Abstract
Purpose
Mental health research has powerfully documented inequities related to characteristics, such as ethnicity and gender. Yet how and where disparities like unmet need occur have been more elusive. Drawing from a now modest body of research that deployed the Network Episode Model (NEM), we examine how individuals create patterns of response to mental health problems, influenced by the culture and resources embedded in their social networks.
Methods
The Person-to-Person Health Interview Study (P2P; N ~ 2,700, 2018–2021) provides representative, community-based, NEM-tailored data. Both descriptive, latent class and multinomial regression analyses mark mental health care-seeking patterns, including individuals consulted and activities used, as well as the influence of the structure and cultural content of social networks.
Results
Latent class analysis detected five pathways with good fit statistics. The Networked General Care Path (37.0%) and The Kin General Care Path (14.5%) differ only in whether friends are activated in using the general care sector. The Networked Multi-Sector Care Path (32.5%) and The Saturated Path (12.6%) involve family, friends, and both general and specialty care with only the latter expanding consultation to coworkers and clergy. The Null Path (3.3%), or no contacts, is not used as perceived problem severity increases. Network size and strength are associated with the more complex pathways that activate ties, respectively. Trust in doctors is associated with pathways that include specialty providers but not others at work or church. Race, age, and rural residence have specific pathway effects, while gender has no significant impact.
Conclusions
Social networks propel individuals with mental health problems into action. Tie strength and trust produce care responses that are fuller and more targeted. Considering the nature of homophily, results also suggest that majority status and college education are clearly implicated in networked pathways. Overall, findings support community-targeted rather than individually based efforts to increase service use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The onset of mental health problems presents individuals and society with three unique dilemmas. First, with no physical manifestations, great heterogeneity, few symptoms distinct from behavioral or biological repertories, and no measurable signs to bring to diagnosis, recognizing the problem is daunting for individuals and mental health providers alike [1]. Second, the persistence of public, personal, and provider-based stigma surrounding mental health [2]; the difficulties that individuals from diverse cultures or identities groups face in care [3]; and the documented fear of reprisal that medical providers, themselves, report in facing their own mental health problems [4] all diminish the public’s enthusiasm for seeking formal mental health care. Third, even if individuals want such care, the perennial mental health workforce shortage [5]; efforts to continually pass additional legislation to enforce parity efforts and equitable reimbursement for sustained mental health care (e.g., proposed H.R.1364—Parity Enforcement Act of 2021; see [6, 7]); and the diversion of the majority of U.S. mental health research funds from services, stigma and treatment innovation to a failed search for biomarkers [8] makes the search for care difficult. In essence, the science, the public, and the system all conspire to produce high levels of unmet need. Countering this discouraging profile are the facts that many treatments work [9]; mental health literacy in the public has improved [10]; frameworks, research and interventions to understand and reduce mental health disparities have grown [11,12,13]; legislation to prioritize physician mental health has passed [4]; and anti-stigma efforts have documented modest but real effects [14,15,16].
This summary of negative and positive conditions in the mental health landscape reveals a great deal of complexity and uncertainty surrounding the response to onset, care, and outcome. Yet, for the most part, the traditional approach to understanding who eventually gets into care focuses on individual factors and a “one-off event” [17: 140]. Individuals’ assessment and beliefs, their knowledge of insurance and access, and their social characteristics are the mainstay of research [18]. More recently, however, theoretical efforts have expanded to consider how these critical aspects are embedded in communities, both public and professional, where social interactions are the mechanism through which problems are recognized and services are provided. With the response to onset seen as a process that is often “peopled”, the Network Episode Model (NEM) [19, 20] represents one effort. Developed in direct response to the dominant individually focused, use-no use models, the NEM contextualized illness response by suggesting two key theoretical differences. First, tracing the entire set of actions, from discussion with family and friends to consultation with lay advisors to entering the healthcare system, shifts the focus to patterns or pathways to care. Second, by emphasizing that recognizing health problems, especially mental health problems, is difficult even for the educated, the role of social network ties become more central. Individuals in family, work, school, or other social settings hold (mis)knowledge, beliefs, and resources that can facilitate or delay entry into formal mental health care. Further, social network influence likely varies by the structure of ties (e.g., number and frequency), which provide the degree or “push” or influence, in combination with cultural scripts that suggest whether formal mental health care systems can be trusted.
Research employing the NEM has documented different patterns and pathways to care, diverse mental health care experiences (even for anxiety, depression, and mania/hypomania, the most common mental health concerns) and varying outcomes [21,22,23,24,25]. For example, among older individuals, coercion into mental health care was rare, while “muddling through” predominated [22]. Among African American youth, access to mental health services has been shown to be a relational and socially embedded process [26]. Different pathways were associated with diverse outcomes, including diagnosis, trusting working alliances, completing treatment protocols, or post-treatment adherence [21, 27,28,29,30]. Yet, for individuals with mental illness, the large and broadly functional social networks reported as they enter formal mental health care dropped over time, dramatically so compared to general population shifts in the same period [29]. Even online, gamers with more depressive symptoms may seek help by leveraging their networks via online channels [31]. As Boydell et al. [32: 184] note, networked pathways to care appear to be critical to understanding “how services and supports are received and experienced over time” (original emphasis).
Attention to matters of process, culture, networks, and inequality in health and health care is hardly new in sociomedical science (e.g., [33,34,35,36]). How individuals perceive the healthcare systems and its providers, particularly whether they trust physicians, has been a mainstay of understanding service use (e.g., [37,38,39]). The NEM made no claim of originality. It more intentionally conceptualized formal mental health care utilization as the result of the intersection of community and treatment systems, building a stronger bridge between the “social” and the “psychiatric” [40, 41]. Perhaps no surprise, then, that mental health care utilization researchers who focus on cultural minorities, cultures outside of the West, or other economically and socially disadvantaged populations often used the NEM [42]. For example, among Chinese Americans, conflict in the family network was associated with mental health care utilization [43], but traditional measures of family support were not (also [44, 45] on Korean Americans). Among African Americans, the contrast between kin networks being critical in everyday life but locked out from participation in community mental health centers translated into non-retention in care [46]. Several studies documented how migrants selectively activated “compatriots” (e.g., those with similar experiences), relying on them more heavily as their mental health career progressed and reducing the time to entering formal mental health care [25, 47, 48]. More generally, larger social networks resulted in greater utilization of mental health care among homeless individuals [49], and both youth and older adults [32, 50,51,52].
However, networks do not always facilitate utilization, as research on the “dark side” of social ties has documented [53]. In some contexts, networks may constrain behaviors and discourage seeking both formal and informal mental health care. For example, among those in Puerto Rico, larger, more supportive networks diminished the uptake of care-seeking patterns that included mental health providers [54] (also [55] on prenatal care). Finally, individuals often employ care providers and practices that never reach the formal mental health care system [56,57,58,59]. As Alegria et al. [13] conclude, community, family, friends, and individuals may encourage or block individuals’ referral, entry, or retention in mental health care or substance abuse treatment.
In total, the last 2 decades have compiled a promising and solid body of research that not only offers new insights but provides novel directions for formal and informal mental health care and interventions designed to facilitate pathways to care. Yet, comparatively speaking, little research directly ties community network cultures to individuals’ mental health care-seeking. In some cases (e.g., using statistics for organizational planning), the deep dive into process and communities is not required. However, when the target is to improve entry, retention, and effectiveness, looking to networks continues to be promising. Network data are hard to come by, because research designs that collect such data are resource and time intensive. On the quantitative side, they take more time to collect and require novel analytic tools beyond standard statistical approaches requiring independence of cases [41, 60]. On the qualitative side, efforts to precisely guide qualitative studies are rare and quite recent [61,62,63,64]. As Wyke et al. [65: 82–83] conclude, “The idea of a social network as the fundamental unit of analysis is attractive but is easier to articulate than to operationalize.”
Here, we take advantage of the Person-to-Person Health Interview Study (P2P), a representative sample of individuals (N ~ 2700) collected between 2018 and 2021 to explore mental health care-seeking pathways. Using P2P data on the structure of respondents’ health-targeted social networks and their trust in the medical system, we examine if and how these factors are related to the number, type, and patterns of mental health care-seeking for past-year problems seen to touch mental health. We draw from the NEM but take an exploratory approach because this stands among the few large-scale, population-representative studies that ask about networks, mental health care-seeking behavior, and mental health care utilization.
Mental health is an important concern in Indiana, where access and utilization of formal mental health care are limited and differential relative to characteristics, such as age, race, gender, rurality, and insurance coverage. A Kaiser Family Foundation fact sheet on mental health in Indiana reports levels of the three most common mental health concerns (anxiety, depression, and mania/hypomania) at levels slightly lower than but not significantly different from those for the United States overall in 2021 (28.6% in Indiana, 31.6% for the US, [66]) That same report indicates that a slightly higher percentage of Indiana residents needing formal mental health care reported not receiving those services relative to levels for the entire US (29.3% v. 26.9%, [66]). Health disparities are a significant problem in Indiana with about a third of Indiana residents reporting common mental health concerns and about a third of those reporting unmet need. Furthermore, the House Committee on Ways and Means reported that in 2020 Indiana had lower access to healthcare, rates of health insurance, average life expectancy, and median household income than the United States overall. Health inequities are more pronounced in areas of Indiana with higher proportions of non-white residents [67, see also 68, 69]. This study explores pathways to mental health care. In light of the clear presence of health disparities based on education, socioeconomic status, insurance status, race, and ethnicity a study that explores such pathways from the point of view of key characteristics associated with health disparities in the United States stands to provide unique information for policy change.
Methods
Data source and study sample
The Indiana University Person-to-Person Health Interview Study (P2P) is an omnibus health and wellness study based on face-to-face interviews, designed to study multilevel factors that shape health, using a stratified probability sample of households across the state of Indiana. In addition to demographics, the study collected information on a broad range of health behaviors and attitudes, service utilization and attitudes, employment history, environmental exposure through work and home, and an ego-centered network battery. The study was conducted with a target random sample of 2700 State residents selected to be representative on age, ethnicity, urbanicity, county (a proxy for economic status), and gender. Data were collected from October 23, 2018, to March 21, 2020 when interviewers were pulled from the field as COVID-19 became prevalent in Indiana. Interviews resumed from July 16, 2020 to June 30, 2021 (N = 2685). After deletion of respondents with missing age, race, sex, number of total adults in the household, or key mental health outcomes, the effective sample for this analysis is N = 2559 individuals.
Respondent enrollment occurred in two stages. First, our sampling design partners, NORC, developed a randomized state-level household sampling strategy to be reflective of the population distribution of the state but clustered within 50% of counties to facilitate data collection. This approach is identical to the approach used in the US General Social Survey, which NORC implements. Then, each household is approached and an adult is asked to describe all adult members of the household. From that list, a survey respondent is chosen at random to participate in the study. If they refuse to participate, the field interviewer moves on to the next randomly selected household on the list. Participation in the study requires only that a respondent be an adult cognitively able to respond to an interviewer administered survey. Thus, these data avoid the limitations of surveys using convenience samples or respondent panels, which are vulnerable to response and selection bias, particularly for those with lower education level or living in rural communities. Our focus here is on individuals who self-reported having a mental health/emotional problem in the past year (N = 400). Examining pathways to care from a population point of view requires that individuals or those around them suggest that there may be a problem. Of course, pathways can be examined in treated populations sampled from clinical records with interview follow-up [54] or looking at the service use of individuals with “need” determined by population-based diagnostic measures.Footnote 1
Measures
Mental health problem: severity and use variables
Measures were developed specifically for examining the response to self- or other-perceived mental health problems. Respondents were asked if they thought or someone around them thought that they (respondent) might have a mental health or emotional problem. For participants responding “yes”, follow-up questions included problem severity assessed on a four-point scale ranging from very serious (1), moderately serious (2), not very serious (3) to not serious at all (4). Eight single utilization items asked who they talked to (yes/no) about those problems: relative; friend; neighbor; coworker; minister, pastor, or priest; physician, nurse, physician’s assistant, nurse practitioner or community health worker; psychologist, psychiatrist, social worker or counselor; or nobody.
Network variables
Network data were collected using the PhenX Toolkit social network measures (https://www.phenxtoolkit.org/protocols/view/211101). Three variables included network size, a count of people respondents listed as important matters or health ties (range to 20). For each person listed, respondents rated relationship strength (scale 1–10). Average relationship strength served as a general measure of connection. For each, they also indicated how much they felt the ties trusted doctors to take care of people’s problems (responses: none, a little, some, a lot). Pro-medical cultural climate for each respondent was calculated as the percentage of ties who were thought to trust doctors “a lot”. The P2P did not do a second-stage interview of network ties as in some studies (e.g., [54]) because studies have reported that respondents accurately report information on network close or frequent ties [48, 70].
Sociodemographic, need, and cultural controls
Network variables are not the only correlates, given the solid body of research on mental health care disparities [13]. Social and cultural characteristics mark important limits on contacts [40, 54: 227]. Respondent age was calculated as the difference between date of interview and birthdate. Participants were asked about their current sex or gender: male, female, and other identities (e.g., transgender, non-binary/gender fluid). Due to the very small sample size of alternative identities, we use the simple male/female dichotomy. Race compares non-Hispanic white participants with all other races and ethnicities due to limited number of respondents, in line with Indiana’s population profile. Education was recorded as the highest level of education completed in five categories: less than high school, high school graduate/GED, some college (no degree), and technical certificates/associates degree, or college and higher. Rural status is based on the county residence determined by NORC’s Metropolitan/Micropolitan status codes. Table 1 provides the basic sample descriptives. In addition, perceived severity variable is included as a continuous variable.
Statistical analysis
Descriptive statistics reported demographics, mental health problems, and network variables. To identify pathways, latent class analysis used the eight utilization items. Automatic starting values for the Rho parameters were used and set a seed for reproducibility. No covariates were used in the initial pathway analyses. Selection of the final class model was based on model fit criteria, primarily the Bayesian Information criteria (BIC, lower values indicate better fit) and interpretability. Other fit statistics are also reported. To assess pattern correlates, multinomial regression used predicted class membership as the outcome with severity, network structure and culture, and demographic variables (age, gender, race, education, and rural status) as predictors.
Results
Table 2 presents the basic descriptive data on perceived mental health problems, social networks, and source of care. Of the four hundred individuals reported that they or someone they knew felt they had a mental health or emotional problem, most (77.1%) reported the problem as moderate or very serious. Respondents most frequently reported talking to relatives (74.0%); friends (67.3%); or a physician, physician’s assistant, nurse, nurse practitioner, or community health worker (49.5%) about their mental health or emotional problem. Respondents reported social networks with an average of about six unique members named across name generators (5.7), strong relationships with network members (average tie strength of 8.1 on a 1–10 scale), and that about half of their network members (50.4%) trusted doctors very much.
Pathways to care
The latent class analyses reveal five groups, based on patterns of communication related to the reported mental health or emotional problem (Table 3). With data density using a 40% probability of endorsing a care source, the largest pathway group (37%) was a Networked, General Care (NGC) pathway. Almost all these respondents spoke to family (72%) and friends (96%) with nearly half (43%) visiting a general health care provider. The next largest group (32.5%) activated varied and numerous sources of advice and care. In this Networked Multi-Sector Care (NMC) path, respondents spoke to family (62%) and friends (55%) with two-thirds visiting a specialty mental health provider (66% mentioning psychologist, psychiatrist, social worker, or counselor) and nearly half accessing providers in the general care sector (45%). In the Kin General Care (KGC, 14.5%) path, all spoke to relatives (100%) but fewer than half visited a general medical sector (40%). While the Saturated Path (SP) represents only 12.8% of respondents, they activated the most sources of care—family (100%); friends (97%); coworkers (58%); a minister, pastor, or priest (45%); and both general (88%) and specialty sector (92%) providers. The smallest group (3.3%) spoke to no one, representing a Null path (NP).
Pathway correlates
The multinomial regression results reveal the relationship between pathways, network and need factors, and demographic controls (Table 4). Wald Chi-square tests provide an assessment of whether each correlate has an overall effect on pathway type. Severity of the problem and network size significantly discriminated across care pathways. Age and race were marginally associated.
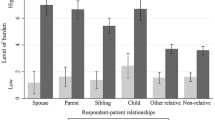
A more fine-grained analysis requires the sets of multinomial regressions where correlates are examined on each contrast of two pathways. Figure 1a, b provides a graphical summary of effects from the eight multivariate tables (one full contrast provided in Appendix 1, full set on request). These analyses, more detailed and relatively more complicated than typical regression results, are interpreted as follows: each column represents a reference category in a multivariate regression that examines the impact of independent variables on whether individuals were more likely to travel a different pathway compared to the reference. Each table row provides the effects of an independent variable on that comparison for a particular comparison group, indicated by a color-coded whisker plot. It should be noted that the whisker plots associated with the reference category are not included. For example, the upper left corner of Fig. 1a represents the four analyses done to see if and how network size affects whether individuals activated an alternate pathway compared to the Networked General Care Pathway (NGC), with the blue whisker plot corresponding to NGC not shown. The one, starred effect indicates a significant effect of network size—those with larger networks are more likely to report the purple path (SP) compared to the reference NGC. Substantively, the interpretation suggests that those with larger networks are likely to go beyond activating family and physician helpers (in the NGC), because the saturated path includes coworkers, friends, the clergy, and specialty providers. Looking across all cells in that top row indicates that larger networks make the saturated pathway the most common as network size increases. In turn, this indicates that when human resources are available, individuals will activate them and social networks can facilitate help-seeking across the board.
a Odds ratios and standard errors for multinomial regression models across all reference categories, continuous and ordinal variables. Relevant reference category is indicated by color. Significant effects are noted with an asterisk. Person-to-Person (P2P) Health Interview Survey, 2018–2021 (effective sample size 2559). b Odds ratios and standard errors for multinomial regression models across all reference categories, binary variables. Relevant reference category is indicated by color. Significant effects are noted with an asterisk. Person-to-Person (P2P) Health Interview Study, 2018–2021 (effective sample size 2559)
The network strength findings (next set of rows) indicate that most of the action is located relative to the Null Path. This indicates that, controlling for network size, those who have stronger ties are more likely to travel any pathway rather than not do anything at all. Trust in doctors does not have many significant effects; however, trust predisposes individuals to paths that include the specialty sector (see columns 1, 3) but does not generally increase types of care (non-significance in column 5). Older respondents were more likely to report pathways that included relatives alone (columns 1,3), but when they do include friends, they are more likely to include specialty care (columns 1,4).
In Fig. 1b, individuals who reported their problem to be moderate or serious were more likely to travel any path than the Null Path (column 2); however, they were also more likely to end up in pathways that included specialty providers (columns 1, 3). Whites were more likely to travel pathways that included specialty providers while individuals from minority populations were less likely to do so (column 1). Gender had no effect on pathways. The effects of education come into play only for those with college/advanced degrees. In this case, respondents travel any pathway rather than do nothing and are less likely to stop at the general care sector. Rurality has inconsistent effects but suggests that rural residents are more likely to do nothing than engage either a lot of others or, if they do get formal care, tend to activate only kin and general medical care (column 5).
Discussion
Our ability to understand the role that “the social” plays in mental illness is undermined, at least in part, by a reliance on a view that focuses on the individual alone. While sociodemographic categories tap into the social and cultural lives of individuals, providing critical insights, they are less well equipped to see how those factors operate to create inequalities. Research in many areas, including employment, migration and immigration, and birth control, has established that human connections are often those active ingredients creating disparities, even for health behavior change [71]. Network research, which traces the human connections that surround individuals and stand as the sources of formal and informal care than can be activated during a health crisis, may offer novel findings. Yet, because network data collection is messy, complicated, and more time-consuming than the traditional quantitative or qualitative approaches [60], social network studies are more rare. However, we argue that the Network Episode Model may be a better theoretical match, because the search for care, especially for mental health problems, also appears to be messy and complicated.
The findings reported here are far from meeting the immensity of that challenge. However, we attempted to contextualize the search for mental health care by connecting individuals to whom they consulted about their problem and enumerating the structure and cultural content of those network ties. In this representative sample, we find that almost 15% of individuals reported problem recognition by self or other and their response pathways varied from doing nothing (a very small number) to activating lay and professional ties across many sectors of the community, including family, friends, coworkers, and general and specialty medical providers. Both networks and severity propel individuals into care-seeking behavior. While those with strong ties are likely to seek care of some sort, having larger networks translates into accessing a richer set of options. Cultural beliefs in those networks matter to some extent, since networks with strong trust in doctors are associated with pathways that access the general and specialty medical sectors. Individuals from the majority white population, and those with higher levels are education, report pathways to the specialty sector, signaling a continued disparity.
Of course, this study is not without problems that raise questions about disparities. In our representative sample, we find few race effects. While it may be unsurprising that minority population respondents are less likely to report pathways that include psychiatric care providers than are majority individuals, there are both sampling and prevalence limits here. First, even with a population-based sample of nearly 3000 individuals, we had only a small group that reported self- or other-perceived need, as indicated above. Second, this is compounded by fielding the study in a state that has about 10% black population and another 6% other races and/or ethnicities. Only an oversample would offer a more solid basis for examining race and ethnic disparities and the social processes involved in the search for mental health care. However, in a state that is highly rural 78% of counties, and where education ranks 46th nationally in adults with a college degree, we find both residence and education in operation to some extent. Finally, the stem of the mental health/emotional problem question does not distinguish between common or severe mental health problems or distinguish between individuals who were self-aware or who were nudged, or even coerced, by others to recognize and act on their mental health issues. We know that pathways, and network effects on pathways, are shaped by whether coercion or agency is at work in seeking care [22, 54]. Finally, as noted earlier, we have data from respondents on their social network members. We cannot ascertain whether respondents’ self-reports are accurate interpretations of the beliefs and opinions of their network ties. Ultimately, the NEM may be best suited to a mixed method approach or to one that includes oversamples of minority populations [72]. To that end, a mixed-methods study involving qualitative interviews exploring pathways to care, particularly among minority populations is underway and subsequent survey administrations will feature oversamples of minority populations. Subsequent studies will also disaggregate respondents according to assessments of depression, anxiety, and mania/hypomania.
Nevertheless, our goal here was to reconsider the role of “the social” in understanding the lay and professional resources that individuals use over the course of seeking care for a mental health problem by looking to the structure and culture of their social networks. We have established that there are unique pathways to mental health care. Further, social networks and the nature of the problem matter most in the response to mental health problems. Having stronger ties translates into eliciting a response, but only having many ties and ones that support medical solutions result in activating a lot of helpers, including those in the specialty mental health sector. As we see social ties exert influence, it becomes imperative to think about utilization as a community response, even if we think of “small worlds” within communities. In turn, policy and services designed to alleviate the burden of mental health problems might be more effective if they shift from a focus on individuals to a focus on their communities.
Data availability
The data that support the findings of this study are not publicly available at the time of publication. The data are, however, available from the authors upon reasonable request and with the permission of the Person-to-Person Health Interview Study Principal Investigators. To inquire about access to P2P data, please email irsay@iu.edu.
Notes
Instrumentation varies with the study population. For those in care, the pathway stem question would be: How did you get here? For population-based samples like the one here, the stem question is the problem recognition question listed in the text.
References
García-Gutiérrez MS, Navarrete F, Sala F, Gasparyan A, Austrich-Olivares A, Manzanares J (2020) Biomarkers in psychiatry: concept, definition, types and relevance to the clinical reality. Front Psychiatry. https://doi.org/10.3389/fpsyt.2020.00432
Pescosolido BA (2013) The public stigma of mental illness: what do we think; what do we know; what can we prove? J Health Soc Behav 54(1):1–21. https://doi.org/10.1177/0022146512471197
Miranda J, McGuire TG, Williams DR, Wang P (2008) Mental health in the context of health disparities. Am J Psychiatry 165(9):1102–1108. https://doi.org/10.1176/appi.ajp.2008.08030333
Acep.org (2022) Your advocacy at work: President Biden Signs Dr. Lorna Breen Bill. Acep.org. Accessed 24 May 2022
Olfson M (2016) Building the mental health workforce capacity needed to treat adults with serious mental illnesses. Health Aff 35(6):983–990. https://doi.org/10.1377/hlthaff.2015.1619
Carlo AD, Barnett BS, Frank RG (2020) Behavioral health parity efforts in the US. JAMA 324(5):447–448. https://doi.org/10.1001/jama.2020.3505
Frank RG (2018) Reflections on the mental health parity and addiction equity act after 10 years. Milbank Q 96(4):615–618. https://doi.org/10.1111/1468-0009.12346
Insel T (2022) Healing: our path from mental illness to mental health. Penguin Press, New York
Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, Roiser JP, Bockting CLH, O’Connor RC, Shafran R, Moulds ML, Craske MG (2018) The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry 5(3):237–286. https://doi.org/10.1016/s2215-0366(17)30513-8
Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG (2010) “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry 167(11):1321–1330. https://doi.org/10.1176/appi.ajp.2010.09121743
Alegria M, Lloyd JJ, Ali N, DiMarzio K (2021) Improving equity in healthcare through multilevel interventions. In: Dankwa-Mullan I, Pérez-Stable EJ, Gardner KL, Zhang X, Rosario AM (eds) The science of health disparities research. Wiley Online Library, pp 257–287. https://doi.org/10.1002/9781119374855.ch16
Alegría M, NeMoyer A, Falgàs Bagué I, Wang Y, Alvarez K (2018) Social determinants of mental health: where we are and where we need to go. Curr Psychiatry Rep 20(11):95–95. https://doi.org/10.1007/s11920-018-0969-9
Alegria M, Pescosolido BA, Williams S, Canino G (2011) Culture, race/ethnicity and disparities: fleshing out the socio-cultural framework for health services disparities. In: Pescosolido BA, Martin JK, McLeod JD, Rogers A (eds) Handbook of the sociology of health, illness, and healing: A blueprint for the 21st century. Springer, pp 363–382
Henderson C, Robinson E, Evans-Lacko S, Corker E, Rebollo-Mesa I, Rose D, Thornicroft G (2016) Public knowledge, attitudes, social distance and reported contact regarding people with mental illness 2009–2015. Acta Psychiatr Scand 134(Suppl 446):23–33. https://doi.org/10.1111/acps.12607
Stuart H, Sartorius N (2022) Paradigms lost, paradigms found: lessons learned in the fight against the stigma of mental illness. Oxford University Press, Oxford
Pescosolido BA, Perry BL, Krendl AC (2020) Empowering the next generation to end stigma by starting the conversation: bring change to mind and the College Toolbox Project. J Am Acad Child Adolesc Psychiatry 59(4):519–530. https://doi.org/10.1016/j.jaac.2019.06.016
Mackian S, Bedri N, Lovel H (2004) Up the garden path and over the edge: where might health-seeking behaviour take us? Health Policy Plan 19(3):137–146. https://doi.org/10.1093/heapol/czh017
Tipping G, Segall MM (1995) Health care seeking behaviour in developing countries: an annotated bibliography and literature review. Development Bibliography, No. 12. Institute of Development Studies, University of Sussex, United Kingdom
Pescosolido BA (1991) Illness careers and network ties: a conceptual model of utilization and compliance. In: Albrecht GL, Levy JA (eds) Advances in medical sociology. JAI Press, Stamford, pp 161–184
Pescosolido BA (2006) Of pride and prejudice: the role of sociology and social networks in integrating the health sciences. J Health Soc Behav 47(September):189–208
Alang SM, McAlpine DD (2018) Pathways to mental health services and perceptions about the effectiveness of treatment. Soc Ment Health 9(3):388–407. https://doi.org/10.1177/2156869318802341
Berard LDH, Mackenzie CS, Reynolds KA, Thompson G, Koven L, Beatie B (2020) Choice, coercion, and/or muddling through: older adults’ experiences in seeking psychological treatment. Soc Sci Med 255:113011. https://doi.org/10.1016/j.socscimed.2020.113011
Reynolds K, Medved M, Mackenzie CS, Funk LM, Koven L (2020) Older adults’ narratives of seeking mental health treatment: making sense of mental health challenges and “muddling through” to care. Qual Health Res 30(10):1517–1528. https://doi.org/10.1177/1049732320919094
Pescosolido BA, Wright ER, Alegria M, Vera M (1998) Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med Care 36(7):1057–1072
Antoniades J, Mazza D, Brijnath B (2018) Agency, activation and compatriots: the influence of social networks on health-seeking behaviours among Sri Lankan migrants and Anglo-Australians with depression. Sociol Health Illn 40(8):1376–1390. https://doi.org/10.1111/1467-9566.12764
Planey AM, Smith SM, Moor S, Walter TD (2019) Barriers and facilitators to mental health help-seeking among African American youth and their families: a systematic review study. Child Youth Serv Rev 101:190–200
Novins DK, Spicer P, Fickenscher A, Pescosolido B (2012) Pathways to care: narratives of American Indian adolescents entering substance abuse treatment. Soc Sci Med 74(12):2037–2045
Pullen EL (2014) Social networks, drug use, and drug abuse help-seeking: a test of the network episode model among African American women. University of Kentucky, Lexington
Perry BL, Pescosolido BA (2012) Social network dynamics in the face of biographical disruption: the case of “first timers” with mental illness. Am J Sociol 18(1):134–175
Usmanov GS, Wright ER, Anderson RK (2021) Treatment network typologies and the working alliance of clients with serious mental illness. Soc Ment Health 12(1):17–31. https://doi.org/10.1177/21568693211001432
Prochno T, Patterson MS, Hartnell L, Umstattd Meyer MR (2020) Depressive symptoms associations with online and in person networks in an online gaming community: a pilot study. Ment Health Rev J 25(1):21–33. https://doi.org/10.1108/MHRJ-11-2019-0044
Boydell KM, Volpe T, Gladstone BM, Stasiulis E, Addington J (2013) Youth at ultra high risk for psychosis: using the Revised Network Episode Model to examine pathways to mental health care. Early Interv Psychiatry 7(2):170–186. https://doi.org/10.1111/j.1751-7893.2012.00350.x
Clausen JA, Yarrow MR (1955) Pathways to the mental hospital. J Soc Issues 11:25–32
Horwitz AV (1977) Social networks and pathways to psychiatric treatment. Soc Forces 56(1):86–105
Kleinman A (1980) Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. University of California Press, Berkeley
Pescosolido BA, Kronenfeld J (1995) Health, illness, and healing in an uncertain era: challenges from and for medical sociology. J Health Soc Behav 35(1):5–33
Musa D, Schulz R, Harris R, Silverman M, Thomas SB (2009) Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health 99(7):1293–1299. https://doi.org/10.2105/ajph.2007.123927
Rosenstock IM (2005) Why people use health services. Milbank Q. https://doi.org/10.1111/j.1468-0009.2005.00425.x. (online‐only-online‐only)
Trent MJ, Salmon DA, MacIntyre CR (2021) Using the health belief model to identify barriers to seasonal influenza vaccination among Australian adults in 2019. Influenza Other Respir Viruses 15(5):678–687. https://doi.org/10.1111/irv.12843
Morgan C, Mallett R, Hutchinson G, Leff J (2004) Negative pathways to psychiatric care and ethnicity: the bridge between social science and psychiatry. Soc Sci Med 58(4):739–752. https://doi.org/10.1016/S0277-9536(03)00233-8
Pescosolido BA (2011) Organizing the sociological landscape for the next decades of health and health care research: the network episode model III-R as cartographic subfield guide. In: Pescosolido BA, Martin JK, McLeod JD, Rogers A (eds) Handbook of the sociology of health, illness, and healing: Blueprint for the 21st century. Springer, New Yori, pp 39–66
Uehara ES (2001) Understanding the dynamics of illness and help-seeking: event structure analysis and a Cambodian American narrative of “spirit invasion.” Soc Sci Med 52(4):519–536
Abe-Kim J, Takeuchi D, Hwang W-C (2002) Predictors of help seeking for emotional distress among Chinese Americans: family matters. J Consult Clin Psychol 70(5):1186
Lee H, Fawcett J, Yang JH, Hann H-W (2012) Correlates of hepatitis B virus health-related behaviors of Korean Americans: a situation-specific nursing theory. J Nurs Scholarsh 44(4):315–322. https://doi.org/10.1111/j.1547-5069.2012.01468.x
Lee H, Hann H-W, Yang JH, Fawcett J (2011) Recognition and management of HBV infection in a social context. J Cancer Educ 26(3):516–521. https://doi.org/10.1007/s13187-011-0203-5
Hack SM, Larrison CR, Bennett ME, Lucksted A (2019) Experiences of African–American men with serious mental illness and their kinship networks within the mental health care system. J Ethn Cult Divers Soc Work 28(1):98–114. https://doi.org/10.1080/15313204.2019.1570888
Devillanova C (2008) Social networks, information and health care utilization: evidence from undocumented immigrants in Milan. J Health Econ 27(2):265–286. https://doi.org/10.1016/j.jhealeco.2007.08.006
Maglalang DD, Castro ABd, Gee G, Sabbath EL, Tran TV, Takeuchi DT (2020) Associations of sociodemographic factors with health-related social networks among pre-migration Filipinos. Soc Work Public Health 35(8):669–678. https://doi.org/10.1080/19371918.2020.1822977
Bonin J-P, Fournier L, Blais R (2007) Predictors of mental health service utilization by people using resources for homeless people in Canada. Psychiatr Serv 58(7):936–941. https://doi.org/10.1176/ps.2007.58.7.936
Lindsey MA, Korr WS, Broitman M, Bone L, Green A, Leaf PJ (2006) Help-seeking behaviors and depression among African American adolescent boys. Soc Work 51(1):49–58. https://doi.org/10.1093/sw/51.1.49
Stiffman AR, Pescosolido B, Cabassa LJ (2004) Building a model to understand youth service access: the gateway provider model. Ment Health Serv Res 6(4):189–198
Xiao Y, Lindsey MA (2021) Adolescent social networks matter for suicidal trajectories: disparities across race/ethnicity, sex, sexual identity, and socioeconomic status. Psychol Med. https://doi.org/10.1017/s0033291721000465
Villalonga-Olives E, Kawachi I (2017) The dark side of social capital: a systematic review of the negative health effects of social capital. Soc Sci Med 194:105–127. https://doi.org/10.1016/j.socscimed.2017.10.020
Pescosolido BA, Brooks-Gardner C, Lubell KM (1998) How people get into mental health services: stories of choice, coercion and ‘muddling through’ from ‘first-timers.’ Soc Sci Med 46(2):275–286
St Clair PA, Smeriglio VL, Alexander CS, Celentano DD (1989) Social network structure and prenatal care utilization. Med Care 27(8):823–832. https://doi.org/10.1097/00005650-198908000-00006
Ward H, Mertens TE, Thomas C (1997) Health seeking behaviour and the control of sexually transmitted disease. Health Policy Plan 12(1):19–28. https://doi.org/10.1093/heapol/12.1.19
Edmonds JK, Hruschka D, Bernard HR, Sibley L (2012) Women’s social networks and birth attendant decisions: application of the network-episode model. Soc Sci Med 74(3):452–459. https://doi.org/10.1016/j.socscimed.2011.10.032
Figuereo V, Calvo R (2018) Latinx use of traditional health care: the social network effect. Health Soc Work 43(4):217–225. https://doi.org/10.1093/hsw/hly024
Kikuzawa S, Pescosolido B, Kasahara-Kiritani M, Matoba T, Yamaki C, Sugiyama K (2019) Mental health care and the cultural toolboxes of the present-day Japanese population: examining suggested patterns of care and their correlates. Soc Sci Med 228:252–261
Perry BL, Pescosolido BA, Borgatti SP (2018) Egocentric network analysis: foundations, methods, and models. Structural analysis in the social sciences. Cambridge University Press, New York
Beatie BE, Mackenzie CS, Thompson G, Koven L, Eschenwecker T, Walker JR (2020) Exploring older adults’ experiences seeking psychological services using the network episode model. Ageing & Society:1–24
Dobbie F, Reith G, McConville S (2017) Utilising social network research in the qualitative exploration of gamblers’ social relationships. Qual Res 18(2):207–223. https://doi.org/10.1177/1468794117710323
Heath S, Fuller A, Johnston B (2009) Chasing shadows: defining network boundaries in qualitative social network analysis. Qual Res 9:645–661
Small ML, Calarco JM (2022) Qualitative literacy: a guide to evaluating ethnographic and interview research. University of California Press, Oakland
Wyke S, Adamson J, Dixon D, Hunt K (2013) Consultation and illness behaviour in response to symptoms: a comparison of models from different disciplinary frameworks and suggestions for future research directions. Soc Sci Med 86:79–87. https://doi.org/10.1016/j.socscimed.2013.03.007
Mental Health in Indiana Fact Sheet. KFF. https://www.kff.org/statedata/mental-health-and-substance-use-state-fact-sheets/indiana/. Accessed Feb 2023
House Ways and Means Committee (2021) Indiana health equity facts, 2020. Washington, DC
United Health Foundation (2022) America’s health rankings annual report 2021: Indiana summary. https://www.americashealthrankings.org/learn/reports/2021-annual-report/state-summaries-indiana. Accessed 2022
Rawl SM, Dickinson S, Lee JL, Roberts JL, Teal E, Baker LB, Kianersi S, Haggstrom DA (2019) Racial and socioeconomic disparities in cancer-related knowledge, beliefs, and behaviors in Indiana. Cancer Epidemiol Biomark Prev 28(3):462–470
Green HD, Hoover MA, Wagner GJ, Ryan GW, Ssegujja E (2013) Measuring agreement between egos and alters: understanding informant accuracy in personal network studies. Field Methods 26(2):126–140. https://doi.org/10.1177/1525822X13492676
Hunter RF, McAneney H, Davis M, Tully MA, Valente TW, Kee F (2015) “Hidden” social networks in behavior change interventions. Am J Public Health 105(3):513–516. https://doi.org/10.2105/ajph.2014.302399
Pescosolido BA, Wright ER (2004) The view from two worlds: the convergence of social network reports between mental health clients and their ties. Soc Sci Med 58:1795–1806
Acknowledgements
We acknowledge support from the Indiana Consortium for Mental Health Services Research, the Irsay Institute, Indiana University’s Vice President for Research, the College of Arts and Sciences and the Indiana University Grand Challenge—Precision Health Initiative. We thank Alex Capshew and Karen Tucker for their continuous support on the P2P Study. In addition, we thank the editors of the special issues for their guidance and members of the working group, especially Annahita Ehsan and Milena Bister for their comments on earlier drafts of this paper.
Funding
The research leading to these results received internal funding from Indiana University under the Grand Challenges Program—Precision Health Initiative.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the study conception, design, and data collection. BAP is PI of the P2P study and HDG was the Project Director. Analysis was performed by HDG. The first draft of the manuscript was written by BAP. Both authors contributed to subsequent versions of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board IRB00000222 of Indiana University (September 24, 2018; Study #180341862).
Appendix 1
Appendix 1
See Table
5.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Green, H.D., Pescosolido, B.A. Social pathways to care: how community-based network ties shape the health care response of individuals with mental health problems. Soc Psychiatry Psychiatr Epidemiol 59, 431–442 (2024). https://doi.org/10.1007/s00127-023-02476-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-023-02476-2