Abstract
Purpose
Mental health conditions may affect outcome of COVID-19 disease, while exposure to stressors during the pandemic may impact mental health. The purpose of this study was to examine these factors in relation to ocurrence of depression and anxiety after the first outbreak in Spain.
Methods
We contacted 9515 participants from a population-based cohort study in Catalonia between May and October 2020. We drew blood samples to establish infection to the virus. Pre-pandemic mental health conditions were confirmed through Electronic Health Registries. We used the Hospital Anxiety and Depression Scale to assess severe depression and anxiety post-pandemic. Exposure to proximal, financial and wider environment stressors during the lockdown were collected. We calculated Relative Risks (RR), adjusting for individual- and contextual covariates.
Results
Pre-pandemic mental health disorders were not associated with SARS-CoV-2 infection , but were associated with severity of COVID-19 disease. People with pre-existing mental health disorders showed higher prevalence of severe depression (25.4%) and anxiety (37.8%) than those without prior mental disorders (4.9% and 10.1%). Living alone was a strong predictor of severe depression among mental health patients (RR = 1.6, 95% CI 1.2–2.2). Among those without prior mental health disorders, post-lockdown depression and anxiety were associated with household interpersonal conflicts (RR = 2.6, 95% CI 2.1–3.1; RR = 2.1, 95% CI 1.9–2.4) and financial instability (RR = 2.2, 95% CI 1.8–2.9; 1.9, 95% CI 1.6–2.2).
Conclusions
The COVID-19 pandemic and the lockdown were associated with increased post-lockdown depression and anxiety. Patients with pre-existing mental health conditions are a vulnerable group for severe COVID-19 disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
From the beginning of the coronavirus disease 2019 (COVID-19) pandemic, higher rates of severe depression and anxiety were expected in association with the outbreak itself (e.g. fear of getting infected) and with stressors originating from the disruptions in living and socioeconomic conditions following the stay-at-home orders [1, 2]. These expectations were promoted by previous evidence on vulnerable groups showing that enforced isolation, household interpersonal conflicts, job insecurity, and environmental hazards are stressors associated with clinically relevant depression and anxiety [3,4,5]. After the outbreak of the COVID-19 disease, population-based studies provided initial confirmation to these associations [6].
The effects of potential stressors in different population groups are still unclear. A key component to understand these relationships are inequalities that can potentially shape the rates of the disorders and the risks associated with each of the stressors. For example, women survivors of domestic violence have a two-time increased risk of depression and anxiety [7], but the impact of this exposure may be different in the context of the confinement during the pandemic. Similarly, stressors such as isolation may have been particularly hard in some age groups, potentially modifying the age-dependent rates of depression and anxiety. Therefore, the examination of the effects of the pandemic response measures on mental health requires disaggregating the results according to these factors that may underlie an unequal distribution of susceptibility [8].
Patients with prior mental health conditions have been found to be more prone to COVID-19 disease [9]. They may have a reduced awareness of risk that can lead to increased exposure to hazards and more barriers in accessing adequate treatment [10]. Pathophysiological features involving the hypothalamic–pituitary–adrenal (HPA) axis, autonomic nervous system and immunological response may increase the patients’ neurobiological vulnerability to the disease [11, 12]. Recent analyses have identified gene clusters and inflammatory signalling pathways shared between COVID-19 and mental disorders that suggest common pathogenic mechanisms [13, 14]. In turn, people with pre-existing depression and anxiety were expected to present a worsening of their mental health status after the first outbreak of the COVID-19 pandemic. Being a vulnerable group, they may be differentially affected by risk factors such as unemployment, isolation, and other stressors that were frequent in the context of the confinement [15].
Spain was among the hardest-hit countries in Europe during the first months of the outbreak reaching almost 10,000 cases and over 1000 deaths per day in early April 2020. This led to firm restrictions in a society strongly defined by family ties and outdoor life, and an economy largely dependent on tourism and restaurant business. A stay-at home order was issued at the national level starting March 15th and lasted until April 26th. Official registers showed a 21% increase in the rates of unemployment in May 2020 relative to May 2019 [16]. Calls to emergency numbers reporting domestic violence increased by 80% in May 2020 relative to February 2020 [17].
In the present study, we examined in a large population-based cohort in northern Spain (Catalonia) the association of pre-pandemic mental conditions with infection to SARS-CoV-2 and severity of COVID-19 disease. We describe the prevalence of severe depression and anxiety following the first wave of the COVID-19 pandemic and explore the association between proximal, financial and wider environment stressors during the lockdown with the prevalence of depression and anxiety, disaggregated by previous history of mental health diagnoses. We finally examine these factors across vulnerable groups defined by age, gender, and socioeconomic status (SES).
Methods
Study design and participants
The COVICAT Study (COVID-19 cohort in Catalonia) is a prospective epidemiological study that aims to describe the health impact of the COVID-19 pandemic on the adult population in northern Spain. It builds on pre-existing cohort studies that were established before the outbreak. A single harmonized protocol was used for all five cohorts included in the COVICAT study that comprised all living cohort participants with an email address or telephone number. 88.5% of the COVICAT study where participants of a single cohort (GCAT) [18]. The description of the individual cohort studies, references, and inclusion criteria are described in Supplementary materials pp.2–3. After the first wave of the COVID-19 pandemic in Spain in March 2020, we harmonized data of all cohorts and participants were contacted. They responded to a questionnaire and draw blood samples to determine SARS-CoV-2 seroprevalence. Data collection was primarily completed on a study portal website, while we conducted telephone interviews for participants unfamiliar with web-based approaches (n = 577, 6.1%). All participants provided informed consent, and we obtained ethical approval for the study from the Parc de Salut Mar Ethics Committee (CEIm-PS MAR, number 2020/9307/I).
We contacted most participants in our study (99.7%) between May 28th and August 15th, 2020, coincident with the progression towards the “new normality.” This phase was characterized by increased mobility, opening of commercial activities at 50% space capacity, and priority times for outings of vulnerable groups. These restrictions were progressively reduced until the new normality was reached in mid-June. Out of the eligible participants who were contacted 10,862 (61.5%) agreed to participate; of these, 10,087 (92.9%) participants completed the interview satisfactorily. In the present report, we excluded 34 participants who were interviewed in autumn (between October and November, 2020), when new restrictions were applied. Pre-pandemic information of diagnosis of mental health disorder could not be confirmed through Electronic Health Records in 538 participants, and these cases were excluded from the analysis. Complete records were available for 9515 participants.
Measures
The study primary outcomes were severe depression and anxiety experienced by the participants at the time of data collection. These outcomes were assessed using the Hospital Anxiety and Depression Scale (HADS) [19], which provided a measure of ongoing symptoms of anxiety and depression through 14 items scored on a four-point Likert-type scale. The HADS can be used for diagnostic purposes and for assessing the severity of the disorders through the Depression and Anxiety subscales. Each subscale counts 7 items and ranges between 0 and 21. Following the cut-off points validated in the Spanish population [20], we used a score of 11 for each subscale to identify both severe anxiety and severe depression, while moderate levels of anxiety were settled at 8 and moderate levels of depression at 6. Severe anxiety and depression levels indicate clinically relevant diagnosis [21]).
Participants were asked whether they had ever been diagnosed by a doctor with depression, anxiety or other mental health illness. Lifetime self-reported diagnoses were confirmed through Electronic Health Records of the Public Healthcare System linked to each participant through the Health Personal Identification Number. This system provides detailed data on mental health diagnoses according to the International Classification of Diseases, 9th revision, registered by healthcare professionals in clinical settings since 2012.
We identified the stressors of interest during confinement (March 15th to April 26th, 2020) among factors previously proposed to have a disrupting effect [1] and conceptualized them as (1) proximal, (2) financial, (3) wider environment factors according to the established ecological systems theory [22] and the social determinants of mental health model [5]. We also evaluated COVID-19 disease as a potential stressor:
-
(1)
Proximal factors.
-
1.1
The number of people living in the household during the confinement was used as an indicator of isolation. Living alone, in contrast to sharing the household with 1 or more people, was considered of risk for depression/anxiety.
-
1.2
Media exposure during the confinement was examined through the frequency of use of media to check information about the pandemic, ranked several times a day, daily, weekly or more. Consulting information several times a day was considered high media exposure.
-
1.3
Data on interpersonal conflicts in the household during the confinement were collected by asking participants to state indicate the degree of agreement with a statement that they had difficulties to cope with lockdown due to conflicts with other household members. A complete or partial agreement was considered of risk.
-
1.4
Caregiving activities during the confinement were explored by asking participants whether they were in charge of caregiving for children in contrast to their partner, a third party or shared responsibilities within the adults in the household. Being in charge of caregiving activities was considered of risk.
-
1.1
-
(2)
Financial factors.
-
2.1
Concerns regarding financial instability were explored through the question: “As a consequence of the lockdown, are you in a situation where you cannot face common expenses such as rent or food?”. A positive response was considered of risk and captured as “Struggle to pay rent/food”.
-
2.2
Employment status at the time of assessment was collected and unemployment during the lockdown was analysed compared to the rest of status (employed, others including retired, student, and household work).
-
2.1
-
(3)
Wider environment factors.
-
3.1
Access to outdoor facilities during confinement was explored by rating the availability and frequency of use of any balcony, terrace or garden in this period, and dichotomizing the answers to code for frequent/very frequent access versus rare/no access (risk).
-
3.2
Participants had to rate how much they were annoyed by noise coming from outside their homes (traffic, essential commercial and industrial, neighbours) during confinement using a 11-point Likert scale. This variable was dichotomized as no/low annoyance (score 0–5) versus moderate/high annoyance (score 6–10 indicating risk).
-
3.1
-
(4)
COVID-19.
Participants were asked about a positive test for SARS-CoV-2 infection, COVID-19 hospitalization, presence of COVID-19 symptoms or contact with diagnosed COVID-19 case. Based on this information, we defined 469 cases of COVID-19 [23]. Severe COVID cases were those reporting COVID-19 hospital or Intensive Care Unit (ICU) admission (n = 59) verified through electronic records.
The survey’s digitalized format forced the users to respond to all items of the scales before submitting, which prevented missing items as well as missing HADS scores. Two predictors used in this study (media exposure and access to outdoor spaces) were omitted in the telephone survey due to the length of the interview and those participants are not included in analyses of these variables. The total number of participants for each analysis is reported in the table footnotes.
All participants were invited to participate in the serological study and 8906 agreed. We collected blood samples from 4103 participants randomly selected from those agreeing to participate. The assay used measured levels of IgM, IgA and IgG to five SARS-CoV-2 antigens and defined seropositivity using pre-pandemic control samples. Assay performance has been described elsewhere [24]. We detected SARS-CoV-2 antibodies in 70% of self-reported cases and in 90% of participants reporting prior COVID-19 hospital admission. [23].
Data on age, gender and educational level were collected. Educational level was used as a proxy for socioeconomic status: higher education level (graduate or above) indexed higher socioeconomic status. Number of days passed from end of stay-at-home order to the interview date was recorded and explored to control for potential differences in emotional states related to the different phases of the deconfinement process.
Statistical analysis
We applied log-binomial regression models to estimate Relative Risks (RR) and 95% CIs for the association between the stressors and the outcomes, adjusted for age, gender, education level, days passed from end of stay-at-home order to the interview date, type of interview (online/telephone), pre-pandemic diagnosis of mental health (MH) disorder and (when appropriate) COVID-19 disease. When convergence was not achieved, we applied Poisson regression models with robust standard errors. We examined potential differences in the associations across vulnerable groups. Effect modification by gender, age, SES and pre-pandemic diagnosis of mental health disorder was assessed by including the interaction term in the models. Relative Risks for each stratum were derived from the interaction model. We also applied log-binomial regression to estimate Relative Risks (RR) and 95% CIs for models evaluating COVID-19 outcomes (SAR-CoV-2 infection, COVID-19 and severity). All statistical analyses were performed using Stata S.E. version 16 (StataCorp LLC, Texas, USA).
To extrapolate the prevalence of severe depression and anxiety to the overall population, we calibrated study data to generate estimates representing the population of the region aged more than 20 years from the 2019 national census (INE 2019), including age, sex, education, smoking, and health region. We calculated sampling weights using iterative proportional fitting or "raking" [25] to balance the study sample characteristics to those of the population. The COVICAT study includes lower numbers of younger ages (less than 40), which leads to overdispersed weights. For this reason, we restricted extreme weights by trimming the distribution at 99% of the weights.
Results
The mean age of the participants was 54.6 years old (age range 20–72) with a slightly higher proportion of women and 46% with education level graduate or above (Table 1). The mean number of days passed between the end of the stay-at-home order and the date of the interview was 45.8 days. Almost 5% of the sample had a diagnosis of COVID-19 disease (N = 469). Table 1 shows the frequencies of confirmed pre-pandemic depression (n = 225; diagnosis of major depressive disorder = 87 cases, dysthymia = 155 cases) and anxiety (n = 267; diagnosis of anxiety disorder = 248 cases, phobias = 20 cases, obsessive–compulsive disorder = 17 cases). Other diagnoses were: bipolar disorder Type I (21 cases), schizophrenia (8 cases), and eating disorders (19 cases). Participants with pre-pandemic diagnosis of mental health disorder were more frequently women (70.7%) in their 50’s (51.9%) and presented a secondary-level education (46.2%).
Pre-pandemic mental health diagnosis, SARS-CoV-2 infection and COVID-19
We examined whether the risk of SARS-CoV-2 infection (measured through antibody levels), COVID-19 disease and severity of the disease were associated with having pre-pandemic diagnosed mental health conditions compared to those not diagnosed with these conditions (Table 2). The risk of SARS-CoV-2 infection was explored among participants with serological testing (N = 3879). There was no evidence of association between prior mental health diagnosis and infection (RR = 1.17, 95% CI = 0.89–1.54 for any prior disease). Compared to participants with no prior mental health diagnosis, patients had an increased risk of COVID-19 disease (RR = 1.64, 95% CI = 1.22–2.21 for any prior mental health diagnosis). Risk was higher for those with severe COVID-19 (hospitalized or ICU) (RR = 3.60, 95% CI = 1.83–7.10). Patients diagnosed with depression tended to have higher risks than those diagnosed with anxiety (Table 2).
Post-lockdown prevalence of anxiety and depression
The prevalence of severe depression at the COVICAT study after the outbreak (measured with HADS) was 5.9% and of severe anxiety 11.8% (Table 3). Prevalence was higher among participants with any pre-pandemic mental health disorders (25.4% for severe depression and 37.8% for severe anxiety) compared to those without pre-pandemic diagnosis (4.9% severe depression, 10.1% severe anxiety). Women, people under the age of 50, and those in low-and middle-SES, showed higher prevalence than men, those aged 50 and above and those in high SES (Table 3).
We extrapolated these estimates to the total adult population of Catalonia, using weights calculated based on sex, age, education and area of Catalonia distribution in the adult population. The post-pandemic prevalence in the total adult population of Catalonia was estimated to be 5.0% (n = 305,207) for severe depression and 10.7% for severe anxiety (n = 653,229 cases).
Stressors during lockdown, anxiety and depression
We explored the association between stressors during lockdown and severity of post-lockdown depression and anxiety (Table 4). All stressors (with the exception of living alone for severe anxiety) were associated with severe depression and severe anxiety. The highest RR were observed for household interpersonal conflicts in relation to severe depression (RR = 2.22, 95% CI = 1.90–2-59) and severe anxiety (RR = 1.97, 95% CI = 1.77–2.19). There was also a strong effect of financial factors, specifically struggle to pay for rent/food (RR = 2.05, 95% CI = 1.70–2.47 for severe depression; RR = 1.77, 95% CI = 1.55–2.01 for severe anxiety) and also for unemployment in relation to severe depression (RR = 1.81, 95% CI = 1.49–2.20). Having been diagnosed with COVID-19 disease was associated with both severe depression and severe anxiety (Table 4).
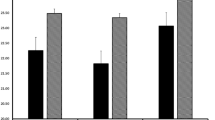
When stratifying by pre-pandemic diagnosis of mental health disorders, patterns of risk of severe depression and anxiety in relation to stressors tended to be lower among those with prior mental health disorders as compared to risks found among persons without prior mental health disorders (Fig. 1). The only exception was the association between living alone and severe depression and anxiety, which was higher in the group of mental health patients (Fig. 1 and Supplementary Table S1 for numerical estimates).
Associations between exposures and severe depression (a) and anxiety (b) by pre-pandemic diagnosis of mental health (MH) disorder from log-binomial/Poisson regressions. Dots indicate estimates of relative risks and bars represent 95% CI. Analyses were adjusted for gender, age, education level, days passed since end of stay-at-home order, COVID-19 diagnosis, and type of interview
The impact of unemployment and struggle to pay for rent/food was larger among men, in particular for anxiety (interaction p < 0.01). Women showed higher increases in RR of depression in association with noise annoyance (interaction p < 0.05). The widest difference by age was found for noise annoyance with a higher RR of anxiety among persons above 60 (interaction p < 0.05). Finally, caregiving of children was associated with higher RR of anxiety in high SES group compared to low/middle SES group (interaction p < 0.05) (Fig. 2 and Supplementary Tables S2-S4).
Discussion
Using a large population-based cohort of adult participants in northern Spain, we found that diagnosed pre-pandemic mental health disorders were associated with a higher risk of severe COVID-19 disease although not for a higher risk of infection by SARS-CoV-2. 5.7% of people presented severe depression and 11.5% severe anxiety after the first wave of the COVID-19 pandemic and the prevalence was four- to five-times higher among those with confirmed history of mental health diagnosis. Post-lockdown increased risks of anxiety and depression were associated with proximal, financial and environmental stressors experienced during the lockdown and with COVID-19 disease, and were dependent upon pre-pandemic social, economic and health inequalities.
The finding that patients with previous history of mental health treatment presented high prevalence of depression and anxiety during the lockdown has been proposed in studies using self-reported measures as perceived by the patients [26, 27], case–control reports measuring symptoms through scales [28] and longitudinal population-based studies [15]. However, the mechanisms underlying this increased risk of severe symptomatology are not fully understood. We found that the associations between the increases in prevalence of depression and anxiety and the stressors were in general weaker among patients when compared to the group of participants without pre-existing mental illness. The only exception was living alone, which was associated with a RR = 1.59 among these patients (95% CI = 1.17–2.15). This finding supports a role for forced physical distancing as a potential detrimental influence among patients with a history of mental health diagnosis. The emotional state of loneliness has been found to predict mental health conditions [29], and it could be the case that those living alone may experience this emotional state more frequently and/or more severely than those sharing the household. Other factors not included in our study, such as disruption of healthcare and reduced access to medication, may have had a large influence in the mental state of people requiring treatment as was the case for other patients with chronic disorders [30,31,32]. Further research is needed in longitudinal follow-ups of patients using pre-pandemic mental health registries and treatment disruptions.
We found that patients with prior mental health conditions were more frequently affected by COVID-19 disease, and the presentation of the disease was more severe. In turn, having a diagnosis of COVID-19 was associated with increased risk of presenting depression and anxiety during the confinement. This bi-directional relationship between mental health and COVID-19 is supported by most, although not all, cohort studies based on pre-pandemic records [33,34,35] and reports of patients with long-COVID [36]. Potential explanations include psychosocial characteristics involving behavioral and lifestyle patterns along with a high symptoms awareness and close access to the health system that could have facilitated the diagnosis. Importantly, shared biological mechanisms affecting brain areas implicated in mood regulation or related to psychopharmacological treatment may explain the findings. We did not find evidence for higher seropositivity in the group of patients, indicating that previous mental health conditions do not increase susceptibility to infection with SARS-CoV-2. Among those infected, however, prior mental health conditions did predispose to more severe COVID-19 disease. Most reports focusing on people with previous mental disorders did not include information on antibodies levels. Interestingly, a study exploring severe mental disorders (i.e. schizophrenia, bipolar disorder) found that risk of SARS-CoV-2 seropositivity was lower in patients [37]. Altered neuroendocrine regulation and associated interactions with the immune system are key features of depression and anxiety. COVID-19 disease impacts similar pathways and shows significant genetic correlations with mental disorders [38]. Increased severity of COVID-19 among people with pre-pandemic mental conditions may be therefore better explained by common molecular mechanisms acting at the central level. We have observed that some of the candidate genes of the 17q21.31 inversion locus associated with severity show a strong expression enrichment in the neural system [39]. For example, protein coding genes including ARL17B, STH, KANSL1, LRRC37A2, MAPT, NSF, PLEKHM1 and CRHR1 show high expression in brain tissues and pituitary gland. A combined effect of previous conditions and COVID-19 disease may trigger autoimmune and inflammatory processes leading to an exaggerated symptoms progression [13]. While further research is warrant, it is evident that people living with a mental health condition are a vulnerable group that require a special consideration during health emergencies such as the COVID-19 pandemic.
When considering the general population, household interpersonal conflicts were among the strongest factors associated with depression and anxiety after the first outbreak. This effect may have been accentuated by the prolonged lockdown measures, as suggested by the 27.8% of participants reporting difficulties in interpersonal relationships at home during confinement. Interpersonal conflicts include a wide range of behaviors and describe interpersonal dynamics that repeat over time. It is possible that a frequent exposure to these stressful situations underlies the increased risk of depression and anxiety [40, 41]. Financial stressors also showed a relevant association with increased severe depression and anxiety not only among people in low/middle SES but also among those from higher income contexts. Unemployment and inability to pay the bills are a well-acknowledged risk factor for poor mental health that in the context of the pandemic has hit the society as a whole, creating new vulnerabilities and further deepening pre-existing inequalities [6, 42].
Lack of access to outdoor spaces was a main concern during the confinement, because it had previously been linked to changes at the level of the stress response system through direct modulation of affective states, or indirectly through social cohesion and physical activity [43]. Our results support these concerns, and add evidence towards the role of noise as a relevant environmental predictor of both depression and anxiety. We explored this association using a measure of noise annoyance that indicates the subjective emotion related to the experience of noise. This result may in part reflect the fact that noise coming from outside the homes was inescapable during confinement, which could have accentuated the experience of stress [44, 45].
This study has several strengths, including the cohort and population-based design, and sample size. Limitations include the modest response rate mostly due to errors in contact information and an overrepresentation of people with an education level of college degree or higher, as well as aged 45 and above. The prevalence of pre-pandemic diagnosis of mental health disorder was at the lower end of the range expected in the general population according to Spanish registries [46]. This does not affect the validity of the findings but may affect generalizability. The prevalence of severe depression and anxiety in our study are similar to those reported by initial population-based surveys in other settings [15, 47, 48], although the direct comparison between studies should be done cautiously given the methodological differences across them (diagnosis definition and assessment, selection of participants, period of data collection). Our data do not cover young people, who are a particularly vulnerable group and showed a high increase in prevalence of depression and anxiety after the first outbreak [49]. However, people over 40 was the age group with the highest prevalence before the outbreak, and followed younger groups in post-outbreak increased prevalence [50]. The availability of population surveys in the region with detailed information on lifestyle, residence, social class, health conditions and health-related behaviors allowed us to control for differences between our study population and the general population of the wider region and model population prevalence. Finally, the number of participants with COVID-19 disease was small, which could be a limitation of our study. However, the prevalence of COVID-19 in our sample was comparable with that of the underlying population at the time of assessment [51].
In conclusion, we found an increase in prevalence of severe depression and anxiety in relation to the COVID-19 pandemic and subsequent lockdown. Our results raise awareness on the impact of interpersonal conflicts and financial burden on mental wellbeing and highlight the need to address wider environment and societal factors in the management of the emergency. The variation in risk observed among people with pre-pandemic mental health conditions suggest different underlying mechanisms that require tailored interventions.
Data sharing
The COVICAT study deidentified participant data and data dictionary will be made available upon request to the corresponding author after approval of a proposal and signed data access agreement.
References
Holmes EA, O’Connor RC, Perry VH et al (2020) Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7:547–560. https://doi.org/10.1016/S2215-0366(20)30168-1
Simon N, Saxe G, Marmar CR (2020) Mental health disorders related to COVID-19 – related deaths. JAMA 324:1493–1494. https://doi.org/10.1001/jama.2020.19632
Kessler RC, Bromet EJ (2013) The epidemiology of depression across cultures. Annu Rev Public Health 34:119. https://doi.org/10.1146/ANNUREV-PUBLHEALTH-031912-114409
Bandelow B, Michaelis S (2015) Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci 17:327. https://doi.org/10.31887/DCNS.2015.17.3/BBANDELOW
Allen J, Balfour R, Bell R, Marmot M (2014) Social determinants of mental health. Int Rev Psychiatry 26:392–407. https://doi.org/10.3109/09540261.2014.928270
Chandola T, Kumari M, Booker CL, Benzeval MJ (2020) The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol Med 7:1–10. https://doi.org/10.1017/S0033291720005048
Kuehner C (2017) Why is depression more common among women than among men? Lancet Psychiatry 4:146–158
Fitzpatrick KM, Harris C, Drawve G (2020) Living in the midst of fear: depressive symptomatology among US adults during the COVID-19 pandemic. Depress Anxiety. https://doi.org/10.1002/da.23080
Liu L, Ni S-Y, Yan W et al (2021) Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: a systematic review, meta-analysis and call for action. EClinicalMedicine 40:101111. https://doi.org/10.1016/J.ECLINM.2021.101111
Yao H, Chen JH, Xu YF (2020) Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 7:e21. https://doi.org/10.1016/S2215-0366(20)30090-0
Otte C, Gold SM, Penninx BW et al (2016) Major depressive disorder. Nat Rev Dis Prim 2:44
Craske MG, Stein MB, Eley TC et al (2017) Anxiety disorders. Nat Rev Dis Prim 3:1–18. https://doi.org/10.1038/nrdp.2017.24
Moni MA, Lin P-I, Quinn JMW, Eapen V (2021) COVID-19 patient transcriptomic and genomic profiling reveals comorbidity interactions with psychiatric disorders. Transl Psychiatry 11:160. https://doi.org/10.1038/s41398-020-01151-3
Xia J, Chen S, Li Y et al (2022) Immune response is key to genetic mechanisms of SARS-CoV-2 infection with psychiatric disorders based on differential gene expression pattern analysis. Front Immunol. https://doi.org/10.3389/FIMMU.2022.798538/FULL
Fancourt D, Steptoe A, Bu F (2021) Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8:141–149. https://doi.org/10.1016/S2215-0366(20)30482-X
Ministerio de Trabajo y Economía Social (2020) Evolución del paro registrado, Madrid
Ministerio de Igualdad (2020) Boletín Estadístico Mensual, Madrid
Obón-Santacana M, Vilardell M, Carreras A et al (2018) GCAT|Genomes for life: a prospective cohort study of the genomes of Catalonia. BMJ Open. https://doi.org/10.1136/bmjopen-2017-018324
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Carmen Terol-Cantero M, Cabrera-Perona V, Martín-Aragón M (2015) Revisión de estudios de la Escala de Ansiedad y Depresión Hospitalaria (HAD) en muestras españolas. An Psicol. https://doi.org/10.6018/analesps.31.2.172701
Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the hospital anxiety and depression scale: an updated literature review. J Psychosom Res 52:69–77. https://doi.org/10.1016/S0022-3999(01)00296-3
Bronfenbrenner U, Ceci SJ (1994) Nature-nurture reconceptualized in developmental perspective: a bioecological model. Psychol Rev 101:568–586
Karachaliou M, Moncunill G, Espinosa A et al (2021) Infection induced SARS-CoV-2 seroprevalence and heterogeneity of antibody responses in a general population cohort study in Catalonia Spain. Sci Rep 11:21571. https://doi.org/10.1038/S41598-021-00807-4
Dobaño C, Vidal M, Santano R et al (2021) Highly sensitive and specific multiplex antibody assays to quantify immunoglobulins M, A, and G against SARS-CoV-2 antigens. J Clin Microbiol. https://doi.org/10.1128/JCM.01731-20
Dal Grande E, Chittleborough CR, Campostrini S et al (2015) Health estimates using survey raked-weighting techniques in an Australian population health surveillance system. Am J Epidemiol 182:544–556. https://doi.org/10.1093/aje/kwv080
Gobbi S, Płomecka M, Ashraf Z et al (2020) Worsening of preexisting psychiatric conditions during the COVID-19 pandemic. Front Psychiatry 11:581426. https://doi.org/10.3389/fpsyt.2020.581426
Favreau M, Hillert A, Osen B et al (2021) Psychological consequences and differential impact of the COVID-19 pandemic in patients with mental disorders. Psychiatry Res. https://doi.org/10.1016/j.psychres.2021.114045
Hao F, Tan W, Jiang L et al (2020) Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun 87:100–106. https://doi.org/10.1016/j.bbi.2020.04.069
Cacioppo JT, Cacioppo S (2018) The growing problem of loneliness. Lancet (London, England) 391:426. https://doi.org/10.1016/S0140-6736(18)30142-9
Burrai J, Roma P, Barchielli B et al (2020) Psychological and emotional impact of patients living in psychiatric treatment communities during Covid-19 lockdown in Italy. J Clin Med 9:3787. https://doi.org/10.3390/JCM9113787
Mills EHA, Møller AL, Gnesin F et al (2020) National all-cause mortality during the COVID-19 pandemic: a Danish registry-based study. Eur J Epidemiol 35:1. https://doi.org/10.1007/S10654-020-00680-X
Sheridan Rains L, Johnson S, Barnett P et al (2021) Early impacts of the COVID-19 pandemic on mental health care and on people with mental health conditions: framework synthesis of international experiences and responses. Soc Psychiatry Psychiatr Epidemiol 56:13–24. https://doi.org/10.1007/S00127-020-01924-7
Taquet M, Luciano S, Geddes JR, Harrison PJ (2020) Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 0366:1–11. https://doi.org/10.1016/S2215-0366(20)30462-4
Lee SW, Yang JM, Moon SY et al (2020) Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry 7:1025–1031. https://doi.org/10.1016/S2215-0366(20)30421-1
Park HY, Song I-A, Lee SH et al (2021) Prevalence of mental illness among COVID-19 survivors in South Korea: nationwide cohort. BJPsych open. https://doi.org/10.1192/BJO.2021.1001
Taquet M, Dercon Q, Luciano S et al (2021) Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. https://doi.org/10.1371/JOURNAL.PMED.1003773
Sass MR, Juul TS, Skov R et al (2022) SARS-CoV-2 seroprevalence among patients with severe mental illness: a cross-sectional study. PLoS One 17:e0264325. https://doi.org/10.1371/JOURNAL.PONE.0264325
Niemi KME, Karjalainen J, Liao RG et al (2021) Mapping the human genetic architecture of COVID-19. Nature 600:472–477. https://doi.org/10.1038/s41586-021-03767-x
Degenhardt F, Ellinghaus D, Juzenas S et al (2022) Detailed stratified GWAS analysis for severe COVID-19 in four European populations. medRxiv. https://doi.org/10.1101/2021.07.21.21260624
Garcia-Moreno C, Jansen HA, Ellsberg M et al (2006) Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet 368:1260–1269. https://doi.org/10.1016/S0140-6736(06)69523-8
Coll CVN, Ewerling F, García-Moreno C et al (2020) Intimate partner violence in 46 low-income and middle-income countries: an appraisal of the most vulnerable groups of women using national health surveys. BMJ Glob Heal 5:e002208. https://doi.org/10.1136/bmjgh-2019-002208
Wright L, Steptoe A, Fancourt D (2021) Does thinking make it so? Differential associations between adversity worries and experiences and mental health during the COVID-19 pandemic. J Epidemiol Community Health 75:817–823. https://doi.org/10.1136/jech-2020-215598
Bratman GN, Anderson CB, Berman MG et al (2019) Nature and mental health: an ecosystem service perspective. Sci Adv. https://doi.org/10.1126/sciadv.aax0903
Orban E, McDonald K, Sutcliffe R et al (2016) Residential road traffic noise and high depressive symptoms after five years of follow-up: results from the heinz nixdorf recall study. Environ Health Perspect. https://doi.org/10.1289/ehp.1409400
Park J, Chung S, Lee J et al (2017) Noise sensitivity, rather than noise level, predicts the non-auditory effects of noise in community samples: a population-based survey. BMC Public Health. https://doi.org/10.1186/s12889-017-4244-5
Ministerio de Sanidad Consumo y Bienestar Social (2017) Informe monográfico de Salud Mental, Madrid
Cénat JM, Noorishad PG, Kokou-Kpolou CK et al (2021) Prevalence and correlates of depression during the COVID-19 pandemic and the major role of stigmatization in low- and middle-income countries: a multinational cross-sectional study. Psychiatry Res. https://doi.org/10.1016/j.psychres.2021.113714
Czeisler M, Lane RI, Wiley JF et al (2021) Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, september 2020. JAMA Netw open. https://doi.org/10.1001/JAMANETWORKOPEN.2020.37665
Gagné T, Schoon I, McMunn A, Sacker A (2021) Mental distress among young adults in Great Britain: long-term trends and early changes during the COVID-19 pandemic. Soc Psychiatry Psychiatr Epidemiol. https://doi.org/10.1007/S00127-021-02194-7
Santomauro DF, Mantilla Herrera AM, Shadid J et al (2021) Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet (London, England) 398:1700–1712. https://doi.org/10.1016/S0140-6736(21)02143-7
Equipo COVID-19 (2020) Informe no 42. Situación de COVID-19 en España, Madrid
Acknowledgements
The authors wish to acknowledge all the GCAT volunteers who participate in the study, Victor Moreno and Delphine Casabonne for their support, and lab staff involved in the serology: Alfons Jiménez, Marta Vidal, Rebeca Santano, Diana Barrios, Laura Puyol, Leonie Mayer, Rocío Rubio, Luis Izquierdo and Ruth Aguilar.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This study was conducted in the framework of the support "Incentius a l’Avaluació de Centres CERCA (in_CERCA)", according to the resolution on 20th Dec 2019 from the president of the Executive Board of the AGAUR. ISGlobal acknowledges support from the Spanish Ministry of Science and Innovation through the “Centro de Excelencia Severo Ochoa 2019–2023” Program (CEX2018-000806-S), and support from the Generalitat de Catalunya through the CERCA Program. This study makes use of data generated by the GCAT-Genomes for Life. Cohort study of the Genomes of Catalonia, Fundacio IGTP. IGTP is part of the CERCA Program / Generalitat de Catalunya. GCAT is supported by Acción de Dinamización del ISCIII-MINECO and the Ministry of Health of the Generalitat of Catalunya (ADE 10/00026); the Agència de Gestió d’Ajuts Universitaris i de Recerca (AGAUR) (2017-SGR 529). BC is supported by national grants PI18/01512. Full list of the investigators who contributed to the generation of the GCAT data is available from www.genomesforlife.com. PD is funded by a Ramón y Cajal fellowship [RYC-2012–10995] awarded by the Spanish Ministry of Economy and Finance. M Foraster is a beneficiary of an AXA Research Fund grant. LeRAgs is funded by Instituto de Salud Carlos III (PI17/01555).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Parc de Salut Mar Ethics Committee (CEIm-PS MAR, number 2020/9307/I). All participants provided informed consent.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goldberg, X., Castaño-Vinyals, G., Espinosa, A. et al. Mental health and COVID-19 in a general population cohort in Spain (COVICAT study). Soc Psychiatry Psychiatr Epidemiol 57, 2457–2468 (2022). https://doi.org/10.1007/s00127-022-02303-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02303-0