Abstract
Background
Glucose control (GC) with insulin decreases morbidity and mortality of critically ill patients. In this study we investigated GC performance over time during implementation of GC strategies within three intensive care units (ICUs) and in routine clinical practice.
Methods
All adult critically ill patients who stayed for >24 h between 1999 and 2007 were included. Effects of implementing local GC guidelines and guideline revisions on effectiveness/efficiency-related indicators, safety-related indicators, and protocol-related indicators were measured.
Results
Data of 17,111 patient admissions were evaluated, with 714,141 available blood glucose levels (BGL) measurements. Mean BGL, time to reach target, hyperglycemia index, sampling frequency, percentage of hyperglycemia events, and in-range measurements statistically changed after introducing GC in all ICUs. The introduction of simple rules on GC had the largest effect. Subsequent changes in the protocol had a smaller effect than the introduction of the protocol itself. As soon as the protocol was introduced, in all ICUs the percentage of hypoglycemia events increased. Various revisions were implemented to reduce hypoglycemia events, but levels never returned to those from pre-implementation. More intensive implementation strategies including the use of a decision support system resulted in better control of the process.
Conclusion
There are various strategies to achieve GC in routine clinical practice but with variable success. All of them were associated with an increase in hypoglycemia events, but GC was never stopped. Instead, these events have been accepted and managed. Statistical process control is a useful tool for monitoring phenomena over time and captures within-institution changes.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Hyperglycemia is frequently encountered in critically ill patients [1, 2]. The underlying physiology of hyperglycemia that drives mortality, independently of glucose control (GC), has been described [3, 4]. GC aiming at normoglycemia [i.e., blood glucose level (BGL) of 80–110 mg/dl, frequently referred to as “tight glycemic control”] decreased morbidity and mortality of critically ill patients in two randomized controlled trials [5, 6]. Recent published meta-analysis [7, 8] could not confirm the benefits of GC, but there are some important methodological concerns about this study [9, 10] and many intensive care units (ICUs) still use GC in their routine clinical practice. Although some studies showed that the implementation of GC with insulin came with the risk of hypoglycemia [5, 6, 11–13], others did not [14–18]. Some studies therefore advise maintaining a BGL <150 mg/dl [19–21]. Another recent randomized controlled trial showed that maintaining BGL <180 mg/dl is superior to adhering to the tight glycemic control in terms of mortality and morbidity [22]. However, this result should be interpreted in the context of the specific implemented guideline and the level of compliance with it. This context is important because the quality of GC and outcome are directly linked [1, 23, 24].
Determining how and for whom GC is safe and effective remains quite elusive [25–27]. Implementing GC as well as the performance of the GC process itself is of great importance in intensive care medicine. To measure GC performance one has to determine and define adequate performance indicators and analyze these indicators over time. This implies monitoring the implementation process and determining whether GC is truly applied and functioning at a consistent and acceptable level. Statistical process control (SPC) is a powerful tool for quality measurement of phenomena over time and the improvement of processes [28].
Our objective was to study GC performance over time during implementation of this strategy in three different ICUs. First, we described and analyzed the performance of GC in the early stage of GC but before implementation of local guidelines, and after the implementation of a written guideline in each center. Second, we analyzed differences between simple and complex guidelines, and between non-computerized and computerized GC. In addition, we described the influence of concerns of clinicians and nurses regarding the safety of GC.
Methods
Study locations
Collection of data was performed in three closed-format mixed medical-surgical ICUs in the Netherlands. ICU-A is a 30-bed ICU of an academic hospital. ICU-B is a 10-bed ICU of a nonacademic teaching hospital. ICU-C is an 18-bed ICU of a nonacademic teaching hospital. In ICU-A and ICU-C, physicians are constantly present.
ICU-A (March 2002) and ICU-C (April 2001) were equipped with a patient data management system (PDMS). The PDMS can display and process all BGLs directly after their measurement with a maximum delay of 1 min.
Local glucose control guidelines
Tables 1 and 2 show the guideline characteristics and changes in them over time. Note that for severe hypoglycemia events, the guidelines recommend stopping insulin infusion as well as injecting glucose.
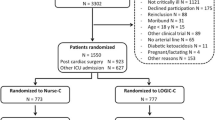
Patients
All adult critically ill patients who stayed for >24 h between 1999 and 2007 were included. The hospital information system and PDMS were searched for all records on BGL for these patients. The first BGLs directly after ICU admittance were excluded from the final analysis because we considered them not to be influenced by any ICU regimen.
Performance indicators and definitions
The most common performance indicators [29] were selected to show the quality of glucose regulation in the three ICUs. The indicators, described in Table S1 in the electronic supplementary material (ESM), were categorized in three groups: effectiveness/efficiency-related indicators (mean BGL, BGL within predefined targets, and time to reach target), safety-related indicators (severe hypoglycemia, hyperglycemia, and hyperglycemia index), and protocol-related indicators (sampling frequency).
Statistical analysis
We used the SPC technique, described in the ESM, and the XMR control chart [30] to construct and analyze the processes. Due to big subgroup size and the increasing chance of a false-positive result, we used the XMR chart in place of attribute charts [31, 32]. The quality indicators that we chose were calculated per quarter and plotted as points on the XMR chart. The mean of the points before GC implementation was calculated along with the ±3 sigma limits. To determine whether a change in the process occurs further along the time axis, the mean and process control limits were extrapolated over the entire study period. Because the time of intervention is known and because the process is stable (i.e., not “out of control” according to the SPC rules) before and after the intervention, the mean and process control limits were recalculated in the intervention period. The Kruskal-Wallis H, Mann-Whitney U, and chi-squared tests were used to assess the statistical significance of differences among pre- and post-intervention periods and to compare these results with those of the SPC analysis. All analysis was performed with Systat 12.
Results
Patients
In total 9,392, 2,968, and 4,751 admissions from ICU-A and ICU-B (from 1 January 1999 to 31 September 2007) and ICU-C (from 1 January 2001 to 31 September 2007), respectively, were extracted and analyzed. Table S2 in the ESM shows the patient baseline characteristics including age, gender, APACHE III score, admission type, ICU mortality, and length of stay in each year of study. SPC showed that they were stable and did not change significantly during the study period.
Effectiveness and efficiency of glucose control
Figure 1 shows the quality process control charts for the effectiveness/efficiency-related indicators of GC in the three ICUs. Mean BGL decreased and became “out of process control” (i.e., a change was detected) after implementing the GC guideline in all three ICUs. The introduction of simple rules on GC had the largest effect in ICU-A, since GC became more stable with less variation. Subsequent changes in the guidelines did not have effects as large as the introduction of the guideline itself. Mean BGL in ICU-B was reduced by the introduction of the guideline but the mean BGL still remained higher and less stable from quarter to quarter than in the other two ICUs. Similar to ICU-A, in ICU-C the implementation of the GC guideline had a large effect on BGL, but with the introduction of the computerized decision support system (CDSS) the mean BGL decreased further and GC stabilized.
Control charts of mean BGL, time to reach target range, percentage of BGLs in range predefined in the protocols, and percentage of BGLs between 63 and 150 mg/dl (efficiency-related indicators). An asterisk means that the indicator was not only influenced by performance but also by definition of targets, and that because of the latter sharp changes over time could be recognized. When the data points are, without any special-cause variation, within the process control limits then the process is said to be “in control” and stable. Common rules for distinguishing a special-cause variation (i.e., a structural change): one or more points above or below the process control limit, a run of eight (or seven) or more points on one side of the center line, two out of three consecutive points appearing beyond 2 sigmas on the same side of the center line, a run of eight (or seven) or more points all trending up or down. Because the time of intervention (major changes) is known and because the process was stable (i.e., not “out of control” according to the SPC rules) before and after the intervention, the mean and process control limits are recalculated in the intervention period
The percentage of BGLs within locally defined targets increased after introducing GC guidelines in all three ICUs. In ICU-A, the subsequent revisions in the protocol did not change this percentage. As with mean BGLs, the percentage of BGLs within target in ICU-B changed significantly with the two changes in the protocol. In ICU-C, both the introduction of GC as well as the introduction of the CDSS increased the percentage of BGLs within targets.
Time to reach targets decreased after introducing the first GC guideline in ICU-A and ICU-C. The means of this indicator in ICU-A were better than in ICU-C before introducing the protocol. But in ICU-C after protocol introduction, and especially with CDSS implementation, the mean of this indicator rapidly decreased and eventually it was half of that in ICU-A. After protocol implementation in ICU-B, the mean time to reach target ranges decreased stepwise with changes in the protocol, but was comparable to the other two ICUs with less stability and higher mean.
Safety of glucose control
Process control charts of safety-related quality indicators are shown in Figs. 2 and 3. As soon as the guidelines were introduced, in all three ICUs the percentage of BGL measurements ≤40 mg/dl increased. In ICU-A, the first revision of the guideline decreased both severe and nonsevere hypoglycemia events. In ICU-B, with all changes in the protocol, the incidence of hypoglycemia increased. In ICU-C, these indicators increased after introducing GC and further increased after CDSS implementation. Compared to the other two ICUs, the percentage of BGL measurements ≤40 mg/dl in ICU-B was less stable with more variation from quarter to quarter before the third revision in the GC guideline.
Protocol-related indicator
Mean interval between BGL measurements decreased after introducing the GC guidelines in ICU-A and ICU-C (Fig. 4). In ICU-A this interval was smaller than in ICU-C before introducing the protocol. But after introduction of the guideline in ICU-C, especially with the CDSS implementation, this mean rapidly decreased and was even half of that in ICU-A. With the introduction and subsequent changes of the guideline in ICU-B, the mean interval between BGL measurements decreased, but compared to the other two ICUs, with less stability and with higher means especially before the third revision. Both reductions were statistically significant.
The results of nonparametric and chi-squared tests on the effect of introducing GC and related changes on these indicators were concordant with the SPC results (data not shown).
We used all data from 31 September 2005 till 31 September 2007 because all ICUs declared there were no other interventions that could have affected GC in this period. The SPC charts also showed the processes were stable for all indicators in all three ICUs in this period. Median BGL in ICU-C and ICU-B was significantly lower than ICU-A. The percentage of patients with at least one hypoglycemia event and overall percentage of hypoglycemia and severe hypoglycemia events were significantly higher in ICU-C and ICU-B. Other statistically (and seemingly clinically) significant differences were in BGL measurement interval, and time to reach target, which were lower in ICU-C (Table S3 in the ESM).
Discussion
The effect of introducing GC guidelines and the various implementations on the quality of GC, especially for an extended period of time, is unknown. The implementation strategies of GC ranged from raising awareness to employing a computerized decision support system. In all three ICUs, regardless of strategy, there was a continuous and significant improvement in the effectiveness and efficiency indicators, an increase in hypoglycemic-related indicators, and an increase in BGL measurements. However, the speed of change and the final outcomes differed significantly among the three ICUs.
With SPC, data are plotted and interpreted in a time series rather than merely comparing before and after measures. With this method special causes of variation were easily distinguished from common causes. Process control charts showed which parts of the processes were more stable and also showed the duration of change after each intervention. SPC charts in Figs. 1, 2, 3 and 4 showed the diversity in results for implementing similar protocols in three different centers and reflected a range of “error”, all else being equal, in implementing a protocol with differing interpretations and implementation details. Those wishing to use SPC as a tool for longitudinal self-examination of performance are referred to [31].
This study has three main strengths. First, to our knowledge this is the first report on effects of GC in routine daily clinical practice over an extended period of time. Second, to visualize and make inferences on the longitudinal development of quality indicators, we used the powerful instrument of process control charts from the field of SPC. Third, we studied three different ICUs employing different GC strategies. There are however also limitations to our study. First, we did not perform subgroup analysis (such as surgical vs. medical patients). Second, we did not investigate the influence of GC on clinically relevant endpoints such as survival. However, as GC has been shown to be an evidence-based strategy that decreases morbidity and mortality [5, 6], adherence to this strategy is commonly advocated. Third, the actual adherence to the protocols is unknown. However, the fact that the quality indicators were significantly influenced implies that the protocols are being increasingly followed. Finally, because nutrition data were not available for the whole study period, we could not investigate the possible effect of nutrition on the quality of GC. However, nutrition input is not likely to have changed over the study period within each hospital. In addition, the protocol should be robust to reasonable fluctuations in the given nutritional carbohydrate levels.
Usually routine clinical practice characteristics and limitations are not considered in randomized control trial (RCTs) and guidelines. This is one explanation for the underuse of treatments in routine practice that were beneficial in trials and that are recommended in guidelines. Among tight glycemic control (TGC) studies, some have explicitly considered routine practice issues in their design, e.g., [14, 15, 17]. However, we in addition monitored performance during actual use of the protocol over time with SPC.
Relaxing the GC range to a wider, locally workable target can perhaps be explained by an associated “fear” of hypoglycemia. Brunkhorst et al. showed that the rate of patients with at least one episode of severe hypoglycemia (≤40 mg/dl) was higher in the study group than in the control group (17.0 vs. 4.1%, P<0.001) [11]. Although they reported that no serious adverse events were found, the trial was nonetheless stopped due to the hypoglycemic episodes. Interestingly our results showed that in routine practice, and in contrast to the clinical trials, GC was not stopped although the rate of patients with at least one hypoglycemia event were relatively high even with less tight target ranges (9% in the ICU-B and ICU-C after the last guideline revision). Although concern about increasing the percentage of hypoglycemic patients resulted in terminating the use of the more detailed protocol in ICU-B, thereafter an even tighter target range was used in this ICU, and the percentage of hypoglycemic patients increased even after these revisions. Protocol failure and/or lack of compliance could partly explain this result, but we do not have data to test these hypotheses. Vriesendorp et al. and Chase et al. showed that TGC-induced hypoglycemia was not associated with worse outcome [17, 33], although recent studies have reported such an association [22, 34]. Association of hypoglycemia with worse outcome may be related to the protocols in use. Fear of hypoglycemia and its reputation as being more dangerous than hyperglycemia in the critically ill may well be based on deeply rooted emotional beliefs rather than on evidence [35]. Our study demonstrates that as long as continuous measurement tools are not available, hypoglycemia events are considered acceptable and can be consequently managed.
Our results also showed that any decrease in mean BGL resulted in an increase in the percentage of hypoglycemia events. ICU-C, which eventually had the lowest mean BGL, also had the highest percentage of hypoglycemia events. The complex guidelines and the use of the CDSS, resulting in a mean measurement interval in ICU-C of 120 min, may have led to more early (and possibly more frequent) detection of the hypoglycemia. Also minimum BGL in ICU-A and ICU-B was associated with maximum percentage of hypoglycemia events. Revising the protocol in ICU-A decreased the hypoglycemia events but could not return the level to what it was before implementing GC.
Shortly after the first presentation on TGC in November 2001 [6], there were either no written guidelines in the participating ICUs or the guidelines were very simple and in a development phase. SPC charts showed that awareness of TGC, regardless of the guidelines in place, brought about the maximum changes in the related indicators. However, thereafter there remained little room for improvement. After this stage, stronger interventions, such as more complex protocols and the use of a CDSS, were called upon to bring about change, but the level of change was smaller.
Different strategies were developed to achieve GC in the three ICUs studied. All have managed to reach an acceptable control but with different speeds of change and different variability over time. Both ICUs with detailed written protocols (ICU-A and ICU-C) had better results and more stable processes with lower variability from quarter to quarter than ICU-B. Using a detailed written protocol with clearly defined steps compared to simple rules (ICU-B) seems to help the nurses to make better decisions to control blood glucose.
Our results show that a complex protocol with more steps and detail in ICU-C had improved effects but only after including the CDSS as an intervention. In ICU-C the mean BGL measurement interval also became smaller than in ICU-A after the CDSS. We can conclude that the CDSS influenced the nurses’ behavior by reminding them about the time of the next BGL test. Probably the shorter time between measurements is based on differences between protocols, not the effect of CDSS. However it is unclear whether the beneficial effects of the CDSS are mainly due to the more frequent measurements or due to the complex protocol rules. With the current data we cannot answer this question. In addition, to achieve such a low mean BGL, higher costs (CDSS and more nursing and laboratory utilization) were incurred and patients experienced more hypoglycemia events. Cost-benefit analysis merits more research when aiming at lower mean BGL.
Frequent BGL measurement is a key element in TGC, in order to steer the process in a timely manner [14, 17, 36]. In the three studied ICUs, better results were associated with more frequent measurements. In ICU-A, there were many BGL measurements before introducing GC, since BGL measurements were included with blood gas analysis, even when there was no intention to measure it. This might explain some of the fast improvement in glucose regulation in ICU-A after introducing the guideline and the very small variation in sample interval.
Conclusions
There are different successful strategies to realize GC in routine clinical practice but they have various speeds and implementations. All of the strategies studied here were associated with an increase in hypoglycemia events. More intensive implementation strategies resulted in better control of the process but at the cost of more ICU resources, including the use of a decision support system. SPC is a useful tool for monitoring phenomena over time and allows for capturing within-institution changes. Within quality measurement and/or improvement efforts, SPC can show where the special variations are and where opportunities lie for improving (adherence to) protocols.
References
Krinsley JS (2003) Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc 78:1471–1478
Capes SE, Hunt D, Malmberg K, Gerstein HC (2000) Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 355:773–778
Marik PE, Raghavan M (2004) Stress-hyperglycemia, insulin and immunomodulation in sepsis. Intensive Care Med 30:748–756
Weekers F, Giulietti AP, Michalaki M, Coopmans W, Van Herck E, Mathieu C, Van den Berghe G (2003) Metabolic, endocrine, and immune effects of stress hyperglycemia in a rabbit model of prolonged critical illness. Endocrinology 144:5329–5338
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Bouillon R (2006) Intensive insulin therapy in the medical ICU. N Engl J Med 354:449–461
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R (2001) Intensive insulin therapy in the critically ill patients. N Engl J Med 345:1359–1367
Wiener RS, Wiener DC, Larson RJ (2008) Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA 300:933–944
Griesdale DE, de Souza RJ, van Dam RM, Heyland DK, Cook DJ, Malhotra A, Dhaliwal R, Henderson WR, Chittock DR, Finfer S, Talmor D (2009) Intensive insulin therapy and mortality among critically ill patients: a meta-analysis including NICE-SUGAR study data. CMAJ 180:821–827
Finfer S, Delaney A (2008) Tight glycemic control in critically ill adults. JAMA 300:963–965
Hermans G, Schetz M, van den Berghe G (2008) Tight glucose control in critically ill adults. JAMA 300:2725, author reply 2726–2727
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139
De La Rosa GD, Donado JH, Restrepo AH, Quintero AM, Gonzalez LG, Saldarriaga NE, Bedoya M, Toro JM, Velasquez JB, Valencia JC, Arango CM, Aleman PH, Vasquez EM, Chavarriaga JC, Yepes A, Pulido W, Cadavid CA (2008) Strict glycaemic control in patients hospitalised in a mixed medical and surgical intensive care unit: a randomised clinical trial. Crit Care 12:R120
Preiser JC, Devos P, Ruiz-Santana S, Melot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M, Stecher A, Chiolero R (2009) A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med 35:1738–1748
Plank J, Blaha J, Cordingley J, Wilinska ME, Chassin LJ, Morgan C, Squire S, Haluzik M, Kremen J, Svacina S, Toller W, Plasnik A, Ellmerer M, Hovorka R, Pieber TR (2006) Multicentric, randomized, controlled trial to evaluate blood glucose control by the model predictive control algorithm versus routine glucose management protocols in intensive care unit patients. Diabetes Care 29:271–276
Vogelzang M, Zijlstra F, Nijsten MW (2005) Design and implementation of GRIP: a computerized glucose control system at a surgical intensive care unit. BMC Med Inform Decis Mak 5:38
Eslami S, Abu-Hanna A, de Jonge E, de Keizer NF (2009) Tight glycemic control and computerized decision-support systems: a systematic review. Intensive Care Med 35:1505–1517
Chase JG, Shaw G, Le Compte A, Lonergan T, Willacy M, Wong XW, Lin J, Lotz T, Lee D, Hann C (2008) Implementation and evaluation of the SPRINT protocol for tight glycaemic control in critically ill patients: a clinical practice change. Crit Care 12:R49
Pachler C, Plank J, Weinhandl H, Chassin LJ, Wilinska ME, Kulnik R, Kaufmann P, Smolle KH, Pilger E, Pieber TR, Ellmerer M, Hovorka R (2008) Tight glycaemic control by an automated algorithm with time-variant sampling in medical ICU patients. Intensive Care Med 34:1224–1230
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 34:17–60
Furnary AP, Wu Y, Bookin SO (2004) Effect of hyperglycemia and continuous intravenous insulin infusions on outcomes of cardiac surgical procedures: the Portland Diabetic Project. Endocr Pract 10(Suppl 2):21–33
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM (2004) Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ (2009) Intensive versus conventional glucose control in critically ill patients. N Engl J Med 360:1283–1297
Egi M, Bellomo R, Stachowski E, French CJ, Hart G (2006) Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology 105:244–252
Krinsley JS (2008) Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med 36:3008–3013
Chase JG, Shaw GM (2007) Is there more to glycaemic control than meets the eye? Crit Care 11:160
Schultz MJ, Royakkers AA, Levi M, Moeniralam HS, Spronk PE (2006) Intensive insulin therapy in intensive care: an example of the struggle to implement evidence-based medicine. PLoS Med 3:e456
Lacherade JC, Jabre P, Bastuji-Garin S, Grimaldi D, Fangio P, Theron V, Outin H, De Jonghe B (2007) Failure to achieve glycemic control despite intensive insulin therapy in a medical ICU: incidence and influence on ICU mortality. Intensive Care Med 33:814–821
Carey RG (2002) How do you know that your chart is improving? Part I: basic concepts in statistical thinking. J Ambul Care Manage 25:80–87
Eslami S, de Keizer NF, Schultz MJ, de Jonge E, Abu-Hanna A (2008) A systematic review on quality indicators for tight glycaemic control in critically ill patients: need for an unambiguous indicator reference subset. Crit Care 12:R139
Mohammed MA, Worthington P, Woodall WH (2008) Plotting basic control charts: tutorial notes for healthcare practitioners. Qual Saf Health Care 17:137–145
Carey RG (2003) Improving healthcare with control chart: basic and advanced SPC methods and case studies. ASQ Quality Press, Milwaukee
Wheeler DJ (1995) Advanced topics in statistical process control. SPC Press, Knoxville
Vriesendorp TM, De Vries JH, van Santen S, Moeniralam HS, de Jonge E, Roos YB, Schultz MJ, Rosendaal FR, Hoekstra JB (2006) Evaluation of short-term consequences of hypoglycemia in an intensive care unit. Crit Care Med 34:2714–2718
Bagshaw SM, Bellomo R, Jacka MJ, Egi M, Hart GK, George C (2009) The impact of early hypoglycemia and blood glucose variability on outcome in critical illness. Crit Care 13:R91
Van den Berghe G (2006) First do no harm… hypoglycemia or hyperglycemia? Crit Care Med 34:2843–2844
Lonergan T, Le Compte A, Willacy M, Chase JG, Shaw GM, Wong XW, Lotz T, Lin J, Hann CE (2006) A simple insulin-nutrition protocol for tight glycemic control in critical illness: development and protocol comparison. Diabetes Technol Ther 8:191–206
Rood E, Bosman RJ, van der Spoel JI, Taylor P, Zandstra DF (2005) Use of a computerized guideline for glucose regulation in the intensive care unit improved both guideline adherence and glucose regulation. J Am Med Inform Assoc 12:172–180
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Eslami, S., Abu-Hanna, A., de Keizer, N.F. et al. Implementing glucose control in intensive care: a multicenter trial using statistical process control. Intensive Care Med 36, 1556–1565 (2010). https://doi.org/10.1007/s00134-010-1924-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1924-3