Abstract
Objective
To evaluate the impact of helium-oxygen (He/O2) on inspiratory effort and work of breathing (WOB) in intubated COPD patients ventilated with pressure support.
Design and setting
Prospective crossover interventional study in the medical ICU of a university hospital.
Patients and participants
Ten patients.
Interventions
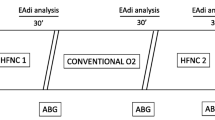
Sequential inhalation (30 min each) of three gas mixtures: (a) air/O2, (b) He/O2 (c) air/O2, at constant FIO2 and level of pressure support.
Measurements and results
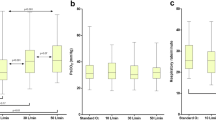
Inspiratory effort and WOB were determined by esophageal and gastric pressure. Throughout the study pressure support and FIO2 were 14±3 cmH2O and 0.33±0.07 respectively. Compared to Air/O2, He/O2 reduced the number of ineffective breaths (4±5 vs. 9±5 breaths/min), intrinsic PEEP (3.1±2 vs. 4.8±2 cmH2O), the magnitude of negative esophageal pressure swings (6.7±2 vs. 9.1±4.9 cmH2O), pressure-time product (42±37 vs. 67±65 cmH2O s−1 min−1), and total WOB (11±3 vs. 18±10 J/min). Elastic (6±1 vs. 10±6 J/min) and resistive (5±1 vs. 9±4 J/min) components of the WOB were decreased by He/O2.
Conclusions
In intubated COPD patients ventilated with pressure support He/O2 reduces intrinsic PEEP, the number of ineffective breaths, and the magnitude of inspiratory effort and WOB. He/O2 could prove useful in patients with high levels of PEEPi and WOB ventilated in pressure support, for example, during weaning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In decompensated chronic obstructive pulmonary disease (COPD) there is a marked increase in both the elastic and resistive components of the work of breathing (WOB) [1, 2, 3]. The ensuing respiratory muscle fatigue is a key factor determining weaning trial failure [4, 5], and prolonged ventilator dependence [1] in intubated patients. Pressure support (PS) is often used to provide a titrable level of respiratory muscle unloading in these patients [1]. However, excessive levels of PS can adversely affect patient-ventilator synchrony and increase WOB [6, 7]. Likewise, applying external positive end-expiratory pressure (PEEPe) can offset the inspiratory threshold effect of intrinsic PEEP (PEEPi) [8], but PEEPe may be difficult to titrate and can increase total PEEP and dynamic hyperinflation [9, 10]. On the other hand, helium-oxygen (He/O2) reduces the resistance to flow within the airways due to its low density [11]. In turn this effect has been shown to enhance lung emptying and decrease PEEPi [12] and to reduce WOB during controlled mechanical ventilation [13] and T-piece breathing [14] in intubated COPD. However, while two studies have shown that He/O2 can exert such beneficial effects in acutely decompensated COPD patients undergoing noninvasive PS [15, 16], no study has so far addressed whether these beneficial effects could also be observed in intubated patients. Such a favorable impact might indeed improve patient tolerance and endurance to spontaneous-assisted ventilation, for example, during weaning, while avoiding the deleterious effects of excessive respiratory muscle loading [17]. The purpose of the present study was therefore to test the hypothesis that He/O2 can reduce PEEPi and the magnitude of inspiratory effort and WOB during PS in intubated COPD patients.
Results from this study were presented in abstract form at the 2005 annual meeting of the American Thoracic Society [18].
Patients and methods
Patients
Patients were consecutively included if they met the commonly accepted criteria for COPD [19], were intubated, and in PS mode. Exclusion criteria were the presence of pneumothorax and/or hypoxemia requiring an inspired O2 fraction (FIO2) of 0.45 or higher. Ten patients were consecutively included in the study; patients’ main clinical characteristics are summarized in Table 1. Data collection was complete in all patients. As seen in their most recent FEV 1.0 values from the 2 years prior to admission, patients had severe obstructive disease. The protocol was accepted by the Ethics committee of our institution. Informed consent was obtained from all patients.
Methods
Prior to protocol initiation a nasogastric tube with esophageal and gastric balloons (Guenard ch 16 nasogastric tube, Marquat Génie Biomédical, Boissy-Saint-Léger, France) was inserted, and its correct position verified by the occlusion method [20]. The electromyographic activity of the diaphragm (EMGd) was recorded with two surface electrodes positioned on the right and left costal margins with a reference electrode placed over the sternum [21]. After filtering and digitalization at a sampling rate of 1000 Hz by means of the Biopac EMG module (Biopac Systems, Goleta, Calif., USA) the EMGd signal was rectified and integrated [22].
Patients were placed in a semirecumbent position, and the protocol was initiated after tracheal suctioning. All patients were ventilated with a Galileo Gold Series ventilator (Hamilton Medical, Rhäzuns, Switzerland), which can be safely used to deliver He/O2 without any modifications [23]. He/O2 was administered as previously described [12, 16]. Briefly, a 50-l canister pressurized at 200 bar (Carbagas, Gümligen, Switzerland) containing a 78:22 mixture of He and O2 was connected through a pressure regulator at 6 bar into the ventilator’s air inlet. A correction factor for reported tidal volume (VT) was used, since the VT reading on the ventilator underestimates the actual VT during He/O2 use [23]. The VT computed with this correction factor was also checked against true VT measured with a precision density-independent spirometer (5420 Volume Monitor, Ohmeda, Louisville, Col., USA). A heat and moisture exchanger was fitted on the ventilator circuit between the endotracheal tube and the Y-piece in all patients-PS was set by the clinician in charge of the patient, following our usual practice guidelines, i.e., FIO2 adjusted to maintain SpO2 at a level higher than 0.9, level of PS titrated to obtain an expired VT of 8 ml/kg, pressurization time of 0.2 s, inspiratory trigger set at maximum sensitivity, and inspiratory:expiratory cycling set at 25% of peak inspiratory flow rate. PEEPa to compensate for the inspiratory threshold load of PEEPi was added following our usual protocol, i.e., starting at zero end-expiratory pressure and increasing by 1 cmH2O increments until ineffective inspiratory attempts disappeared or decreased [8] to a maximum of 10 cmH2O.
After an initial 30 min period with Air/O2 patients were switched to the He/O2 mixture for 30 min, then back again for 30 min to Air/O2. All ventilator settings including FIO2 were kept constant throughout the protocol. Heart rate, arterial blood pressure, and pulse oxymetry were continuously monitored.
Measurement protocol
Data recordings were performed during the last 5 min of ventilation with each gas mixture. Esophageal (Pes) and gastric pressures (Pga) were continuously recorded by differential pressure transducers (Biopac), all signals being digitalized at a sampling rate of 1000 Hz, and stored in a laptop computer for subsequent analysis (AcqKnowledge software, Biopac). Patient inspiratory effort time (ti) was measured as the interval between the initial decrease in Pes and the initial rapid decrease of electrical activity on the processed EMGd signal [22, 24].
The following parameters were determined during each phase of the protocol: VT, minute-volume (V′E), and peak expiratory flow (V′exp) obtained by analysis of the instantaneous flow tracing; peak expiratory resistance (Rexp) computed as Rexp=Paw−Pes/V′exp, where Paw=airway pressure; the expiratory time constant (τe), determined by analysis of the expiratory flow-volume tracing [25]; respiratory rate reported by the ventilator (RRvent); patient respiratory rate (RRpat) determined from EMGd and Pes tracings; number of ineffective inspiratory attempts (Rineff), computed as Rineff=RRpat−RRvent; PEEPi: the Pes difference between the onset of inspiratory effort and the point at which instantaneous expiratory flow reached 0, further corrected for any expiratory muscle activity [26]; trigger delay (Td): the time difference between the onset of inspiratory effort and that of pressurization by the ventilator; duration of delayed cycling (tiexcess), computed as the difference between the end of ti and the duration of pressurization by the ventilator. Respiratory muscle workload can be determined by two approaches. One is to compute it from the esophageal pressure and flow tracings. Its drawback is that it is dependent on flow, and therefore does not take into account the ineffective inspiratory efforts which are often present in COPD. Hence this technique underestimates the magnitude of inspiratory muscle workload. However, its main advantage is that it allows determination of total transpulmonary WOB and its partition into elastic and resistive components, which is important to assess the various effects of helium in obstructive patients. The other approach is to compute the pressure-time product, which does not depend on flow, and therefore takes into account the workload imposed by ineffective inspiratory attempts. This technique is also well correlated with respiratory muscle oxygen consumption and therefore with the metabolic cost of breathing. We therefore used both methods in the present study. Inspiratory WOB was determined by analysis of the Pes−VT tracing, using the classical method based on the Campbell diagram [15, 27]: briefly, WOB was determined as the area enclosed between (a) the inspiratory Pes−VT curve and (b) the static esophageal chest wall pressure-volume curve, using a theoretical chest wall compliance value (4% of the predicted value of the vital capacity/cmH2O). WOB was expressed as work per breath (J/cycle) and per volume unit (J/l).
Using measurements of transpulmonary pressure (i.e., the difference between airway pressure, Paw, measured at the endotracheal tube, and Pes), total transpulmonary work per minute (Wtptot, J/min) was determined, and partitioned into its resistive (Wtpres, J/min) and elastic (Wtpel, J/min) components [15]. Finally, due to the presence of ineffective inspiratory attempts inspiratory effort was also quantified by computation of transdiaphragmatic pressure (Pdi), as well as total (PTPdi) and triggering (PTPt) pressure-time products, which are independent of flow and volume signals [28]. WOB was thus computed only for those patient breaths which triggered the ventilator, as was the PTPt, while Pdi and PTPdi were determined for both triggering and nontriggering breaths. Arterial blood gases were analyzed at the end of each study phase. Figure 1 illustrates the various time intervals from a patient.
Representative tracing from a patient, illustrating the various time intervals used. Paw Airway pressure; Flow instantaneous flow measured at airway opening; Pdi transdiaphragmatic pressure; EMGd electromyographic recording of the diaphragm; td trigger delay; ti patient inspiratory effort duration; ti assist duration of pressurization by the ventilator; ti excess duration of pressurization by the ventilator extending beyond the end of ti
Statistics
Data are expressed as mean ±standard deviation. Comparisons (SigmaStat 2.0, SPSS Science) between the three conditions was made by analysis of variance, significance between the time points being determined by Fisher’s protected least significance test. A p value less than 0.05 was considered significant.
Results
No significant differences were observed between the Air/O2 1 and Air/O2 2 data sets. The patients’ respiratory pattern for each condition are shown in Table 2. Expiratory resistance, expiratory time constant, and peak expiratory flow all decreased with He/O2. PEEPi was present in all patients, and its magnitude was decreased by He/O2 as well as the number of ineffective inspiratory attempts. Delayed cycling (tiexcess) was present in all patients but was not influenced by He/O2. Table 3 summarizes the main findings with respect to inspiratory effort and WOB. The magnitude of inspiratory effort, characterized by the Pes and Pdi variations, was decreased by He/O2, as was the PTP. The individual variations or Pdi swings are shown in Fig. 2. The total WOB determined from the Pes tracing was reduced during He/O2 inhalation. Finally, WOB computed from the transpulmonary pressure measurements was also decreased by He/O2, in both its elastic and its resistive components. As shown in Table 4, He/O2 had no effect on arterial blood gases or hemodynamics.
Discussion
The findings of the present study demonstrate that in intubated patients with severe COPD ventilated in PS He/O2 decreases the level of PEEPi and the number of ineffective inspiratory attempts and also reduces the magnitude of inspiratory efforts and the total WOB as well as its resistive and elastic components. Let us now attempt to put these results in perspective and assess how they may affect the weaning process in COPD patients.
Several limitations of the study should be noted initially. First, only a small number of patients was studied. However, all patients exhibited the same response pattern when switched from one gas mixture to another. Second, the static esophageal chest wall pressure-volume curve was determined using a theoretical chest wall compliance rather than a measured value. Nonetheless, although some degree of error can occur with this approach, comparisons between those conditions remains valid, given that the error is present in all measurement conditions [27]. Third, He/O2 was administered for 30 min, which might be insufficient for its full effects to occur in very inhomogeneous lungs such as those of COPD. However, this duration is in line with that of other studies in which a highly significant effect of He/O2 was documented after 20–45 min [10, 12, 13, 14, 15, 16]. Fourth, during spontaneous-assisted breathing reliable measurements of static respiratory system compliance are not possible, leading to some difficulties in interpreting changes in the elastic component of the WOB (Wtpel) [13].
Overall our findings are in line with those of recent studies on He/O2 in intubated COPD patients. During controlled ventilation a decrease in dynamic hyperinflation and PEEPi with He/O2 has been shown [10, 12]. The level of PEEPi was lower in the present study, which is to be expected as patients were in the weaning phase, whereas those of the two former studies had been intubated for less than 48 h. However, the magnitude of decrease in PEEPi was comparable between these three studies. Recently Gainnier et al. [13] obtained similar results in patients undergoing controlled ventilation and also documented a reduction in total, resistive, and elastic WOB with He/O2. The magnitude of decrease in total and individual determinants of WOB was greater in our patients, although the ventilatory mode and timing with regards to intubation were different. This discrepancy probably results from the different measurement techniques used as well as from the fact that their patients were in controlled conditions while those of the present study were undergoing PSV.
In spontaneously breathing COPD patients immediately before extubation without any ventilatory assistance Diehl et al. [14] also observed that He/O2 reduced the level of PEEPi and the WOB, mainly of its resistive component. PEEPi was lower than that in our patients, which is to be expected given that the Diehl et al. study was performed immediately before extubation. Likewise, and probably for the same reasons, the reduction in WOB was smaller in the patients studied by Diehl et al. Finally, during noninvasive PSV applied by face mask to acutely decompensated patients He/O2 leads to a reduction in WOB [15], PaCO2, and dyspnea [15, 16]. Jaber et al. [15] found that PSV at levels comparable to that in our patients decreased the intensity of inspiratory efforts and WOB. The magnitude of these changes was close to that observed in our patients, although PSV was applied noninvasively and to acutely decompensated patients.
The effects of He/O2 on the patients’ ventilatory pattern should be briefly discussed. First, one might have expected the triggering delay to decrease while breathing He/O2, as PEEPi, which represents an inspiratory threshold load, was reduced. The fact that only a nonsignificant trend towards a lower delay was documented probably stems from the low initial level of PEEPi in our patients. Delayed cycling was unaffected by He/O2. This is not surprising given that delayed cycling is influenced by several factors such as the cycling cutoff level of the ventilator (25% of peak inspiratory flow in this study), the time constant of the respiratory system (RC), duration and magnitude of inspiratory effort, level of PS, and profile of the pressure-time curve [22, 29]. Quantitatively the most important determinant of delayed cycling is the ratio between RC and inspiratory time [22, 29]. While elastance and resistance were not measured, the decrease in elastic and resistive components of the WOB suggests that both determinants of the RC were reduced, and therefore that RC remained unchanged. Inspiratory time was also unchanged. Therefore no modification in the magnitude of delayed cycling was observed, as one would expect.
Of note, no effect of He/O2 on PaCO2 was observed. However, the key factor determining the impact of heliox on PaCO2 is probably its initial level. In a previous study in patients undergoing noninvasive PS we found that PaCO2 was lowered the most in those patients who had the highest initial levels of hypercapnia [16], a finding which has subsequently been confirmed by Jaber et al. [15]. In the present study the patients were not acutely decompensated or severely hypercapnic but represented a heterogeneous group of patients who had been intubated, ventilated in controlled mode, and at various stages of the weaning process in PS. Therefore some patients were nonhypercapnic while others had no elevation or only moderate increases in PaCO2. Illustrating this point, we found no effect on PaCO2 in patients without marked hypercapnia in two studies in intubated patients undergoing controlled ventilation [10, 12].
Our results confirm that He/O2, by reducing expiratory airways resistance, can increase expiratory flow, thereby leading to enhanced lung emptying and a decrease in PEEPi. This in turn leads to several beneficial effects. First, the decreased inspiratory threshold load induces a reduction in the number of nontriggering breaths and most likely accounts for the decrease in the magnitudes of esophageal pressure swings and PTP. Second, through the reduction in PEEPi and airways resistance there is a decrease in both elastic and resistive WOB. These results add to the body of evidence outlining the favorable pathophysiological effects of He/O2 in COPD and suggests that it may be useful in difficult-to-wean patients. However, to date there is no proof that these effects can actually impact patient outcome [30]. Furthermore, He/O2 can interfere with ventilator function, thus requiring thorough knowledge of these technical aspects by intensivists to ensure patient safety [23]. Finally, cost can be an issue, although probably not a major one [30].
In conclusion, the present study demonstrates that in intubated COPD patients ventilated with PS He/O2 enhances lung emptying, decreases PEEPi and the number of ineffective inspiratory attempts, and reduces the various key determinants of elevated WOB and inspiratory effort. He/O2 may therefore prove useful in patients with high levels of PEEPi and WOB by unloading the respiratory muscles. This can improve patient-ventilator interaction and tolerance to spontaneous-assisted breathing, which in turn may be beneficial for patient outcome, for example, by facilitating weaning. However, the optimal timing and duration of He/O2 administration remains to be determined. Furthermore, given the technical pitfalls and cost issues associated with the use of He/O2, studies are needed to determine whether the beneficial pathophysiologocal effects of He/O2 inhalation during weaning can have an impact on the duration of weaning, ICU stay, and overall patient outcome.
References
Appendini L, Purro A, Patessio A, Zanaboni S, Carone M, Spada E, Donner C, Rossi A (1996) Partitioning of inspiratory muscle workload and pressure assistance in ventilator-dependent COPD patients. Am J Respir Crit Care Med 154:1301–1309
Jounieaux V, Mayeux I (1995) Oxygen cost of breathing in patients with emphysema or chronic bronchitis in acute respiratory failure. Am J Respir Crit Care Med 152:2181–2184
Fleury B, Murciano D, Talamo C, Aubier M, Pariente R, Milic-Emili J (1985) Work of breathing in patients with chronic obstructive pulmonary disease in acute respiratory failure. Am Rev Respir Dis 131:822–827
Zakynthinos S, Vassilakopoulos T, Roussos C (1995) The load of inspiratory muscles in patients needing mechanical ventilation. Am J Respir Crit Care Med 152:1248–1255
Roussos C, Zakynthinos S (1996) Fatigue of the respiratory muscles. Intensive Care Med 22:134–155
Leung P, Jubran A, Tobin M (1997) Comparison of assisted ventilator modes on triggering, patient effort, and dyspnea. Am J Respir Crit Care Med 155:1940–1948
Parthasarathy S, Jubran A, Tobin M (1998) Cycling of inspiratory and expiratory muscle groups with the ventilator in airflow limitation. Am J Respir Crit Care Med 158:1471–1478
Nava S, Bruschi C, Rubini F, Palo A, Iotti G, Braschi A (1995) Respiratory response and inspiratory effort during pressure support ventilation in COPD patients. Intensive Care Med 21:871–879
Ranieri V, Giuliani R, Cinnella G, Pesce C, Brienza N, Ippolito E, Pomo V, Fiore T, Gottfried S, Brienza A (1993) Physiologic effects of positive end-expiratory pressure in patients with chronic obstructive pulmonary disease during acute ventilatory failure and controlled mechanical ventilation. Am Rev Respir Dis 147:5–13
Jolliet P, Watremez C, Roeseler J, Ngengiyumva JC, De Kock M, Clerbaux T, Tassaux D, Reynaert M, Detry B, Liistro G (2003) Comparative effects of helium-oxygen and external positive end-expiratory pressure on respiratory mechanics, gas exchange, and ventilation-perfusion relationships in mechanically ventilated patients with chronic obstructive pulmonary disease. Intensive Care Med 29:1442–1450
Papamoschou D (1995) Theoretical validation of the respiratory benefits of helium-oxygen mixtures. Respir Physiol 99:183–199
Tassaux D, Jolliet P, Roeseler J, Chevrolet J (2000) Effects of helium-oxygen on intrinsic positive end-expiratory pressure in intubated and mechanically ventilated patients with severe chronic obstructive pulmonary disease. Crit Care Med 28:2721–2728
Gainnier M, Arnal J, Gerbeaux P, Donati S, Papazian L, Sainty J (2003) Helium-oxygen reduces the work of breathing in mechanically ventilated patients with chronic obstructive pulmonary disease. Intensive Care Med 29:1666–1670
Diehl JL, Mercat A, Guérot E, Aïssa F, Teboul JL, Richard C, Labrousse J (2003) Helium/oxygen mixture reduces the work of breathing at the end of the weaning process in patients with severe chronic obstructive pulmonary disease. Crit Care Med 31:1415–1420
Jaber S, Fodil R, Carlucci A, Boussarsar M, Pigeot J, Lemaire F, Harf A, Lofaso F, Isabey D, Brochard L (2000) Noninvasive ventilation with helium-oxygen in acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 161:1191–1200
Jolliet P, Tassaux D, Thouret J, Chevrolet J (1999) Beneficial effects of helium-oxygen vs. air-oxygen non-invasive pressure support in decompensated COPD patients. Crit Care Med 27:2422–2429
Orozco-Levi M, Lloreta J, Minguella J, Serrano S, Broquetas J, Gea J (2001) Injury of the human diaphragm associated with exertion and chronic obstructive pulmonary disease. Am J Respir Crit Car Med 164:1734–1739
Tassaux D, Gainnier M, Battisti A, Jolliet P (2005) Effect of heliox on inspiratory effort and work of breathing in intubated COPD patients during weaning with pressure support. Am J Respir Crit Care Med 2:A160
Derenne J, Fleury B, Pariente R (1988) Acute respiratory failure of chronic obstructive pulmonary disease. Am Rev Respir Dis 138:1006–1033
Baydur A, Behrakis P, Zin W, Jaeger M, Milic-Emili G (1982) A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis 788–791
Maarsingh E, Van Eykern L, Sprikkelman A, Hoekstra M, Aalderen W (2000) Respiratory muscle activity measured with a noninvasive EMG technique: technical aspects and reproductibility. J Appl Physiol 88:1955–1961
Tassaux D, Michotte J, Gainnier M, Gratadour P, Fonseca S, Jolliet P (2004) Expiratory trigger setting in pressure support ventilation: from mathematical model to bedside. Crit Care Med 32:1844–1850
Tassaux D, Jolliet P, Thouret J, Roeseler J, Dorne R, Chevrolet J (1999) Calibration of seven ICU ventilators for mechanical ventilaton with helium-oxygen mixtures. Am J Respir Crit Care Med 160:22–32
Parthasarathy S, Jubran A, Tobin M (2000) Assessment of neural inspiratory time in ventilator-supported patients. Am J Respir Crit Care Med 162:546–552
Lourens M, van den Berg B, Aerts J, Verbraak A, Hoogsteden H, Bogaard J (2000) Expiratory time constants in mechanically ventilated patients with and without COPD. Intensive Care Med 26:1612–1618
Lessard M, Lofaso F, Brochard L (1995) Expiratory muscle activity increases intrinsic positive end-expiratory pressure independently of dynamic hyperinflation in mechanically ventilated patients. Am J Respir Crit Care Med 151:562–569
Brochard L, Rua F, Lorino H, Lemaire F, Harf A (1991) Inspiratory pressure support compensates for the additional work of breathing caused by the endotracheal tube. Anesthesiology 75:739–745
Sassoon C, Light R, Lodia R, Sieck G, Mahutte C (1991) Pressure-time product during continuous positive airway pressure, pressure support ventilation and T-piece weaning from mechanical ventilation. Am Rev Respir Dis 143:459–475
Yamada Y, Du H (2000) Analysis of the mechanisms of expiratory asynchrony in pressure support ventilation: a mathematical approach. J Appl Physiol 88:2143–2150
Jolliet P, Tassaux D, Roeseler J, Burdet L, Broccard A, D’Hoore W, Borst F, Raeynaert M, Schaller M, Chevrolet J (2003) Helium-oxygen vs. air-oxygen non-invasive pressure support in decompensated chronic obstructive disease: a prospective multicenter study. Crit Care Med 31:878–884
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding was provided by the Swiss National Scientific Research Fund (grant #32-63501.00)
Rights and permissions
About this article
Cite this article
Tassaux, D., Gainnier, M., Battisti, A. et al. Helium-oxygen decreases inspiratory effort and work of breathing during pressure support in intubated patients with chronic obstructive pulmonary disease. Intensive Care Med 31, 1501–1507 (2005). https://doi.org/10.1007/s00134-005-2796-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2796-9