Abstract
Purpose
Research has highlighted that the exposure of healthcare professionals to the COVID-19 pandemic for over two years can lead to the development and persistence of symptoms characteristic of Post-Traumatic Stress Disorder (PTSD), with serious consequences on both the individual well-being and the quality of care provided. The present study was aimed at investigating the role of benefit finding in moderating post-traumatic stress symptoms (PTSS) over time.
Methods
The longitudinal study, conducted between April and October 2020, involved 226 Italian health workers (44.7% nurses and midwives, 35% doctors, 20.3% technical and rehabilitation professionals), who filled out an online survey at the beginning of the study (T1), after three months (T2), and after six months (T3).
Participants (77.4% women; mean age = 41.93, SD = 12.06) completed the PTSD Checklist for DSM-5 (PCL-5) and Benefit Finding, a 17-item questionnaire measuring the perceived level of positive consequences derived from stressful experiences. A hierarchical regression analysis highlighted the moderating effect of benefit finding (T2) on the association between PTSS values at T1 and T3.
Results
A buffering effect was observed, with higher benefit finding levels reducing the magnitude of the bivariate association between PTSS assessed at the beginning and at the end of the study.
Conclusion
Findings suggest the potential mental health related benefits of interventions allowing health professionals to identify positive aspects in the experience of working under prolonged emergency circumstances, such as the pandemic ones.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Italy was the first European country to be strongly hit by the SARS-CoV-2 outbreak. The first national lockdown was declared on March 8 and lasted until May 3, 2020; a gradual decrease in COVID-19 cases was observed between May and mid-August, followed by a growing incidence trend and a renewed outbreak in October and November 2020 [1].
Worldwide, several studies explored mental health disorders during the pandemic in the general population; results showed a high prevalence of Post-Traumatic Stress Symptoms (PTSS), and Post-Traumatic Stress Disorder (PTSD), together with anxiety and depression [2,3,4,5,6,7,8]. Similar results were found among healthcare workers (HWs) in different countries [9,10,11,12,13]. Especially during the first and sudden outbreak of the pandemic, HWs experienced remarkable strain in their frontline role, due to dearth of protective equipment, exposure to high infection risk, and lack of available treatment protocols for assisting patients infected by Sars-Cov-2, especially when the disease progression led to critical conditions. Not surprisingly, several studies conducted across countries identified high levels of PTSS among HWs [14,15,16]. As concerns Italian HWs, in a survey conducted during the first pandemic outbreak almost half of the participants reported presence of PTSS [17]; in another work, 26.2% of the sample met the criteria for a provisional PTSD diagnosis [18].
According to the International Classification of Diseases (ICD-11) [19], PTSD development is strongly associated with exposure to a trauma, defined as an extremely threatening or horrific event or series of events. Similarly, the current diagnostic and statistical manual of mental disorders (DSM-5) defines PTSD as a psychological condition that can occur after exposure to a potentially traumatic event [20]. As highlighted in recent works, the COVID-19 pandemic and associated consequences could be considered as a potentially traumatic event in both classification systems [21, 22]. According to the DSM-5, a PTSD diagnosis requires the presence of PTSS including re-experiencing the traumatic event, avoidance of related stimuli, intrusive behaviors, and worsening cognition and mood after the traumatic event. A large body of research showed that PTSS and PTSD are associated with general distress and a higher risk of developing both physical and mental co-morbidities [23,24,25].
From a complementary perspective, an increasing number of studies have been focused on the individual and environmental resources that can be mobilized or developed to cope with or adapt to stressful events and potentially life-threating conditions [26,27,28,29,30,31]. Among these resources, benefit finding (BF) is defined as the identification of benefits from adversities. Benefits can be detected at the individual, relational and transcendent levels; they include, for example, increased appreciation for life, awareness of deepened interpersonal relationships, enhanced sense of spirituality, and life purpose [32,33,34,35,36]. Benefit finding has been associated with optimal adaptation to stressful situations, including pandemics [37, 38]. Both perception of and active search for benefits deriving from stressful events have been accounted for as cognitive meaning-making reappraisal strategies promoting individual well-being [39,40,41].
The identification and acknowledgement of positive contributions from traumatic experiences are an important resource in coping with life-threating situations [42, 43]. It is also a core component of Post-Traumatic Growth (PTG) [44, 45], defined as the process allowing individuals who are coping with trauma or life crises to strengthen their perceptions of self, others, and the meaning attributed to the traumatic experience itself [45]. Although similar, PTG and benefit finding differ in terms of both predictors and development patterns [46, 47]. Concerning predictors, Sears and colleagues [47] found a significant longitudinal association between BF and the personal characteristics of optimism and hope; this relationship was not confirmed for PTG. Research works also suggested different timing in the emergence and development of these two processes, with BF potentially starting immediately after the traumatic experience, and PTG requiring more time (i.e. weeks/months/years), due to the associated in-depth restructuring process [43, 47]. Overall, most studies addressing positive contributions following adversities or trauma were focused on PTG and associated dimensions, while only limited attention was devoted to benefit finding; efforts within this research area were mainly aimed at investigating the relationship between BF and adaptation to stress/life-threating events. Results were however controversial: While a significant association was identified in some studies between BF and lower or decreased levels of distress [32], other works did not confirm this relationship [47, 48]. The even fewer studies devoted to the investigation of the moderating role of BF on psychological distress also provided inconsistent results. In some of them, a significant interaction emerged between BF and severity of stressors in predicting improved psychological adjustment among disaster survivors [49] and women living with HIV/AIDS [50]; BF was also found to buffer the relationship between combat stress and PTSD symptoms among active soldiers following a 15-month deployment, but only under conditions of supportive officer leadership [51]. Opposite patterns were instead detected in other studies, in which the interaction between high levels of BF and breast cancer severity predicted worse mental health outcomes over time [36].
Within the international literature exploring the psychological correlates of the COVID-19 pandemic, only a limited amount of studies was aimed at investigating PTG and BF, both in the general population and among HWs. Results from a large-scale Chinese survey involving nurses showed that 39% of participants experienced PTG; further, nurses working at COVID-19 hospitals and caring for patients in critical care units reported higher PTG scores than nurses not engaged in these services [52].
As for BF, results from the general population showed that mortality concerns related to COVID-19 were cross-sectionally associated with higher BF values; BF was, in turn, positively correlated with life satisfaction, meaning in life, self-esteem, and resilience, while negatively correlated with levels of depression and stress [53].
BF was also found to longitudinally mediate the relationship between support seeking and well-being among Chinese participants from the general population during the COVID-19 pandemic [37].
To the best of our knowledge, no longitudinal studies were yet conducted to jointly monitor PTSS and BF during the COVID-19 pandemic in a population specifically exposed to the related strain and traumatic experiences, such as health professionals. In particular, no longitudinal studies were conducted to investigate the moderating role of benefit finding on PTSS development among these workers.
Study aims
The current study was aimed at investigating: (a) PTSS and BF development among Italian HWs actively working during the COVID-19 pandemic, and (b) to test the moderating role of BF on PTSS development across time. Due to the unpredictable development of the COVID-19 pandemic, no a priori hypotheses were formulated for the first aim (a); concerning the second aim (b), the identification of benefits from adversities related to the COVID-19 pandemic was hypothesized to buffer the magnitude of the association between participants’ PTSS measured at the beginning and at the end of the longitudinal study.
Method
Procedures and participants
The present study was conducted between April and October 2020, and consisted in three consecutive waves of data collection: April 15 to May 15 (T1), July 6 to August 6 (T2), and October 14 to October 30 (T3). Data on levels of PTSS were collected at T1, T2, and T3, while perceived BF was assessed at T2 and T3. Participants were HWs actively working in Lombardy, the Italian region in which the highest rates of contagion and deaths were recorded during the first pandemic outbreak [54, 55]. Potential participants were contacted through an e-mail message containing detailed information on the study features and the link to the online questionnaires, which was sent to HW associations in Lombardy with the invitation to forward it to their members. Both acknowledgment and signature of the informed consent form were mandatory to access the questionnaires. Anonymity was granted by inviting participants to create an individual alphanumeric code, to be used across the three assessment waves.
Measures
All participants completed two self-reported measures:
The Post-Traumatic Stress Disorder Checklist for DSM-5 (PCL-5) [56, 57], a 20-item measure assessing PTSS severity experienced over the previous month on scales ranging from 0 ‘not at all’ to 4 ‘extremely’. A provisional diagnosis of PTSD can also be formulated when the PCL-5 score is ≥ 33 [57]. The PCL-5 was completed at T1, T2 and T3.
Benefit Finding (BF) [32, 36], a 17-item measure assessing the perception of positive contributions to one’s life deriving from stressful and life-threatening experiences. Answers are provided through a 1 ‘I disagree a lot’ to 5 ‘I agree a lot’ scale; higher scores reflect higher perceived benefit; BF was assessed at T2 and T3.
Socio-demographic and work-related data included age, gender, profession and job seniority; in addition, at T2 and T3 participants were also asked to report if they had been assigned to a COVID-19 department since T1.
Data analysis
As a first step, descriptive statistics of the study measures were calculated. Cochran’ Q was employed to longitudinally assess changes, across time, in the frequency of participants meeting criteria for a provisional PTSD diagnosis; differences in PTSS scores at T1, T2, and T3 were tested using a repeated measures ANOVA followed by post-hoc comparisons with Bonferroni correction; BF levels (T2, T3) were also compared using a Student t-test for paired samples. Data were checked for repeated measures ANOVA and Student t-test assumption violations; namely, presence of extreme outliers together with normality assumption were inspected for both analyses; the ANOVA assumption of sphericity was also tested through Mauchly’s test.
Subsequently, Pearson correlations were calculated to assess the magnitude of associations between PTSS and BF both cross-sectionally and at different time points. Regardless of statistical significance, only values ≥|0.30| were considered as meaningful. Values between |0.30| and |0.49| were interpreted as indices of low correlation, values between |0.50| and |0.69| as indices of moderate correlation, and values ≥|0.70| as indices of high correlation between variables [58].
A hierarchical linear regression analysis using Ordinary Least Square (OLS) estimation technique was performed to test for the direct effects of PTSS (T1) and BF (T2) on PTSS (T3), as well as the moderating effect of BF (T2) on the relationship between PTSS at T1 and T3. Demographic and job-specific dimensions were entered in the regression model as control variables. Data were checked for violations of regression assumptions. In particular, linearity and normality of residuals were investigated through comparison of residual vs fitted values and Q-Q plots visual inspection, respectively; the absence of autocorrelation in residuals was assessed using the Durbin-Watson test while the Breusch-Pagan test investigated heteroscedasticity; as final steps, variance inflation factor (VIF) and leverages inspection were employed to detect multicollinearity issues and influential data points, respectively. Categorical variables with three or more levels were dummy coded; a reference category was selected and employed. Significance of regression coefficients was estimated through 95% confidence intervals (CI) from 2,000 bootstrapped samples. Simple slopes were calculated for the 16th, 50th, and 84th percentile of the distribution, as suggested by Hayes [59]. All slopes were then plotted and tested for significance through Student t-test.
In order to assess the reliability of statistically significant results, observed effect sizes were compared with threshold reliability values calculated through sensitivity analysis [60]; f and f2 indices were employed to evaluate reliability of ANOVA and regression analyses, respectively [61].
Results
Attrition rate and data handling
A total of 721 HWs completed the longitudinal study at T1, 357 (49.5%) at T2 and 232 at T3 (32.2%). Demographic features and distress levels were compared between participants who completed all three data waves and those who dropped out after T1 or T2. Attrition analysis results indicated that there were no significant differences in age, [t(719) = 1.911; p = 0.056], gender [χ2(1) = 2.36; pFisher = 0.148], job seniority [t(719) = 1.40; p = 0.162], profession [χ2(2) = 0.23; p = 0.890], PTSS(T1) score [t(719) = -0.58; p = 0.562], or percentage of provisional PTSD diagnosis at T1 [χ2(1) = 0.07; pFisher = 0.807].
Out of the 232 participants completing the three waves, four (1.7%) were excluded from the final sample due to missing answers. Moreover, data from two participants (0.86%) were excluded from analyses because they retired from work between T2 and T3.
Descriptive statistics
The sample’s demographic and job characteristics are reported in Table 1. Most participants were women, in their forties and working as nurses or midwives; during the overall study period, over 60% of the HWs worked in a COVID-19 department.
Descriptive statistics are reported in Table 2, together with Cronbach α reliability indices and percentage of participants meeting criteria for a provisional PTSD diagnosis. All α coefficients were ≥ 0.90, indicating excellent internal consistency. As for PTSD, almost 40% of HWs received a provisional diagnosis at T1.
Cochran’ Q was employed to assess differences in the frequency of PTSD diagnosis across time; a significant difference was detected (Q(2) = 39.22; p < 0.001). Post-hoc Dunn’s tests with Bonferroni correction showed a higher percentage of PTSD diagnoses at T1 than T2 (p < 0.001), and T3 (p < 0.001); no differences were found between T2 and T3 (p = 0.82).
Since a violation of sphericity assumption was observed for repeated one-way ANOVA testing differences in PTSS scores at T1, T2, and T3 (W = 0.953; p = 0.004), robust estimation techniques based on trimmed mean (20%) and bootstrap sampling (N = 2000) were employed to corroborate results of parametric tests. Welch-James (WJ) statistic [62] was calculated and used for robust hypothesis testing.
Parametric repeated one-way ANOVA resulted in a significant omnibus test (F(2, 450) = 62.36; p < 0.001), with an effect size (f = 0.52) higher than the sensitivity threshold (f = 0.21; N = 226; 1-β = 0.80; α = 0.05). Pairwise post-hoc comparisons (Bonferroni adjustments) highlighted differences between T1 and T2 (p < 0.001), and between T1 and T3 (p < 0.001). No differences between T2 and T3 were observed for PTSS (p = 0.05). The robust alternative confirmed parametric results: The omnibus test was significant (WJ(2, 269.9) = 20.47, p < 0.001) with pairwise comparisons resulting in both a significant T1 vs T2 (WJ(2, 269.3) = 37.49; 95%CI: [0.41; 0.82]) and T1 vs T3 (WJ(2, 269.3) = 23.22; 95%CI: [0.28; 0.69]) difference; no difference was instead observed between T2 and T3 (WJ(2, 270) = 1.83; 95%CI: [− 0.34; 0.07]).
All assumptions were met for the paired Student t-test comparing BF at T2 and T3; no difference was observed between HWs’ means at these two time points (t(225) = − 0.56; p = 0.58).
Table 3 shows correlations among study measures; PTSS at T1, T2, and T3 were all positively correlated, with values > 0.60; a high positive correlation was also observed between BF at T2 and T3. All remaining correlations did not reach meaningfulness threshold.
To test the moderating effect of BF on PTSS development, a hierarchical regression analysis was employed. PTSS at T3 was considered as the criterion variable; PTSS at T1 and BF at T2 were treated as predictor and moderator, respectively, and they were inserted at step 1 together with the following control variables: participants’ gender, profession (technical and rehabilitation professionals were considered as reference category), job seniority, and being assigned to a COVID-19 department before or at T2. The cross product between PTSS at T1, and BF at T2 followed in step 2.
Plot inspection excluded violations of assumptions related to linearity and normality of residuals; Durbin-Watson (D-W = 1.89; p = 0.36) and Breusch-Pagan (BP = 9.31; p = 0.31) tests further excluded any autocorrelation or heteroscedasticity issue, respectively. While no influential data points were detected through leverages inspection, a high level of correlation (VIF values ≥ 10) was observed among variables. To reduce multicollinearity, PTSS at T1 and BF at T2 were centered at their mean values prior to creating their product term [63]. No multicollinearity issues were detected for the model with centered variables (observed VIF values < 2.5).
Results from hierarchical regression analysis are reported in Table 4.
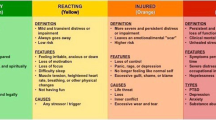
The overall model was significant (F(8,217) = 21.37; p < 0.001) and explained 44% of the variance of PTSS at T3 with an effect size f2 = 0.78 higher than sensitivity threshold (f2 = 0.068; N = 226; 1-β = 0.80; α = 0.05). A significant positive effect was observed for PTSS at T1 (p < 0.001), while no linear association was found between BF at T2 and PTSS at T3; a significant negative effect was instead identified for the product between PTSS at T1 and BF at T2 (p = 0.004). The interaction term accounted for an additional 2% of model variance, supporting the moderation hypothesis; the associated effect size to R2 increase was f2 = 0.044, higher than sensitivity threshold (f2 = 0.035; N = 226; 1-β = 0.80; α = 0.05). The interaction was probed by testing the conditional effects of PTSS(T1) at three levels of BF(T2): 16th (BF = 2.88), 50th (BF = 3.47), and 84th (BF = 4.04) percentile of the distribution [59]. A positive and significant association was detected between PTSS(T1) and PTSS(T3) for BF(T2) at 16th (t(217) = 11.22, p < 0.001; 95%CI: [0.58; 0.82]), 50th (t(217) = 11.30, p < 0.001; 95%CI: [0.47; 0.67]), and 84th (t(217) = 6.43, p < 0.001; 95%CI: [0.30; 0.58]) percentile. The moderation of BF(T2) on the relationship between PTSS at T1 and at T3 is plotted in Fig. 1; a buffering effect of BF at T2 was observed, with higher BF(T2) levels reducing the magnitude of the bivariate association between PTSS(T1) and PTSS(T3).
Discussion
The present study was aimed at investigating post-traumatic stress symptoms (PTSS) and benefit finding (BF) among health workers during the COVID-19 pandemic; the moderating role of BF on PTSS development was also inspected and longitudinally tested.
The first wave (T1) took place during the final period of the first national lockdown; not surprisingly, and in line with other studies [17, 64, 65], almost 40% of the participants reported PTSS levels meeting criteria for a provisional PTSD diagnosis. This result attests to the strain and difficulties HWs were exposed to during the pandemic outbreak. Compared to T1, a significantly lower percentage of participants met a PTSD provisional diagnosis at T2 (July–August 2020); this difference is consistent with the steadily decreasing trend of the infection rate during Summer 2020, corresponding to the T2 data collection. Subsequently, however, despite the stable rise in COVID-19 cases observed between August and October 2020 (when the third data collection took place) no significant difference emerged in PTSS values, compared to T2. Individual resources such as benefit finding, effortfully mobilized and/or built by health workers during the previous months, in order to fulfill their demanding role in the community, could have played a significant role in buffering the impact of the pandemic on HWs’ mental health. As results show, participants’ benefit finding scores did not differ between T2 and T3, similarly to what was observed for PTSS values. Considering that no clinical threshold score is available for BF, it is worth noting that HWs’ mean values at both times fell near the central point of the scale with limited standard deviation; this result suggests that most participants were able to derive positive contributions from coping with COVID-19 related difficulties, at least to some extent. The absence of a significant difference between BF values at T2 and T3 suggests that the “positive teachings” acquired from the pandemic experience had become part of the stable set of HWs’ personal resources, and thus they were not negatively impacted by the increase of contagion rates observed on October 2020.
As for the relationship between PTSS and BF, no meaningful correlations were found within and across time points. The literature addressing this topic is scarce and related findings are controversial; therefore, comparisons can be hardly made. In line with our results, the absence of a significant relationship with stress or life-threating events was observed when BF was longitudinally assessed in patients with early-stage breast cancer [47] and colorectal cancer [48]. On the contrary, a significant negative association emerged in a cross-sectional study involving two groups of patients: participants with cancer, and Systemic Lupus Erythematosus [66]. In the context of the COVID-19 pandemic, a negative association was detected between BF and stress among undergraduate students and adults, but the magnitude level was low (r = − 0.33) and the study design was cross-sectional [53]. Consistent with our findings, instead, in a longitudinal study conducted among Chinese university students from February to May 2020 [67] no meaningful associations of BF with stress and anxiety were detected.
To get a more detailed understanding of the data collected in the present study, a hierarchical regression analysis was performed to investigate the moderating effect of BF on PTSS development; results were controlled for participants’ gender, profession, job seniority, and involvement in a COVID-19 department before or at T2 (July–August 2020). BF at T2 was found to exert a significant moderating effect on the relationship between levels of PTSS experienced by HWs at T1 (coinciding with the first national lockdown) and at T3 (October 2020, characterized by a steady increase of contagion rates). More precisely, a buffering effect was observed, with higher BF levels reducing the magnitude of the bivariate association between PTSS assessed at the beginning and at the end of the study. As results showed, HWs’ PTSS measured at T3 increased with PTSS measured at T1 for low, medium and high values of BF at T2. Although significant, the strength of this relationship was reduced for HWs reporting higher scores of BF at T2 as a consequence of the significant interaction.
Overall, evidence from the present study provides support to the role of benefit finding in counterbalancing the post-traumatic stress symptoms experienced by healthcare workers during the COVID-19 pandemic. This finding bears promising implications for interventions aimed at promoting mental health among health professionals facing the COVID-19 pandemic, and other future emergency events [68, 69]. Programs aimed at reducing PTSS through cognitive behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), and well-being therapy [70, 71] could be integrated with strategies aimed at actively fostering benefit finding through the support of the related meaning-making process. As suggested by Lechner [72], however, acknowledgment of benefit finding should never be “prescribed” by clinicians or therapists, but instead facilitated through deep examination and mutual sharing. Spontaneous reports of benefits, when recognized and cultivated, can be the starting point of the meaning-making process, potentially promoting greater awareness and, ultimately, higher levels of well-being.
Considering both the high levels of PTSS, and the prevalence of provisional PTSD diagnoses observed among HWs during the COVID-19 pandemic, the support of benefit finding could be particularly useful for both the professionals who did not find any benefit in working during the pandemic, and the workers whose self-generated perception of benefits could be acknowledged and further fostered.
Limitations, strengths and future directions
To the best of our knowledge, this is the first longitudinal study jointly monitoring PTSS and BF among HWs facing the COVID-19 pandemic, with the aim of testing the effect of benefit finding on post-traumatic stress symptoms development. Taken together, findings underscored the useful role of perceiving positive contributions to one’s life in counterbalancing the negative symptoms derived from prolonged exposure to stressful experiences. Besides these novel contributions, limitations have to be acknowledged as well. First, a high attrition rate was observed along the three study waves, with the majority of participants dropping out between T1 and T2. Caution must therefore be exerted in generalizing the implications of the findings, even though it is worth noting that participants completing all waves did not differ significantly from dropped out ones for any demographic or psychological variables, and comparable dropout rates were observed in other longitudinal studies conducted during the pandemic [37]. A second limitation concerns the self-report measure employed to formulate provisional PTSD diagnoses; in future studies it should be integrated with DSM-5 based diagnosis issued by clinicians. Finally, cross-cultural differences may exist in perceived benefit while facing difficulties of the COVID-19 pandemic.
Despite limitations, results from this study can offer some hints concerning strategies that could be fruitfully implemented to foster the well-being of health workers exposed to the COVID-19 pandemic related challenges [73]. While results from the present research focused on the first months following the pandemic outbreak, future research should explore the role of benefit finding in adjusting to consequences of the pandemic evolution.
Overall, these findings could also provide some suggestions to clinicians and psychotherapists supporting helping professionals engaged in emergency or rescuing interventions.
References
Ministero della Salute. (2021) Covid-19, situation in Italy. https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=english&id=5367&area=nuovoCoronavirus&menu=vuoto. Accessed 1 May 2022
Boyraz G, Legros DN (2020) Coronavirus disease (COVID-19) and traumatic stress: probable risk factors and correlates of posttraumatic stress disorder. J Loss Trauma 25(6–7):503–522. https://doi.org/10.1080/15325024.2020.1763556
da Silva ML, Rocha RSB, Buheji M, Jahrami H, Cunha KdC (2021) A systematic review of the prevalence of anxiety symptoms during coronavirus epidemics. J Health Psychol 26(1):115–125. https://doi.org/10.1177/1359105320951620
Forte G, Favieri F, Tambelli R, Casagrande M (2020) COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int J Env Res Pub He 17(11):1–14. https://doi.org/10.3390/ijerph17114151
Gloster AT, Lamnisos D, Lubenko J, Presti G, Squatrito V, Constantinou M, Nicolaou C, Papacostas S, Gökçen A, Yuen YuC, Wai TC, Ho YuC, Ruiz FJ, Garcia-Martin MB, Obando-Posada DP, Segura-Vargas MA, Vasiliou VS, McHugh L, Höfer S, Baban A, David Dias N, Nunes da Silva A, Jean-Louis M, Alvarez-Galvez J, Paez-Blarrina M, Montesinos F, Valdivia-Salas S, Dorottya O, Kleszcz B, Lappalainen R, Ivanović I, Gosar D, Dionne F, Merwin RM, Kassianos AP, Karekla M (2020) Impact of COVID-19 pandemic on mental health: an international study. PLoS ONE 15(2):e0244809. https://doi.org/10.1371/journal.pone.0244809
Ran L, Wang W, Ai M, Kong Y, Chen J, Kuang L (2020) Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: a study of the general population in China at the peak of its epidemic. Soc Sci Med 262:1–6. https://doi.org/10.1016/j.socscimed.2020.113261
Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, Rasoulpoor S, Khaledi-Paveh B (2020) Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health 16(1):57. https://doi.org/10.1186/s12992-020-00589-w
Tarsitani L, Vassalini P, Koukopoulos A, Borrazzo C, Alessi F, Di Nicolantonio C, Serra R, Alessandri F, Ceccarelli G, Mastroianni CM, d’Ettorre G (2021) Post-traumatic stress disorder among COVID-19 survivors at 3-month follow-up after hospital discharge. J Gen Intern Med 36(6):1702–1707. https://doi.org/10.1007/s11606-021-06731-7
Carmassi C, Foghi C, Dell’Oste V, Cordone A, Bertelloni CA, Bui E, Dell’Osso L (2020) PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiat Res. 292:113312. https://doi.org/10.1016/j.psychres.2020.113312
Della Monica A, Ferrara P, Dal Mas F, Cobianchi L, Scannapieco F, Ruta F (2021) The impact of COVID-19 healthcare emergency on the psychological well-being of health professionals: a review of literature. Ann Ig 34(1):27–44. https://doi.org/10.7416/ai.2021.2445
Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, Yao L, Bai H, Cai Z, Xiang Yang B, Hu S, Zhang K, Wang G, Ma C, Liu Z (2020) Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun 87:11–17. https://doi.org/10.1016/j.bbi.2020.03.028
Moderato L, Lazzeroni D, Oppo A, Dell’Orco F, Moderato P, Presti G (2021) Acute stress response profiles in health workers facing SARS-CoV-2. Front Psychol. https://doi.org/10.3389/fpsyg.2021.660156
Mosheva M, Gross R, Hertz-Palmor N, Hasson-Ohayon I, Kaplan R, Cleper R, Kreiss Y, Gothelf D, Pessach IM (2021) The association between witnessing patient death and mental health outcomes in frontline COVID-19 healthcare workers. Depress Anx 38(4):468–479. https://doi.org/10.1002/da.23140
Bassi M, Negri L, Delle Fave A, Accardi R (2021) The relationship between post-traumatic stress and positive mental health symptoms among health workers during COVID-19 pandemic in Lombardy, Italy. J Affect Disorders 280(Pt B):1–6. https://doi.org/10.1016/j.jad.2020.11.065
d’Ettorre G, Ceccarelli G, Santinelli L, Vassalini P, Innocenti GP, Alessandri F, Koukopoulos AE, Russo A, d’Ettorre G, Tarsitani L (2021) Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review. Int J Env Res Pub Health 18(2):601. https://doi.org/10.3390/ijerph18020601
Guo W-P, Min Q, Gu W-W, Yu L, Xiao X, Yi W-B, Li H-L, Huang B, Li J-L, Dai Y-J, Xia J, Liu J, Li B, Zhou B-H, Li M, Xu H-X, Wang X-B, Shi W-Y (2021) Prevalence of mental health problems in frontline healthcare workers after the first outbreak of COVID-19 in China: a cross-sectional study. Health Qual Life Out 19(1):103. https://doi.org/10.1186/s12955-021-01743-7
Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, Rossi A (2020) Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open 3(5):e2010185. https://doi.org/10.1001/jamanetworkopen.2020.10185
Di Tella M, Romeo A, Benfante A, Castelli L (2020) Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract 26(6):1583–1587. https://doi.org/10.1111/jep.13444
World Health Organization. (2019) International classification of diseases for mortality and morbidity statistics (11th revision). https://icd.who.int/. Accessed 1 May 2022
American Psychiatric Association. (2013) Diagnostic and statistical manual of mental disorders: DSM-5, 5th edn. American Psychiatric Publishing, Washington DC
Horesh D, Brown AD (2020) Traumatic stress in the age of COVID-19: a call to close critical gaps and adapt to new realities. Psychol Trauma-Us 12(4):331. https://doi.org/10.1037/tra0000592
Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, Mason L, Martinez AP, McKay R, Stocks TVA, Bennett KM, Hyland P, Karatzias T, Bentall RP (2020) Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 6(6):e125. https://doi.org/10.1192/bjo.2020.109
Breslau N (2009) The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse 10(3):198–210. https://doi.org/10.1177/1524838009334448
Karatzias T, Hyland P, Bradley A, Cloitre M, Roberts NP, Bisson JI, Shevlin M (2019) Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: findings from a trauma-exposed population based sample of adults in the United Kingdom. Depress Anxiety 36(9):887–894. https://doi.org/10.1002/da.22934
Raker EJ, Lowe SR, Arcaya MC, Johnson ST, Rhodes J, Waters MC (2019) Twelve years later: the long-term mental health consequences of hurricane Katrina. Soc Sci Med 242:112610. https://doi.org/10.1016/j.socscimed.2019.112610
Fincham DS, Altes LK, Stein DJ, Seedat S (2009) Posttraumatic stress disorder symptoms in adolescents: risk factors versus resilience moderation. Compr Psychiatr 50(3):193–199. https://doi.org/10.1016/j.comppsych.2008.09.001
McCanlies EC, Mnatsakanova A, Andrew ME, Burchfiel CM, Violanti JM (2014) Positive psychological factors are associated with lower PTSD symptoms among police officers: post hurricane Katrina. Stress Health 30(5):405–415. https://doi.org/10.1002/smi.2615
Park CL (2010) Making sense of the meaning literature: an integrative review of meaning making and its effects on adjustment to stressful life events. Psychol Bull 136(2):257–301. https://doi.org/10.1037/a0018301
Sleijpen M, van der Aa N, Mooren T, Laban CJ, Kleber RJ (2019) The moderating role of individual resilience in refugee and Dutch adolescents after trauma. Psychol Trauma-Us 11(7):732–742. https://doi.org/10.1037/tra0000450
Tugade MM, Fredrickson BL (2004) Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol 86(2):320–333. https://doi.org/10.1037/0022-3514.86.2.320
Vázquez C, Hervás G (2010) Perceived benefits after terrorist attacks: the role of positive and negative emotions. J Posit Psychol 5(2):154–163. https://doi.org/10.1080/17439761003630060
Carver CS, Antoni MH (2004) Finding benefit in breast cancer during the year after diagnosis predicts better adjustment 5 to 8 years after diagnosis. Health Psychol 23(6):595–598. https://doi.org/10.1037/0278-6133.23.6.595
Collins RL, Taylor SE, Skokan LA (1990) A better world or a shattered vision? Changes in life perspectives following victimization. Soc Cognition 8(3):263–285. https://doi.org/10.1521/soco.1990.8.3.263
Riley K (2013) Benefit finding. In: Gellman MD, Turner JR (eds) Encyclopedia of behavioral medicine. Springer, New York, pp 208–210. https://doi.org/10.1007/978-1-4419-1005-9_628
Tennen H, Affleck G (2002) Benefit-finding and benefit-reminding. In: Snyder CR, Lopez SJ (eds) Handbook of positive psychology. Oxford University Press, Oxford, pp 584–597
Tomich PL, Helgeson VS (2004) Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychol 23(1):16–23. https://doi.org/10.1037/0278-6133.23.1.16
Miao M, Zheng L, Wen J, Jin S, Gan Y (2021) Coping with coronavirus disease 2019: relations between coping strategies, benefit finding, and well-being. Stress Health 38(1):47–56. https://doi.org/10.1002/smi.3072
Sanjuán P, García-Zamora C, Ruiz M, Rueda B, Arranz H, Castro A (2016) Benefit finding in cardiac patients: relationships with emotional well-being and resources after controlling for physical functional impairment. Span J Psychol 19:E50. https://doi.org/10.1017/sjp.2016.60
Affleck G, Tennen H (1996) Construing benefits from adversity: adaptotional significance and disposltional underpinnings. J Pers 64(4):899–922. https://doi.org/10.1111/j.1467-6494.1996.tb00948.x
Davis CG, Nolen-Hoeksema S, Larson J (1998) Making sense of loss and benefiting from the experience: two construals of meaning. J Pers Soc Psychol 75(2):561–574. https://doi.org/10.1037/0022-3514.75.2.561
Park CL, Folkman S (1997) Meaning in the context of stress and coping. Rev Gen Psychol 1(2):115–144. https://doi.org/10.1037/1089-2680.1.2.115
Tedeschi RG, Calhoun LG (2004) A clinical approach to posttraumatic growth. In: Linley PA, Joseph S (eds) Positive psychology in practice. John Wiley & Sons Inc, New York, pp 405–419
Tedeschi RG, Calhoun LG (2004) Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq 15(1):1–18. https://doi.org/10.1207/s15327965pli1501_01
Calhoun LG, Tedeschi RG (2006) The foundations of posttraumatic growth: an expanded framework. In: Calhoun LG, Tedeschi RG (eds) Handbook of posttraumatic growth: research & practice. Lawrence Erlbaum Associates Publishers, Hillsdale, pp 3–23
Tedeschi RG, Calhoun LG (1996) The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress 9(3):455–471. https://doi.org/10.1007/bf02103658
Harding S, Sanipour F, Moss T (2014) Existence of benefit finding and posttraumatic growth in people treated for head and neck cancer: a systematic review. PeerJ 2:e256–e256. https://doi.org/10.7717/peerj.256
Sears SR, Stanton AL, Danoff-Burg S (2003) The yellow brick road and the emerald city: benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychol 22(5):487–497. https://doi.org/10.1037/0278-6133.22.5.487
Zimmaro LA, Deng M, Handorf E, Fang CY, Denlinger CS, Reese JB (2021) Understanding benefit finding among patients with colorectal cancer: a longitudinal study. Support Care Cancer 29(5):2355–2362. https://doi.org/10.1007/s00520-020-05758-6
McMillen JC, Smith EM (1997) Perceived benefit and mental health after three types of disaster. J Consult Clin Psychol 65(5):733. https://doi.org/10.1037//0022-006x.65.5.733
Siegel K, Schrimshaw EW (2007) The stress moderating role of benefit finding on psychological distress and well-being among women living with HIV/AIDS. AIDS Behav 11(3):421–433. https://doi.org/10.1007/s10461-006-9186-3
Wood MD, Foran HM, Britt TW, Wright KM (2012) The impact of benefit finding and leadership on combat-related PTSD symptoms. Mil Psychol 24(6):529–541. https://doi.org/10.1080/08995605.2012.736321
Chen R, Sun C, Chen J-J, Jen H-J, Kang XL, Kao C-C, Chou K-R (2021) A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nu 30(1):102–116. https://doi.org/10.1111/inm.12796
Cox CR, Swets JA, Gully B, Xiao J, Yraguen M (2021) Death concerns, benefit-finding, and well-being during the COVID-19 pandemic. Front Psychol. https://doi.org/10.3389/fpsyg.2021.648609
Istituto Superiore di Sanità (2021a) Characteristics of SARS-CoV-2 patients dying in Italy. Report based on available data on March 1st, 2021. https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_1_march_2021.pdf. Accessed 1 May 2022
Istituto Superiore di Sanità (2021b) Epidemia COVID-19. Aggiornamento nazionale 3 marzo—ore 12:00 [The COVID-19 epidemic. National update, March 3, 12:00]. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_3-marzo-2021.pdf. Accessed 1 May 2022
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL (2015) The Posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 28(6):489–498. https://doi.org/10.1002/jts.22059
Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP (2013) The PTSD checklist for DSM-5 (PCL-5). https://www.ptsd.va.gov/. Accessed 1 May 2022
Hinkle DE, Wiersma WJ, Stephen G (2003) Applied statistics for the behavioral sciences. Houghton Mifflin, Boston
Hayes AF (2018) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach, 2nd edn. The Guildford Press, New York
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191. https://doi.org/10.3758/BF03193146
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Routledge
Villacorta PJ (2017) The welchADF package for robust hypothesis testing in unbalanced multivariate mixed models with heteroscedastic and non-normal data. R J 9(2):309–328. https://doi.org/10.32614/rj-2017-049
Aiken LS, West SG (1991) Multiple regression: Testing and interpreting interactions. Sage Publications Inc, New York
Allan SM, Bealey R, Birch J, Cushing T, Parke S, Sergi G, Bloomfield M, Meiser-Stedman R (2020) The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: a rapid systematic review and meta-analysis. Eur J Psychotraumato 11(1):1810903. https://doi.org/10.1080/20008198.2020.1810903
Zhang W, Wang K, Yin L, Zhao W, Xue Q, Peng M, Min B, Tian Q, Leng H, Du J, Chang H, Yang Y, Li W, Shangguan F, Yan T, Dong H, Han Y, Wang Y, Cosci F, Wang H (2020) Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom 89(4):242–250. https://doi.org/10.1159/000507639
Katz RC, Flasher L, Cacciapaglia H, Nelson S (2001) The psychosocial impact of cancer and lupus: a cross validation study that extends the generality of “benefit-finding” in patients with chronic disease. J Behav Med 24(6):561–571. https://doi.org/10.1023/a:1012939310459
Yang Z, Ji LJ, Yang Y, Wang Y, Zhu L, Cai H (2021) Meaning making helps cope with COVID-19: a longitudinal study. Pers Indiv Differ. 174:110670. https://doi.org/10.1016/j.paid.2021.110670
Bryson WJ (2021) Long-term health-related quality of life concerns related to the COVID-19 pandemic: a call to action. Qual Life Res 30(3):643–645. https://doi.org/10.1007/s11136-020-02677-1
Shek DTL (2021) COVID-19 and quality of life: twelve reflections. Appl Res Qual Life 16(1):1–11. https://doi.org/10.1007/s11482-020-09898-z
American Psychological Association (2017) Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. https://www.apa.org/ptsd-guideline/ptsd.pdf. Accessed 1 May 2022
Radstaak M, Hüning L, Bohlmeijer ET (2020) Well-being therapy as rehabilitation therapy for posttraumatic stress disorder symptoms: a randomized controlled trial. J Trauma Stress 33(5):813–823. https://doi.org/10.1002/jts.22500
Lechner SC (2021) Benefit-finding. In: Snyder CR, Lopez SJ, Edwards LM, Marques SC (eds) The Oxford handbook of positive psychology, 3rd edn. Oxford University Press, Oxford, pp 907–918. https://doi.org/10.1093/oxfordhb/9780199396511.013.53
Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R (2021) Monitoring the impact of COVID-19 pandemic on mental health: a public health challenge? Reflection on Italian data. Soc Psych Psych Epid 56(1):165–167. https://doi.org/10.1007/s00127-020-01971-0
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
LN: conceptualized the study aims and design and was involved in data curation, statistical analysis, preparation of the initial draft and its subsequent review and editing. MB: conceptualized the study aims and design and was involved in data collection, data curation, and in critically revising the original draft. RA: conceptualized the study aims and design and was involved in data collection, data curation, and in critically revising the original draft. ADF: conceptualized the study aims and design and was involved in project administration, data collection, data curation, and in critically revising the original draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The study protocol was in line with the Declaration of Helsinki and it was approved by the Ethical Committee of the University of Milano (n. 31/20).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Negri, L., Bassi, M., Accardi, R. et al. Post-traumatic stress symptoms and benefit finding: a longitudinal study among Italian health workers during the COVID-19 pandemic. Soc Psychiatry Psychiatr Epidemiol 58, 1549–1559 (2023). https://doi.org/10.1007/s00127-023-02475-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-023-02475-3