Abstract
Purpose
We explored if patients with treatment-resistant depression (TRD) go through different states of labor market affiliation during their course of illness before they return to work or obtain early retirement as compared to patients without TRD.
Methods
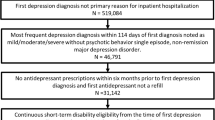
All adults between 18 and 58 years with a first-time hospital contact due to depression in Danish patients’ registers from 2000 to 2014 were followed in a nationwide labor market database. At time of TRD (index week), TRD patients were matched with patients without TRD in a 1:2 ratio. Sequence analysis and logistic regression were applied to explore the association of TRD and labor market affiliation and measures of transitions between labor market states 52 weeks before and after the index week.
Results
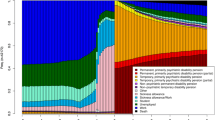
At the index week, 14.1% of patients with TRD were in employment, whereas the proportion was 26.4% among non-TRD patients. Over time, the proportion of patients in employment increased slightly to 25.5% for TRD and 33.7% for non-TRD patients. The proportion of TRD patients with sickness absence at index was 47.0%, while the proportion was 26.2% for non-TRD patients. The adjusted odds of a below mean volatility of labor market transitions, characterized by more episodes in passive social transfer payments and disability pension, were higher among patients with TRD compared with non-TRD patients (OR 1.63, 95% CI [1.56–1.69]). Similarly, the adjusted odds of a below mean integration into employment were 1.63 higher among TRD patients compared with non-TRD patients (95% CI [1.56–1.70]).
Conclusion
Patients with TRD have higher levels of sickness absence and lower levels of reintegration into the labor market after meeting the criteria for TRD compared with patients without TRD.


Similar content being viewed by others
Data availability
All data were retrieved from the Danish Health Data Authority and Statistics Denmark. Access to data is ongoing. Admission to data can be obtained after approval by the Danish Data Protection Agency and Statistics Denmark.
References
Vos T, Lim SS, Abbafati C et al (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396:1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Koopmans PC, Roelen C, a. M, Groothoff JW, (2008) Sickness absence due to depressive symptoms. Int Arch Occup Env Health 81:711–719. https://doi.org/10.1007/s00420-007-0243-7
Nielsen MBD, Bültmann U, Madsen IEH et al (2012) Health, work, and personal-related predictors of time to return to work among employees with mental health problems. Disabil Rehabil 34:1311–1316. https://doi.org/10.3109/09638288.2011.641664
Leijon O, Josephson M, Österlund N (2015) Sick-listing adherence: a register study of 1.4 million episodes of sickness benefit 2010–2013 in Sweden. BMC Public Health 15:380. https://doi.org/10.1186/s12889-015-1741-2
Pedersen P, Lund T, Lindholdt L et al (2016) Labour market trajectories following sickness absence due to self-reported all cause morbidity—a longitudinal study. BMC Public Health 16:337. https://doi.org/10.1186/s12889-016-3017-x
Levinson D, Lakoma MD, Petukhova M et al (2010) Associations of serious mental illness with earnings: results from the WHO world mental health surveys. Br J Psychiatry J Ment Sci 197:114–121. https://doi.org/10.1192/bjp.bp.109.073635
Schofield D, Cunich M, Shrestha R et al (2019) Indirect costs of depression and other mental and behavioural disorders for Australia from 2015–2030. BJPsych Open 5:e40. https://doi.org/10.1192/bjo.2019.26
Lassemo E, Sandanger I, Nygård JF, Sørgaard KW (2016) Predicting disability pension—depression as hazard: a 10 year population-based cohort study in norway: predicting disability pension—depression as hazard. Int J Method Psychiatr Res 25:12–21. https://doi.org/10.1002/mpr.1473
Bultmann U, Christensen KB, Burr H et al (2008) Severe depressive symptoms as predictor of disability pension: a 10-year follow-up study in Denmark. Eur J Public Health 18:232–234. https://doi.org/10.1093/eurpub/ckm132
Greden JF (2001) The burden of disease for treatment-resistant depression. J Clin Psychiatry 62(Suppl 16):26–31
Gronemann FH, Jorgensen MB, Nordentoft M et al (2020) Socio-demographic and clinical risk factors of treatment-resistant depression: a Danish population-based cohort study. J Affect Disord 261:221–229. https://doi.org/10.1016/j.jad.2019.10.005
Kubitz N, Mehra M, Potluri RC et al (2013) Characterization of treatment resistant depression episodes in a cohort of patients from a US commercial claims database. PLoS ONE 8:e76882. https://doi.org/10.1371/journal.pone.0076882
Ivanova JI, Birnbaum HG, Kidolezi Y et al (2010) Direct and indirect costs of employees with treatment-resistant and non-treatment-resistant major depressive disorder. Curr Med Res Opin 26:2475–2484. https://doi.org/10.1185/03007995.2010.517716
Gaynes BN, Warden D, Trivedi MH et al (2009) What did STAR*D teach Us? results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv 60:1439–1445. https://doi.org/10.1176/ps.2009.60.11.1439
Bang Madsen K, Vogdrup Petersen L, Plana-Ripoll O et al (2020) Early labor force exits in patients with treatment-resistant depression: an assessment of work years lost in a Danish nationwide register-based cohort study. Ther Adv Psychopharmacol 10:204512532097379. https://doi.org/10.1177/2045125320973791
Taipale H, Reutfors J, Tanskanen A et al (2020) Risk and risk factors for disability pension among patients with treatment resistant depression–a matched cohort study. BMC Psychiatry 20:232. https://doi.org/10.1186/s12888-020-02642-9
Øyeflaten I, Lie SA, Ihlebæk CM, Eriksen HR (2012) Multiple transitions in sick leave, disability benefits, and return to work—a 4-year follow-up of patients participating in a work-related rehabilitation program. BMC Public Health 12:748. https://doi.org/10.1186/1471-2458-12-748
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish national patient register. Scand J Public Health 39:30–33. https://doi.org/10.1177/1403494811401482
Conway CR, George MS, Sackeim HA (2017) Toward an evidence-based, operational definition of treatment-resistant depression: when enough is enough. JAMA Psychiat 74:9. https://doi.org/10.1001/jamapsychiatry.2016.2586
Wallach Kildemoes H, Toft Sørensen H, Hallas J (2011) The Danish national prescription registry. Scand J Public Health 39:38–41. https://doi.org/10.1177/1403494810394717
Hjollund NH, Larsen FB, Andersen JH (2007) Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health 35:497–502. https://doi.org/10.1080/14034940701271882
Lindholdt L, Labriola M, Nielsen CV et al (2017) Sequence analysis to assess labour market participation following vocational rehabilitation: an observational study among patients sick-listed with low back pain from a randomised clinical trial in Denmark. BMJ Open 7:e015661. https://doi.org/10.1136/bmjopen-2016-015661
Brzinsky-Fay C (2007) Lost in transition? labour market entry sequences of school leavers in Europe. Eur Sociol Rev 23:409–422. https://doi.org/10.1093/esr/jcm011
Lindholdt L, Lund T, Andersen JH, Labriola M (2020) Labour market attachment among parents and self-rated health of their offspring: an intergenerational study. Eur J Public Health 30:584–589. https://doi.org/10.1093/eurpub/ckz213
Pedersen CB (2011) The Danish civil registration system. Scand J Public Health 39:22–25. https://doi.org/10.1177/1403494810387965
Jensen VM, Rasmussen AW (2011) Danish education registers. Scand J Public Health 39:91–94. https://doi.org/10.1177/1403494810394715
Brzinsky-Fay C, Kohler U, Luniak M (2006) Sequence analysis with stata. Stata J Promot Commun Stat Stata 6:435–460. https://doi.org/10.1177/1536867X0600600401
Gasse C, Petersen L, Chollet J, Saragoussi D (2013) Pattern and predictors of sick leave among users of antidepressants: a Danish retrospective register-based cohort study. J Affect Disord 151:959–966. https://doi.org/10.1016/j.jad.2013.08.015
Roelen CAM, Koopmans PC, Schreuder JAH et al (2011) The history of registered sickness absence predicts future sickness absence. Occup Med 61:96–101. https://doi.org/10.1093/occmed/kqq181
Johnston DA, Harvey SB, Glozier N et al (2019) The relationship between depression symptoms, absenteeism and presenteeism. J Affect Disord 256:536–540. https://doi.org/10.1016/j.jad.2019.06.041
Lidwall U (2015) Sick leave diagnoses and return to work: a Swedish register study. Disabil Rehabil 37:396–410. https://doi.org/10.3109/09638288.2014.923521
Statistics Denmark activity and employment rates (RAS200) https://www.statbank.dk/statbank5a/SelectVarVal/Define.asp?Maintable=RAS200&PLanguage=1. Accessed 21 Jan 2021
Gammelgaard I, Christensen TN, Eplov LF et al (2017) ‘I have potential’: experiences of recovery in the individual placement and support intervention. Int J Soc Psychiatry 63:400–406. https://doi.org/10.1177/0020764017708801
Christensen TN, Nielsen IG, Stenager E et al (2015) Individual placement and support supplemented with cognitive remediation and work-related social skills training in Denmark: study protocol for a randomized controlled trial. Trials 16:280. https://doi.org/10.1186/s13063-015-0792-0
Hundrup E, Osler M, Jørgensen MB (2017) Time trends and variations in electroconvulsive treatment in Denmark 2008–2014: a nationwide register-based study. J ECT 33:243–248. https://doi.org/10.1097/YCT.0000000000000381
Hägg D, Brenner P, Reutfors J et al (2020) A register-based approach to identifying treatment-resistant depression—comparison with clinical definitions. PLoS ONE 15:e0236434. https://doi.org/10.1371/journal.pone.0236434
Gronemann FH, Jorgensen MB, Nordentoft M et al (2018) Incidence of, risk factors for, and changes over time in treatment-resistant depression in Denmark: a register-based cohort study. J Clin Psychiatry. https://doi.org/10.4088/JCP.17m11845
Funding
This study was funded by the Danish Council for Independent Research (grant ID: DFF-6110-00195). The funding source was not involved in the conduct of research or the preparation of the present manuscript.
Author information
Authors and Affiliations
Contributions
All listed authors contributed to the design and planning of this study. Collection of and access to data was obtained by MO, MN, and MBJ. Data management and data analyses were performed by FHG with support from LL, TL, and MO. FHG drafted the article. All co-authors contributed to data interpretation, critical revision and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the Danish data protection authorities. According to Danish law, ethical approval and informed consent are not required for register-based studies.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gronemann, F.H., Lund, T., Lindholdt, L. et al. Treatment-resistant depression and labor market affiliation in the Danish welfare society: a register-based study. Soc Psychiatry Psychiatr Epidemiol 57, 1189–1199 (2022). https://doi.org/10.1007/s00127-022-02243-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02243-9