Abstract
Background
Some migrant and ethnic minority groups have a higher risk of coercive pathways to care; however, it is unclear whether differences in clinical presentation contribute to this risk. We sought to assess: (i) whether there were differences in clinician-rated symptoms and behaviours across first-generation immigrant and refugee groups at the first psychiatric hospitalization after psychosis diagnosis, and (ii) whether these differences accounted for disparities in involuntary admission.
Methods
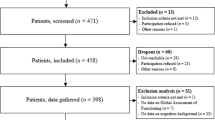
Using population-based health administrative data from Ontario, Canada, we constructed a sample (2009–2013) of incident cases of non-affective psychotic disorder followed for two years to identify first psychiatric hospitalization. We compared clinician-rated symptoms and behaviours at admission between first-generation immigrants and refugees and the general population, and adjusted for these variables to ascertain whether the elevated prevalence of involuntary admission persisted.
Results
Immigrants and refugee groups tended to have lower ratings for affective symptoms, self-harm behaviours, and substance use, as well as higher levels of medication nonadherence and poor insight. Immigrant groups were more likely to be perceived as aggressive and a risk of harm to others, and both groups were perceived as having self-care issues. Adjustment for perceived differences in clinical presentation at admission did not attenuate the higher prevalence of involuntary admission for immigrant and refugee groups.
Conclusions
First-generation migrant groups may differ in clinical presentation during the early course of psychotic illness, although these perceived differences did not explain the elevated rates of involuntary admission. Further research using outpatient samples and tools with established cross-cultural validity are warranted.


Similar content being viewed by others
Data Availability
The dataset from this study is held securely in coded form at ICES and the analyst (RR) had full access to study data. While data sharing agreements prohibit ICES from making the data set publicly available, access can be granted to those who meet pre-specified criteria for confidential access, available at https://www.ices.on.ca/DAS. The full dataset creation plan is available from the authors upon request.
References
Selten JP, van der Ven E, Termorshuizen F (2020) Migration and psychosis: a meta-analysis of incidence studies. Psychol Med 50(2):303–313. https://doi.org/10.1017/S0033291719000035
Amad A, Guardia D, Salleron J, Thomas P, Roelandt JL, Vaiva G (2013) Increased prevalence of psychotic disorders among third-generation migrants: Results from the French Mental Health in General Population survey. Schizophr Res 147(1):193–195. https://doi.org/10.1016/j.schres.2013.03.011
Waxmann A, Thompson A, McGorry P, O’Donoghue B (2022) Pathways to care for first-generation migrants with first episode psychosis in northwestern metropolitan Melbourne. Aust N Z J Psychiatry 000486742210759. https://doi.org/10.1177/00048674221075980
Anderson KK, McKenzie KJ, Kurdyak P (2017) Examining the impact of migrant status on ethnic differences in mental health service use preceding a first diagnosis of schizophrenia. Soc Psychiatry Psychiatr Epidemiol 52(8):949–961. https://doi.org/10.1007/s00127-017-1403-z
Rodrigues R, MacDougall AG, Zou G et al (2020) Risk of involuntary admission among first-generation ethnic minority groups with early psychosis: a retrospective cohort study using health administrative data. Epidemiol Psychiatr Sci 29:e59. https://doi.org/10.1017/S2045796019000556
Anderson KK, Kurdyak P (2017) Factors associated with timely physician follow-up after a first diagnosis of psychotic disorder. Can J Psychiatry 62(4):268–277. https://doi.org/10.1177/0706743716673322
Anderson KK (2018) Ethnic differences in physician follow-up after a first diagnosis of psychotic disorder. Schizophr Res 193:463–464. https://doi.org/10.1016/j.schres.2017.07.019
Nerhus M, Berg AO, Haram M, Kvitland LR, Andreassen OA, Melle I (2015) Migrant background and ethnic minority status as predictors for duration of untreated psychosis: Migration and duration of untreated psychosis. Early Interv Psychiatry 9(1):61–65. https://doi.org/10.1111/eip.12106
Boonstra N, Sterk B, Wunderink L, Sytema S, De Haan L, Wiersma D (2012) Association of treatment delay, migration and urbanicity in psychosis. Eur Psychiatr 27(7):500–505. https://doi.org/10.1016/j.eurpsy.2011.05.001
Rodrigues R, Beswick A, Anderson KK (2020) Psychiatric hospitalization following psychosis onset: a retrospective cohort study using health administrative data. Early Interv Psychiatry 14(2):235–240. https://doi.org/10.1111/eip.12893
Katsampa D, Akther SF, Hollander AC, Dal H, Dalman C, Kirkbride JB (2021) inequalities in psychiatric service use and mortality by migrant status following a first diagnosis of psychotic disorder: a Swedish cohort study of 1.3m people. Schizophrenia Bull Open 2(1):sgab009. https://doi.org/10.1093/schizbullopen/sgab009
Maguire J, Mifsud N, Seiler N et al (2021) Symptomatic, functional and service utilization outcomes of migrants with a first episode of psychosis. Soc Psychiatry Psychiatr Epidemiol 56(8):1389–1397. https://doi.org/10.1007/s00127-020-02011-7
Bosqui TJ, Hoy K, Shannon C (2014) A systematic review and meta-analysis of the ethnic density effect in psychotic disorders. Soc Psychiatry Psychiatr Epidemiol 49(4):519–529. https://doi.org/10.1007/s00127-013-0773-0
Forcada I, Pera V, Cruz I et al (2013) Comparison of immigrant and native-born population adherence to antipsychotic treatment in a Spanish health region. Community Ment Health J 49(2):199–205. https://doi.org/10.1007/s10597-012-9551-9
Ouellet-Plamondon C, Rousseau C, Nicole L, Abdel-Baki A (2015) Engaging immigrants in early psychosis treatment: a clinical challenge. Psychiatr Serv 66(7):757–759. https://doi.org/10.1176/appi.ps.201300284
Golay P, Baumann PS, Jaton L et al (2019) Migration in patients with early psychosis: a 3-year prospective follow-up study. Psychiatry Res 275:108–114. https://doi.org/10.1016/j.psychres.2019.03.021
Olbert CM, Nagendra A, Buck B (2018) Meta-analysis of Black vs. White racial disparity in schizophrenia diagnosis in the United States: Do structured assessments attenuate racial disparities? J Abnorm Psychol 127(1):104–115. https://doi.org/10.1037/abn0000309
Zandi T, Havenaar JM, Smits M et al (2010) First contact incidence of psychotic disorders among native Dutch and Moroccan immigrants in the Netherlands: Influence of diagnostic bias. Schizophr Res 119(1–3):27–33. https://doi.org/10.1016/j.schres.2010.02.1059
Zandi T, Havenaar JM, Laan W, Kahn RS, van den Brink W (2016) Effects of a culturally sensitive assessment on symptom profiles in native Dutch and Moroccan patients with a first psychosis referral. Transcult Psychiatry 53(1):45–59. https://doi.org/10.1177/1363461515577288
Adeponle AB, Thombs BD, Groleau D, Jarvis E, Kirmayer LJ (2012) Using the cultural formulation to resolve uncertainty in diagnoses of psychosis among ethnoculturally diverse patients. PS 63(2):147–153. https://doi.org/10.1176/appi.ps.201100280
Berg AO, Melle I, Rossberg JI et al (2011) Perceived discrimination is associated with severity of positive and depression/anxiety symptoms in immigrants with psychosis: a cross-sectional study. BMC Psychiatry 11(1):77. https://doi.org/10.1186/1471-244X-11-77
Perlman G, Kotov R, Fu J et al (2016) Symptoms of psychosis in schizophrenia, schizoaffective disorder, and bipolar disorder: a comparison of African Americans and Caucasians in the Genomic Psychiatry Cohort. Am J Med Genet 171(4):546–555. https://doi.org/10.1002/ajmg.b.32409
Quattrone D, Di Forti M, Gayer-Anderson C et al (2019) Transdiagnostic dimensions of psychopathology at first episode psychosis: findings from the multinational EU-GEI study. Psychol Med 49(08):1378–1391. https://doi.org/10.1017/S0033291718002131
Benchimol EI, Smeeth L, Guttmann A et al (2015) The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med 12(10):e1001885. https://doi.org/10.1371/journal.pmed.1001885
Kurdyak P, Lin E, Green D, Vigod S (2015) Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry 60(8):362–368. https://doi.org/10.1177/070674371506000805
Statistics Canada (2010) Standard classification of countries and areas of interest. Accessed August 11, 2021. https://www.statcan.gc.ca/eng/subjects/standard/sccai/2010/sccai
Hirdes JP, Smith TF, Rabinowitz T et al (2002) The resident assessment instrument-mental health (RAI-MH): inter-rater reliability and convergent validity. J Behav Health Serv Res 29(4):419–432. https://doi.org/10.1007/BF02287348
Martin L, Hirdes JP, Morris JN, Montague P, Rabinowitz T, Fries BE (2009) Validating the mental health assessment protocols (MHAPs) in the resident assessment instrument mental health (RAI-MH). J Psychiatr Ment Health Nurs 16(7):646–653. https://doi.org/10.1111/j.1365-2850.2009.01429.x
Hirdes JP, Ljunggren G, Morris JN et al (2008) Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res 8(1):277. https://doi.org/10.1186/1472-6963-8-277
Burrows A (2000) Development of a minimum data set-based depression rating scale for use in nursing homes. Age Ageing 29(2):165–172. https://doi.org/10.1093/ageing/29.2.165
Perlman CM, Hirdes JP (2008) The aggressive behavior scale: a new scale to measure aggression based on the minimum data set: the MDS-aggressive behavior scale. J Am Geriatr Soc 56(12):2298–2303. https://doi.org/10.1111/j.1532-5415.2008.02048.x
Neufeld E, Perlman CM, Hirdes JP (2012) Predicting inpatient aggression using the InterRAI risk of harm to others clinical assessment protocol: a tool for risk assessment and care planning. J Behav Health Serv Res 39(4):472–480. https://doi.org/10.1007/s11414-011-9271-x
Chiu M, Lebenbaum M, Newman AM, Zaheer J, Kurdyak P (2016) Ethnic differences in mental illness severity: A population-based study of Chinese and South Asian patients in Ontario. Can J Clin Psychiatry 77(09):e1108–e1116. https://doi.org/10.4088/JCP.15m10086
Mah TM, Hirdes JP, Heckman G, Stolee P (2015) Use of control interventions in adult in-patient mental health services. Healthc Manage Forum 28(4):139–145. https://doi.org/10.1177/0840470415581230
Steele LS, Glazier RH, Lin E, Evans M (2004) Using administrative data to measure ambulatory mental health service provision in primary care. Med Care 42(10):960–965
Austin PC (2009) Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 38(6):1228–1234. https://doi.org/10.1080/03610910902859574
Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159(7):702–706. https://doi.org/10.1093/aje/kwh090
Zou G, Donner A (2013) Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res 22(6):661–670. https://doi.org/10.1177/0962280211427759
Lloyd K, Moodley P (1992) Psychotropic medication and ethnicity: an inpatient survey. Soc Psychiatry Psychiatr Epidemiol 27(2):95–101. https://doi.org/10.1007/BF00788512
Morgan C, Mallett R, Hutchinson G et al (2005) Pathways to care and ethnicity. 1: Sample characteristics and compulsory admission: Report from the ÆSOP study. Br J Psychiatry 186(4):281–289. https://doi.org/10.1192/bjp.186.4.281
Mulder CL, Koopmans GT, Selten JP (2006) Emergency psychiatry, compulsory admissions and clinical presentation among immigrants to the Netherlands. Br J Psychiatry 188(4):386–391. https://doi.org/10.1192/bjp.188.4.386
Barnett P, Mackay E, Matthews H et al (2019) Ethnic variations in compulsory detention under the Mental Health Act: a systematic review and meta-analysis of international data. The Lancet Psychiatry 6(4):305–317. https://doi.org/10.1016/S2215-0366(19)30027-6
Morgan C, Mallett R, Hutchinson G, Leff J (2004) Negative pathways to psychiatric care and ethnicity: the bridge between social science and psychiatry. Soc Sci Med 58(4):739–752. https://doi.org/10.1016/S0277-9536(03)00233-8
Anderson KK, Cheng J, Susser E, McKenzie KJ, Kurdyak P (2015) Incidence of psychotic disorders among first-generation immigrants and refugees in Ontario. CMAJ 187(9):E279–E286. https://doi.org/10.1503/cmaj.141420
Anderson KK, Flora N, Ferrari M et al (2015) Pathways to first-episode care for psychosis in African-, Caribbean-, and European-origin groups in Ontario. Can J Psychiatry 60(5):223–231. https://doi.org/10.1177/070674371506000504
Stouten LH, Veling W, Laan W, Van der Gaag M (2019) Psychopathology, cognition and outcome in Dutch and immigrant first-episode psychosis patients. Early Interv Psychiatry 13(3):646–656. https://doi.org/10.1111/eip.12561
Veling W, Selten JP, Mackenbach JP, Hoek HW (2007) Symptoms at first contact for psychotic disorder: Comparison between native Dutch and ethnic minorities. Schizophr Res 95(1–3):30–38. https://doi.org/10.1016/j.schres.2007.06.024
Berg AO, Andreassen OA, Aminoff SR, Romm KL, Hauff E, Melle I (2014) The impact of immigration and visible minority status on psychosis symptom profile. Soc Psychiatry Psychiatr Epidemiol 49(11):1747–1757. https://doi.org/10.1007/s00127-014-0897-x
Tortelli A, Nakamura A, Suprani F et al (2018) Subclinical psychosis in adult migrants and ethnic minorities: systematic review and meta-analysis. BJPsych Open 4(6):510–518. https://doi.org/10.1192/bjo.2018.68
Senior PA, Bhopal R (1994) Ethnicity as a variable in epidemiological research. BMJ 309(6950):327–330. https://doi.org/10.1136/bmj.309.6950.327
Acknowledgements
Kelly Anderson is supported by a Canada Research Chair in Public Mental Health Research. This study was funded by a New Investigator Fellowship from the Ontario Mental Health Association (KKA). This study was conducted at ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). Parts of this material are based on data and information compiled and provided by the MOH and the Canadian Institute for Health Information (CIHI). The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. Parts or whole of this material is based on data and/or information compiled and provided by Immigration, Refugees and Citizenship Canada (IRCC). However, the analyses, conclusions, opinions, and statements expressed in the material are those of the author(s), and not necessarily those of IRCC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anderson, K.K., Rodrigues, R. Differences in clinical presentation at first hospitalization and the impact on involuntary admissions among first-generation migrant groups with non-affective psychotic disorders. Soc Psychiatry Psychiatr Epidemiol 58, 1329–1341 (2023). https://doi.org/10.1007/s00127-023-02465-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-023-02465-5