Abstract
Objective
To investigate whether pyrrolidinone derivative (N2733), an inhibitor of nuclear factor (NF)-κB activation, improves altered metabolic and hemodynamic changes and organ dysfunctions caused by endotoxic shock.
Design and setting
Prospective, randomized, animal study in a laboratory at a university hospital.
Subjects
Twenty-three anesthetized male beagle dogs (10–14 kg).
Interventions
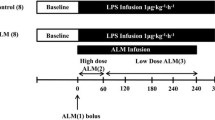
Dogs were mechanically ventilated and monitored with a pulmonary arterial catheter and a gastric tonometer. A central venous catheter was inserted into the femoral vein, and lactated Ringer’s solution (10 ml/kg per hour) was administered throughout the study period. Three groups of animals were studied: (a) the lipopolysaccharide (LPS) group (n=8), which received LPS (250 ng/kg per minute for 2 h); (b) the LPS plus N2733 group (n=8), which received N2733 (30 mg/kg intravenously and 10 mg/kg hour for 6 h) after the start of LPS; and (c) the N2733 group (n=7), which received N2733 (30 mg/kg intravenously and 10 mg/kg per hour for 6 h).
Measurements and results
Changes in hemodynamics, blood gas, gastric intramural pH, and renal and hepatic function were measured for 6 h. Coadministration of N2733 increased oxygen delivery index and prevented the LPS-induced hypotension, metabolic acidosis, and gastric mucosal acidosis but did not affect renal or hepatic function.
Conclusions
Administration of N2733 increased oxygen delivery index and prevented the LPS-induced hypotension and metabolic and gastric mucosal acidosis in an anesthetized canine endotoxic shock model, suggesting its beneficial effect on local blood flow against tissue hypoxia. These findings suggest that blockade of NF-κB activation prevents hypodynamic shock and gastric hypoperfusin in endotoxic shock.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial endotoxin triggers release of a variety of mediators through the activation of proinflammatory cytokines which can amplify the inflammatory response to induce tissue damage [1, 2]. At the cellular level endotoxin causes immediate expression of genes encoding various immunomediators by the activation of the transcription factor, nuclear factor (NF)-κB [3]. NF-κB plays an important role in transcriptional regulation of many proinflammatory genes, such as tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, and inducible nitric oxide synthase (iNOS) [4]; NF-κB is considered to be involved in the pathogenesis of systemic inflammatory response syndrome and multiple-organ dysfunction syndrome as a pivotal determinant. It has been reported that mortality in patients with sepsis is predictable by increased NF-κB activity of the patient’s blood mononuclear cells; nonsurvivors had more than twofold increase over controls in NF-κB activation in the first 6 days, whereas survivors had less than that during 14 days [5].
Although both anti-TNF antibody and IL-1 receptor antagonist have been shown to be effective in experimental endotoxic animal models, none has been shown to be successful in clinical studies [6, 7]. Thus blockade of a single mediator may be insufficient to prevent diverse inflammatory response pathways because a variety of inflammatory mediators other than TNF-α and IL-1 have already been activated by NF-κB. Therefore any modalities that selectively block NF-κB activity in the proximal pathway could be more efficient and effective than those in distal pathway for the treatment of endotoxic shock [8].
A pyrrolidinone derivative, N2733, has been shown to block NF-κB activation by preventing phosphorylation and degradation of IκB-α [9] and inhibit the LPS-induced TNF-α production in vitro with an improvement in the survival rate of endotoxemic mice in vivo [10]. However, it remains unknown whether this compound has any beneficial effects on endotoxic shock animal models other than rodents. It is mandatory to obtain the detailed experimental data in larger animal models of endotoxic shock before its clinical trials. We therefore attempted to determine whether this pyrrolidinone derivative compound prevents multiple organ dysfunction in canine endotoxic shock model.
Materials and methods
Experimental protocol
The study was approved by the Institutional Review Board for the care of animal subjects. The care and handling of the animals were in accord with National Institutes of Health guidelines. Twenty-three male beagle dogs (10–14 kg) were used in this experiment. After intramuscular injection of ketamine (15 mg/kg) the dogs were placed in supine position, anesthetized with pentobarbital sodium (30 mg/kg intravenously), and maintained with supplemental doses (4 mg/kg per hour) throughout the experiment. The dogs were intubated and ventilated (EV-A ventilator, Dräger, Lübeck, Germany) at an FIO2 of 0.3, tidal volume of 12–15 ml/kg, and respiratory rate of 15 cycles/min. Arterial blood gases and pH were measured before the start of the experiment, and tidal volume was adjusted to maintain arterial carbon dioxide tension and pH within the physiological range. After initial ventilator setting tidal volume was not changed throughout the study period.
A central venous catheter was inserted via the femoral vein and advanced into the central venous circulation, and central venous pressure (CVP) was measured via the distal port of this catheter. Lactated Ringer’s solution (10 ml/kg per hour) was administered by this central venous catheter throughout the study period. Muscle paralysis was obtained by the administration of pancuronium bromide with initial dose of 0.16 mg/kg and subsequent doses of 0.08 mg/kg per hour. The right external jugular vein was exposed, and a flow-directed, balloon-tipped thermodilution catheter (93A-141-7F, Baxter Edwards Critical Care, Irvine, Calif., USA) was inserted into the pulmonary artery. The femoral artery was cannulated with catheter for continuous measurements of systemic arterial pressure and heart rate and for intermittent arterial blood sampling. All catheters were connected to transducers, and zero calibration was taken at the midchest level. All pressures were measured on a polygraph system (RM-7000, Nihon Kohden, Tokyo, Japan) connected to the pressure lines through transducers. A urinary catheter was inserted into bladder for timed urine collections. After surgical preparation the dogs were allowed to stabilize for 1 h.
Dogs were randomized to be divided into three experimental groups: the lipopolysacharide (LPS) group (n=8), the LPS plus pyrrolidinone derivative (N2733) group (n=8), and the N2733 group (n=7). In the LPS group bacterial LPS (Escherichia coli endotoxin, 0127;B8, Difco, Detroit, Mich., USA) was infused intravenously at a rate of 250 ng/kg per minute for 2 h as previously described [11]. In the LPS plus N2733 group N2733 (30 mg/kg) was injected intravenously as a bolus immediately after the start of LPS infusion and was infused intravenously (followed by) at a rate of 10 mg/kg per hour for 6 h. In the N2733 group N2733 (30 mg/kg) was injected intravenously as a bolus and was infused intravenously at a rate of 10 mg/kg per hour for 6 h. Doses of N2733 were chosen on the basis of pilot experiments and our previously published data in rodent model [9, 10].
Heart rate, mean arterial pressure (MAP), mean pulmonary arterial pressure, pulmonary artery occlusion pressure, central venous pressure, and arterial and mixed venous blood gases were measured at 1-h intervals for 6 h. Cardiac output was measured by injecting 5 ml iced 5% dextrose solution via the distal port of the central venous catheter using the thermodilution technique with a cardiac computer (9520A, Baxter Edwards); the mean value of three measurements and cardiac index was calculated; body surface area (m2) was calculated by the formula: body weight (kg)2/3×0.11. Systemic vascular resistance index and pulmonary vascular resistance index were calculated using standard formulae. Arterial and mixed venous blood samples were obtained simultaneously from femoral and pulmonary artery, respectively. Blood gases and O2 saturation were measured by pH/blood gas analyzer (IL 1306A, Instrumentation Laboratory, Lexington, Mass., USA). Hemoglobin (Hb) concentration was measured by Celltak α (MEK-6108, Nihon Kohden). Oxygen delivery index and oxygen consumption index were calculated by following formulae. Oxygen delivery index=CaO2×CI×10; oxygen consumption index=(CaO2−CvO2)×CI×10, where CaO2 is arterial oxygen content, CvO2 is mixed venous oxygen content, and CI is cardiac index. CaO2=1.39×Hb×SaO2+0.0031×PaO2; CvO2=1.39×Hb×SvO2+0.0031×PvO2, where SaO2 is oxygen saturation of arterial blood and SvO2 is oxygen saturation of mixed venous blood.
Gastric intramural pH (pHi) was measured by tonometer (TRIP NGS catheter, Tonometrics, Helsinki, Finland) at 1 h intervals for 6 h. Saline (2.5 ml) was instilled into the tonometer balloon and left in place for 1 h. The saline was then removed and analyzed for PCO2 (gastric mocosal PCO2) after discarding the first 1 ml. Gastric mucosal PCO2 was corrected for the equilibration period and was used with arterial bicarbonate to calculate the pHi as a parameter indicative of gastric mucosal perfusion rate [12]. Additional arterial blood samples were obtained at baseline and 6 h for measurements of aspartate and alanine aminotransferase, bilirubin, and creatinine by an automatic analyzer (7170, Hitachi, Tokyo, Japan). Urine volume was measured at baseline and 6 h.
Data are expressed as mean ±SD. Parameters were compared over the time course using an analysis of variance for repeated measures. When appropriate, post hoc comparisons were made with Bonferroni’s adjustment for the effect of time in a specific group with values at 0 h as a control, and for the effects of treatment at specific times. All analyses were performed using StatView (Abacus Concepts, Berkeley, Calif., USA). Differences at the level of p<0.05 were considered statistically significant.
Results
Changes in hemodynamics
LPS infusion caused a significant (p<0.05) fall in MAP for 2–3 hs which was significantly blocked by coadministration of N2733; N2733 alone had no effect (Fig. 1). CI tended to decrease, but other hemodynamics did not significantly change during 6 h after LPS infusion. Furthermore, LPS infusion tended to decrease oxygen delivery index during 2–6 h, which was significantly blocked by coadministration of N2733. Other hemodynamic parameters did not differ significantly between the three groups (data not shown).
Changes in mean arterial pressure (MAP) and oxygen delivery index. After administration of bacterial lipopolysaccharide (LPS; 250 ng/kg per minute for 2 h) without or with N2733 (30 mg/kg intravenously, 10 mg/kg per hour for 6 h) in anesthetized dogs MAP (upper panel) and oxygen delivery index (lower panel) were measured. *p<0.05, **p<0.01 vs. 0 h, ‡p<0.01 vs. the LPS group
Changes in blood gas and gastric pHi parameters
LPS induced a significant (p<0.05) metabolic acidosis which was reversed by coadministration of N2733; N2733 alone did not affect pH or base excess (Fig. 2). PaCO2 did not significantly change in any group. There were no significant differences in PaO2 or PaCO2 between the three groups (data not shown). LPS also induced a significant (p<0.01) decrease in gastric pHi for 2–6 h which was similarly prevented by co-administration of N2733; N2733 alone had no effect.
Changes in arterial pH, arterial base excess, and gastric intramural pH (pHi). After administration of bacterial lipopolysaccharide (LPS; 250 ng/kg per minute for 2 h) without or with N2733 (30 mg/kg intravenously, 10 mg/kg per hour for 6 h) in anesthetized dogs, arterial pH (top panel), base excess (middle panel), and gastric pHi (bottom panel) were measured. *p<0.05, **p<0.01 vs. 0 h, †p<0.05, ‡p<0.01 vs. the LPS group
Changes in renal and liver function
Urine volume did not significantly change after LPS infusion, whereas urine volume was markedly increased by administration of N2733 (Table 1). Serum concentration of creatinine did not significantly change in any group. Although LPS tended to increase serum concentrations of aspartate aminotransferase, alanine aminotransferase, and bilirubin, there were no significant differences in hepatic enzymes and bilirubin between the three groups.
Discussion
The present study clearly shows that administration of N2733, an inhibitor of NF-κB activation, prevents hypotension and metabolic and gastric mucosal acidosis in an anesthetized canine endotoxic shock model. Furthermore, the present study revealed that administration of N2733 increased oxygen delivery index in the canine endotoxic shock model, suggesting its beneficial effect on local blood flow against tissue hypoxia.
In sepsis NF-κB plays a central role in regulating the gene transcription of several inflammatory cytokines and mediators. Excessive activation of NF-κB by endotoxin and cytokines could lead to the uncontrolled and persistent activation of the same genes of the inflammatory cytokines and mediators via positive or forward feed-back mechanism [4, 5, 8]. Thus the blockage of initial activation of NF-κB pathway could prevent the development of the critical illness caused by sepsis [13]. The administration of N2733 immediately after LPS infusion may therefore have reduced inflammatory response in the early stages. Cuzzocrea et al. [14] have also shown that the antioxidant pyrrolidine dithiocarbamate, a potent inhibitor of NF-κB activation, attenuates the degree of zymosan-induced multiple-organ failure in mice.
Endotoxic shock is characterized by hypotension and depressed myocardial function along with perfusion abnormalities, including metabolic acidosis and oliguria. These pathophysiological changes are due to excess production of proinflammatory cytokines, such as TNF-α and IL-1 [1], and reactive free radicals, including superoxide anion and NO [15], among which TNF-α is related to mortality during multiple-organ dysfunction [16]. N2733 has been shown to inhibit TNF-α production in vitro and improve survival rate in endotoxemic mice [10], suggesting its therapeutic potential for prevention of multiple organ dysfunction. However, the exact mechanism by which N2733 attenuates multiple organ dysfunction in endotoxic shock remains unknown.
Excess production of NO by iNOS in endotoxic shock has been shown to play a major role in endotoxin-induced hypotension [17]. We have previously shown that a selective inhibitor for iNOS improves hypotension and lactic acidosis in canine endotoxic shock model [18]. The generation of large quantities of NO may cause maldistribution of regional blood flow and formation of a diffusion barrier for oxygen and inhibition of mitochondrial respiration [19]. Although NO induces vasodilatation in some organs, not all organ perfusion may improve. In concert with hypotension, these effects of NO may contribute to the tissue ischemia which ultimately facilitates the development of multiple organ dysfunction syndrome. It has been shown that activation of the transcription factor NF-κB plays a pivotal role in the expression of iNOS by TNF-α and IL-1 [20], and we have further demonstrated that N2733 inhibits cytokine-induced NF-κB activation and iNOS expression in vitro [9]. Therefore it is reasonable to consider that inhibition of iNOS-derived NO production by N2733 may partly block the LPS-induced hypotension and metabolic acidosis as demonstrated in this study. Since the inhibition of NO formation by N2733 is limited to iNOS-induced NO, systemic vasoconstriction may not be profound in the presence of endothelial NO synthase derived NO.
Measurement of gastric pHi by the tonometric method has been used as an indicator of the adequacy of perfusion, oxygen delivery, and oxygen utilization in the stomach [12]. A gastric pHi value less than 7.35 has been shown to be prognostic for increased mortality in patients with acute circulatory failure [21]. In the present study the LPS-induced decrease in gastric pHi in canine endotoxic shock model was blocked by administration of N2733, suggesting its beneficial effect on the maintenance of gastric mucosal perfusion.
The mechanisms of the LPS-induced metabolic acidosis may be explained by several possible causes. First, failure of adequate oxygen delivery to individual tissues could cause tissue hypoperfusion and ischemia, resulting in production of lactate in the presence of anaerobic metabolism. Our previous study [18] has shown that same doses of LPS infusion induced lactic acidosis. Second, failure of cellular oxygen utilization in certain local regions may result in lactic acidosis without significant decrease in global oxygen consumption in this model. Third, loss of large volumes of gastrointestinal tract secretions containing substantial amount of bicarbonate could cause metabolic acidosis.
The present study shows that administration of N2733 increases urine volume, and that serum creatinine level was lower in the N2733 group than the LPS group. In the N2733 group urine output was greater than the infusion rate (10 ml/kg per hour) of lactated Ringer’s solution, resulting in mild decrease in MAP. It has been shown that hypotension during endotoxemia is associated with a renal hypoperfusion in dogs [22]. Since LPS-induced fall in MAP was blocked by N2733, N2733 may have increased renal blood flow, resulting in increased urine volume. A fivefold increase in urine output in the N2733 group may be due to its diuretic effects, although its exact mechanism remains unknown from the present experiment. Administration of N2733 did not significantly affect on liver function, although there was a greater variation in hepatic injury to LPS challenge among animals. Thus it remains to be determined using a larger number of animals whether N2733 actually prevents the LPS-induced hepatic dysfunction.
Our endotoxic model is hypodynamic one. The LPS-induced hypotension in our study was accompanied by a tendency towards decreased CI at least during 6 h, which could lead to gradual decrease in cardiac output after longer observation periods. As a result, the calculated systemic vascular resistance index would not decrease. This phenomenon may be explained by the method of fluid resuscitation chosen for this study. The fluid resuscitation by lactated Ringer’s solution (10 ml/kg per hour) administered during the study period might be insufficient to produce hyperdynamic model as usually observed during human septic shock.
Since the experiment was designed for short-term (6 h) canine endotoxic shock model, it remains unknown whether N2733 may improve LPS-induced hemodynamic changes, metabolic acidosis, renal and hepatic functions, and survival rate after a longer periods. Thus long-term effect of N2733 in canine endotoxic shock model is another important subject for future research.
Conclusions
Administration of N2733 increased oxygen delivery index and prevented LPS-induced hypotension and metabolic and gastric mucosal acidosis in an anesthetized canine endotoxic shock model. These findings suggest that blockade of NF-κB activation prevents hypodynamic shock and gastric hypoperfusion in endotoxic shock.
References
Parrillo JE (1993) Pathogenetic mechanism of septic shock. N Engl J Med 328:1471–1477
Natanson C, Hoffman WD, Suffredini AF, Eichacker PQ, Danner RL (1994) Selected treatment strategies for septic shock based on proposed mechanisms of pathogenesis. Ann Intern Med 120:771–783
Baeuerle PA, Henkel T (1994) Function and activation of NF-κB in the immune system. Annu Rev Immunol 12:141–179
Barnes PJ, Karin M (1997) Nuclear factor κB-A pivotal transcription factor in chronic inflammatory diseases. N Engl J Med 336:1066–1071
Böhrer H, Qiu F, Zimmermann T, Zhang Y, Ilmer T, Mannel D, Bottiger BW, Stern DM, Walderr R, Saeger HD, Zeigler R, Bierhaus A, Martin E, Nawroth PP (1997) Role of NF-κB in the mortality of sepsis. J Clin Invest 100:972–985
Christman JW, Holden EP, Blackwell TS (1995) Strategies for blocking the systemic effects of cytokines in the sepsis syndrome. Crit Care Med 23:955–963
Reinhart K, Wiegand-Lohnert C, Grimminger F, Kaul M, Withington S, Treacher D, Eckart J, Willatts S, Bouza C, Krausch D, Stockenhuber F, Eiselstein J, Daum L, Kempeni J (1996) Assessment of the safety and efficacy of the monoclonal anti-tumor necrosis factor antibody-fragment, MAK 195F, in patients with sepsis and septic shock: a multicenter, randomized placebo-controlled, dose-ranging study. Crit Care Med 24:733–742
Christman JW, Lancaster LH, Blackwell TS (1998) Nuclear factor κB: a pivotal role in the systemic inflammatory response syndrome and new target for therapy. Intensive Care Med 24:1131–1138
Katsuyama K, Hirata Y (2001) A pyrrolidinone derivative inhibits cytokine-induced iNOS expression and NF-κB activation by preventing phosphorylation and degradation of IκB-alpha. J Biochem (Tokyo) 129:585–591
Katsuyama K, Kojima R, Yokoyama S, Yanai M, Sueda N, Sugita M, Momose K, Yamada H (1998) N2733:1-[3-(3-Pyridyl)-acryloyl]-2-pyrrolidinone hydrochloride inhibits LPS-induced TNF-alpha production and improves survival in endotoxemic mice. Biosci Biotechnol Biochem 62:2177–2181
D’Orio V, Wahlen C, Rodriguez LM, Fossion A, Juchmes J, Marcelle R (1987) A comparison of Escherichia coli endotoxin single bolus injection with low dose endotoxin infusion on pulmonary and systemic vascular changes. Circ Shock 21:207–216
Sato Y, Weil MH, Tang W (1998) Tissue hypercarbic acidosis as a marker of acute circulatory failure (shock). Chest 114:263–274
Senftleben U (2003) NF-κB in critical diseases: a bad guy? Intensive Care Med 29:1873–1870
Cuzzocrea S, Rossi A, Pisano B, Di Paola R, Genovese T, Patel NSA, Cuzzocrea E, Ianaro A, Sautebin L, Fulia F, Chatterjee PK, Caputi AP, Thiemermann C (2003) Pyrrolidine dithiocarbamate attenuates the development of organ failure induced by zymosan in mice. Intensive Care Med 29:2016–2025
Szabó C, Wu CC, Gross SS, Thiemermann C, Vane JR (1993) Interleukin-1 contributes to the induction of nitric oxide synthase by endotoxin in vivo. Eur J Pharmacol 250:157–160
Volman TJ, Hendrika T, Verhofstad AA (2002) Improved survival of TNF-deficient mice during the zymosan-induced multiple organ dysfunction syndrome. Shock 17:468–472
Thiemermann C, Vane J (1990) Inhibition of nitric oxide synthesis reduces the hypotension induced by bacterial lipopolysaccharide in the rat in vivo. Eur J Pharmacol 182:591–595
Mitaka C, Hirata Y, Yokoyama K, Makita K, Imai T (2001) A selective inhibitor for inducible nitric oxide synthase improves hypotension and lactic acidosis in canine endotoxic shock. Crit Care Med 29:2156–2161
Thiemermann C (1995) Inhibition of nitric oxide synthase activity in circulatory shock: friend or foe? In: Fink MP, Payen D (eds) Role of nitric oxide in sepsis and ARDS, Vincent JL (ed) Update in intensive care and emergency medicine 24. Springer, Berlin Heiderberg, New York, pp 201–216
Griscavage JM, Wilk S, Ignarro LJ (1995) Serine and cysteine proteinase inhibitors prevent nitric oxide production by activated macrophages by interfering with transcription of inducible NO synthase gene. Biochem Biophys Res Commun 215:721–729
Maynard N, Bihari D, Beale R, Smithies M, Baldock G, Mason R, McColl I (1993) Assessment of splanchnic oxygenation by gastric tonometry in patients with acute circulatory failure. JAMA 270:1203–1210
O’Hair DP, Adams MB, Tunberg TC, Osborn JL (1989) Relationships among endotoxemia, arterial pressure, and renal function in dogs. Circ Shock 27:199–210
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mitaka, C., Hirata, Y., Narumi, Y. et al. Blockade of nuclear factor-κB activation prevents hypodynamic shock and gastric hypoperfusion induced by endotoxin in anesthetized dogs. Intensive Care Med 31, 718–723 (2005). https://doi.org/10.1007/s00134-005-2617-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2617-1