Keski-Pohjanmaa Central Hospital; Simo-Pekka Koivisto, Vaasa Central Hospital; Kirsi Nuolivirta, Seinäjoki Central Hospital; Mikko Reilama, Central Finland Central Hospital; Pekka Saastamoinen, Savonlinna Central Hospital; Matti Reinikainen, North Karelian Central Hospital; Heikki Laine, Mikkeli Central Hospital, Jan Adamski, Satakunta Central Hospital; Mikko Huhtanen, Kanta-Häme Central Hospital; Mikko Lavonius, Päijät-Häme Central Hospital; Seppo Hovilehto, South Karelian Central Hospital; Kati Wahlman, Kymeenlaakso Central Hospital; Leena Soininen, Meilahti Central Hospital; and Tero Varpula, Jorvi Central Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Kyösti, E., Ala-Kokko, T.I., Ohtonen, P. et al. Factors associated with health-related quality of life 6 years after ICU discharge in a Finnish paediatric population: a cohort study. Intensive Care Med 44, 1378–1387 (2018). https://doi.org/10.1007/s00134-018-5296-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5296-4