Abstract
Objective
The overall rate of suicide in French Guiana is estimated at 6 per 100,000, a rate that is lower than in mainland France. Given the frequent reports of suicide in Amerindian communities, our hypothesis was that this figure fails to capture a more contrasted reality. Our objective was to refine estimates and determine suicide rates in remote villages of French Guiana.
Methods
We included patients for whom a suicide attempt or suicide was mentioned in medical records. The Health centers were grouped into two zones according to geographical remoteness.
Results
The highest suicide rates observed in the remote Amerindian villages of Camopi and Trois Sauts were, respectively, 118 and 78/100,000. The median age at the time of suicide was significantly younger in remote zones [23 years (95% CI 21.59–25.06)] than in non-remote zones—[27 years (95% CI 24.47–29.31)]. The most frequent methods were hanging (78%) and intoxication (22%).
Conclusions
The suicide rate in remote areas in French Guiana was eight times higher than in France. The suicide of young people in remote areas in French Guiana and specifically in Amerindian villages must be better understood and prevented with contextualized and adapted care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2012, there were an estimated 800,000 suicides worldwide, which corresponds to 11.4 suicide deaths per 100,000 population (15 among men and 8 among women) [1].
In mainland France, the National Suicide Observatory estimated that there were 12,000 suicides per year (16 per 100,000 in 2012). The most at-risk populations were men aged 45–54 years and > 75 years [2, 3].
French Guiana does not have any suicide registry. Suicide data obtained from death certificates compiled by the CEPIDC estimates the suicide incidence in 2014 at 15 for 252,338 which represents a rate of 6 per 100,000.
Patient management in French Guiana mostly relies on the three hospitals located along the coastal area, in Cayenne, Saint Laurent du Maroni, and Kourou. Outside of these areas, patient care rests on a network of health centers [Centres Délocalisés de Prévention et de Soins (CDPS)]. Some of these health centers are located in the coastal area, where 80% of the population resides, and are connected by road [4]. The others deliver care for the remaining 20% of the population, and they are only accessible by canoe or by air. Thus, the most severe cases lead to emergency medical evacuations by helicopter mostly towards the main regional hospital in Cayenne.
In France, death is pronounced by a doctor which is problematic in the remote villages in French Guiana, where doctors are not always present; in addition, early burials without soliciting the help of health professionals lead to an underreporting of suicide cases.
Published data on suicide in French Guiana are scarce and mostly mention Amerindian territories for which there are actually few reliable data to estimate the magnitude of the problem [5,6,7].
Autochthonous populations living in the interior of French Guiana are concentrated along the Maroni (Antecum Pata and Talhuen) and Oyapock (Camopi and TroisSauts) rivers. The Amerindian population in these areas is estimated at 2700 persons, whereas for all of French Guiana it is around 10,000 [8].
In the absence of objective data on a phenomenon that is highly reported in the media, the main objective of the present study was to describe the epidemiology of suicide and suicide attempts in the remote health centers of French Guiana between 2007 and 2016.
Materials and methods
A retrospective observational study was conducted using data from the health centers’ network’s information system and Cayenne hospital emergency department’s medical records between 2007 and 2016.
Our definition of suicide was based on the 2014 WHO report “the term suicide refers to the act of killing oneself”, suicide attempts “the term suicide attempt refers to any non lethal suicidal behavior, and to self-intoxication, self mutilation, self-aggression with or without the intention to die” [1]. However, in an Amazonian context where accidents are frequent, we only considered cases where the intent of attempting to harm one’s life was explicit.
Inclusion criteria
Cases were compiled from the health centers’ information system and from the medical records at the emergency department for patients who were not in the health centers’ database and benefitted from medical evacuation towards Cayenne.
Cases were selected using the tenth international classification of diseases ICD10 coding for self-intoxication, or self-inflicted injury. Some cases for which only a suicide attempt (intentional self-injury or intoxication with a notion of lethal intent) was specified in the medical record were retained.
Cases were classified as intoxications when the following main diagnoses were coded: X40, X60, X61, X62, X69 and X84 or as injuries when the consultation diagnosis was: W33, X70, X71, X72-X73, X74, X78 and X84. These codes were used as main diagnosis in the health centers’ information system because it is not integrated in the hospital’s French standardized information system (PMSI) that would not allow for it. Some of these codes are not related to suicide but they were part of the first data queries to verify if there was any lethal intention in the records, in which case the patient was excluded. The aim of this was to avoid missing suicides that would have been mistakenly coded as intoxications.
Exclusion criteria
Self-intoxications among children less than 10 years, and self-intoxications among adults without confirmation in the medical records were excluded from the study.
In zone 1, the coastal area, it is possible (although very rare especially for a severe psychiatric or organic problem) that a few patients may directly reach the hospital without first being seen by a doctor in the health center. However, in Kourou and Saint Laurent, the emergency ward medical records are not computerized and were not accessible, they were available in Cayenne where, in the 10-year study period, three suicide attempts and zero suicides came directly to the hospital without first going through a health center. Given the heterogeneity in data collection introduced by the absence of data from Kourou and Saint Laurent Emergency wards, we decided to adopt a uniform criterion, which seemed more rigorous. Suicide attempts for which patients went directly to the hospital without first going to the local health center were thus excluded. This possibility only concerned zone 1. In zone 2, corresponding to the most remote areas, all suicide attempts must go through the health center. Only suicide attempts, for which there was an intervention of the local medical team were counted. All suicide attempts that were reported a posteriori for which there was no health center solicitation were excluded.
Grouping of health centers
Health centers connected to the road system are located in zone 1 which included the health centers of Apatou, Awala, Javouhey, Iracoubo, Cacao, Regina and St Georges. The total population for zone 1 according to the 2011 census was estimated to be 18,122 inhabitants. Zone 2, for which access is only possible by canoe or by air (plane/helicopter) includes the health centers of Camopi and TroisSauts on the Oyapock, and the health centers of Grand Santi, Papaïchton, Maripasoula, Talhuen and Antecum Pata on the Maroni, and finally, Kaw and Saul in central French Guiana. The population of zone 2 is estimated to be 22,719 inhabitants [9] (Fig. 1).
Statistical analysis
First, a descriptive analysis was performed on the data from the interior of French Guiana. Then, suicide numbers and suicide attempts in zone 1 and zone 2 were compared. Chi squared or Fisher’s exact test were used where appropriate. The rank-sum test was used to compare non-normally distributed variables. Suicide rates were obtained by dividing the number of suicide cases by the population size as estimated during the 2011 census. The data was analyzed using STATA 13 (Stata Statistical Software Release 13. College Station, TX, USA: Stata Corp LP.).
Results
Suicide attempts’ numbers and rates
Between 2007 and 2016, 236 suicide attempts were tallied, which corresponds to a yearly suicide attempt rate of 58 per 100,000.
In zone 1, there were 84 known suicide attempts and in zone 2 there were 152, which yields an annual average incidence rate of 46 and 67 per 100,000, respectively (Table 1).
The highest suicide attempt rates were localized in zone 2 notably in Trois Sauts and Camopi on the Oyapock river. In the Amerindian territories on the Maroni, the rates are also high (Figs. 1, 2, 3).
Number and rate of suicide attempts according to age and sex
The sex ratio was 0.46 (75 men and 161 women) with no significant difference between zones. The youngest patient was 10 years old, and the oldest was 86 years.
The median age at the time of suicide attempts was significantly younger in zone 2 than in zone 1, 23 versus 27 years (p = 0.0087) (Table 1).
The 10–19-year-olds represented 41% of cases. When considering the 10–29-year-old group, it represented 75% of cases (Fig. 3).
Suicide attempt method by sex and area of residence
Suicide attempts in women mostly consisted of intoxications (which could consist of different products or medications), while men were twice less likely to use this method (Table 2).
Among women, suicide attempt methods were significantly different between zone 1 and 2, with a greater proportion of hangings in zone 2, notably in Camopi, Trois Sauts, Antecum Pata and Talhuen which concentrated 88% of hanging attempts of women in zone 2, on par with males (Table 2).
Among men, suicide attempts mostly corresponded to hangings.
It was noteworthy that in Maripasoula, 50% of suicides corresponded to paraquat intoxications (Fig. 3).
Suicide numbers and rate
From 2007 to 2016, 37 suicides were registered in the health centers, which is a yearly rate of 9 per 100,000. This rate was more than three times higher in zone 2 than in zone 1 (13 per 100,000 versus 4 per 100,000) (Table 1).
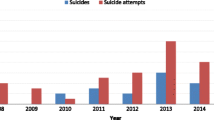
The largest numbers were in Camopi and Trois Sauts (Fig. 1). Although total numbers were small, there was a gradual increase over time (Fig. 4).
Suicide by age and sex
The sex ratio was 2 and the median age was 26 years. The 10–19-year-olds represented 46% of cases, followed by the 30–39 (27%) then the 20–29 (19%).
In zone 2 the median age was significantly younger than in zone 1: 24 versus 33 years (p = 0.015) (Table 1). For comparisons with Latin America, we computed the 10–19 year old average suicide rate which was 42 per 100,000.
Suicide by method and sex
78% of suicides were injuries (65% hanging, 13% gunshot wound), and were more frequent in men than in women. Suicide by intoxication (22%) was exclusively linked to paraquat and there was no difference between men and women (Tables 1, 2; Fig. 5).
Suicide attempt fatality rate
Among all suicide attempts, 13.5% led to death. In zone 2, fatality was 19.7%, whereas in zone 1 it was 8.3% (p < 0.001). Among the 31 who ingested paraquat, the fatality rate was 26% (8 died and 23 survived).
Discussion
French National estimates for French Guiana, based on hospital records, reported an incidence rate of 51 suicide attempts per 100,000 in 2013, which was 71% lower than in mainland France [6, 9, 10]. These estimates are biased by the fact that 78% of suicide attempts in the interior do not lead to medical evacuation in the main hospitals of French Guiana. Thus, these macro statistics do not capture the heterogeneity of the epidemiology of suicide attempts and suicides in French Guiana.
Our study shows that behind the falsely reassuring suicide statistics in French Guiana there are high risk areas for suicide, with a suicide rate that is eight times higher than in France and a suicide attempt rate double of that in mainland France [3, 10].
Beyond the quantitative aspects there are remarkable qualitative features of suicide in the interior of French Guiana. Global and French national statistics indicate that women are three times more likely to attempt suicide than men, mostly through medication intoxication [1, 2, 6, 9, 10], but in our study there are some spatial/ethnic heterogeneities regarding the methods: in the maroon territories of Grand Santi, Papaïchton and Maripasoula medications or pesticides are mostly used, whereas in the Amerindian territories women use hanging or guns. These differences were not salient among men for whom most suicide attempts relied on hanging. Suicide attempts through intoxication were only observed along the Maroni.
For suicide, this regional/ethnic pattern was even more pronounced. There was a focus of suicide in the Amerindian towns of Camopi and Trois Sauts where hanging was the most frequent method used.
Whereas in mainland France, the suicide rate increases with age [2, 3], and the data in the remote territories of French Guiana show that suicide disproportionally affects teenagers and young adults and declines with age. Suicide prevention should thus target the most at-risk age ranges. With 30% lethality among men and 17% among women, and the methods used in suicide attempts underline the frequent intentionality of dying. These observations are similar to what is observed in the region where suicide among youth is a major problem and where similar methods are used [11]. When comparing the incidence rates of suicide among youth in different Latin American countries, we find that on the Guiana shield, Guyana, and Suriname have the highest suicide rates among young people [11, 12]. Although the present study presents a more isolated subset of the population of French Guiana, the rates we observed were also very high, and even higher when we only included the younger age groups. Hence in zone 2, on average the suicide rate was 42 per 100,000, whereas in Guyana it was 31.4 and in Suriname 19.8. Slow economic growth has been hypothesized to contribute to high suicide rates in Latin America, although the interior of French Guiana may offer few economic prospects, French Guiana has the highest GDP per capita in Latin America which seems to rule out the socioeconomic hypothesis. In Suriname and Guyana, suicide disproportionally affects patients in Hindustani cultures, whereas in French Guiana it mostly affects Amerindians. Whereas in French Guiana, there were marked spatiotemporal trends, it has been reported that in Guyana there was little evidence for Tarde’s theory of imitation, and little evidence for geographical patterns [13]. The main problem was linked to relational problems within the Hindustani community, with strong pressures for young generations to conform. Therefore apart from being countries of comparable sizes on the Guiana shield with remote areas, one common factor between Hindustani cultures in Guyana and Suriname and Amerindian cultures of the interior of French Guiana may be the strong pressure for the young generation and its global cultural references to conform to the older generations’ entrenched values and status ladder [13]. Cultural and/or geographical isolation leave few ways of escaping conflicts that unfold behind closed doors.
The vulnerability of autochthonous populations and the frequency of suicide have been extensively described in Canada, Alaska, Brazil, or the USA. In the above autochthonous populations, the cases’ profile is often similar to what we observed [14,15,16,17,18,19,20,21,22,23].
However, the precise reasons explaining these broad trends are debated. Some authors have raised the hypothesis of specific genetic or epigenetic factors influencing decision making and the acuteness of the feeling of rejection leading to a higher vulnerability for suicide [24,25,26,27]. Social and geographic isolation and intoxication have an important role on the enactment of suicide [1, 3, 28]. The present data show that the risk is much higher in the isolated Amerindian territories than in the isolated maroon territories, which suggests additional populational factors. A previous study in Camopi-Trois Sauts, with a small qualitative component showed a lethal mix of isolation, desperation in the perceived lack of future prospects, depression, frequent alcohol addiction and substance use, conflict, and a history of abuse [29]. An additional hypothesis, could be the turbulent transition between “gerontocratic” cultures where elders are at the top of the social structure to a more neontocratic modern culture where the values of youth become preeminent [30]. Indeed, new technologies permeate through the distant Amazonian villages and advertisements and music videos bring new status references, references that are reinforced when young generations go to the coastal part of French Guiana for their studies. Thus staying or returning to the most remote areas, with traditional values may be very confusing.
In the past 10 years, numerous suicide prevention programs have been developed. The prevention of suicide, the reduction of social isolation, and the diagnosis and treatment of depression in the interior of French Guiana still need to be developed [1, 28]. Several prevention programs have been developed in the Upper Maroni area. It is noteworthy that there was no suicide in Antecum Pata, where there is a stronger presence of a non-government organization and a sentinel system allowing the proximity of local cultural mediators and the population. Although it is no definite proof, it is tempting to infer that their intervention has been successful in reducing the risk of suicide. A factor that may not be neutral is the recent massive evangelization in Amerindian territories. The putative protective role of religion on suicide is however controversial and the impact of this trend on the well-being of populations needs to be monitored [31, 32]. The data from this study show that the high suicide rate does not concern all Amerindians in French Guiana but about 30% of this population, those living in the most isolated areas on the upper Maroni and Oyapock rivers. The remaining 70% do not seem to be disproportionally affected by the problem of suicide.
Although injury suicides, notably by hanging remain the most frequent method, in recent years there has been an increase in suicides with paraquat, a herbicide that is forbidden in French territories since 2007 but which is authorized in neighboring Suriname. Overall, 20% of suicides used paraquat, notably in Maripasoula, which is a business hub on the Maroni with neighboring Suriname.
A doctoral thesis on paraquat intoxications found a lethality rate of 51.7%, which is higher than the observed 26%, perhaps because the broader inclusion criteria included accidental ingestions by children, and intoxications in all hospitals and not only the health centers network [33].
The present study has some limitations. The exhaustivity of the compilation of suicide attempts may be debatable for several reasons. First, the WHO has no precise definition of suicide or suicide attempts, which would allow facilitating the task [1]. The direct link of the health centers with the hospital may have biased estimations through the undercounting of suicide attempts in the health centers in zone 1, where patients may have the option of driving to a hospital. In addition, early burial, which is more frequent in zone 2, may have led to underestimating actual suicide numbers in the interior. Given the complexity of counting suicides and suicide attempts, the process should ideally be proactive with different actors (NGO’s, institutions) coordinated by a regional observatory for suicide. The small numbers in these remote areas, and the stratification in subgroups may lead to important fluctuations and are known to promote more extreme values. Rates are crude and could not be standardized because in some of the towns the age categorizations are not those used in the population used for standardization. Suicide rates may fluctuate in time with epidemic waves and Werther effects that our 10-year scale may mask.
Despite these limitations, and probable undercounting, the magnitude of the suicide rate in these remote areas is still patently very high with nearly all persons in the concerned villages witnessing the event, a very traumatizing experience for the local populations. This is a first quantification effort in these underserved areas that are living private dramas that are not captured by national statistics. Interdisciplinary efforts should be implemented to better understand and thus prevent suicide in the remote villages in the interior of French Guiana.
References
World Health Organization (2015) Prévention du suicide: l’Etat d’urgence mondiale. World Health Organization, Geneva
Observatoire national du suicide (France) (2014) Suicide: état des lieux des connaissances et perspective de recherche. Observatoire national du suicide (ONS), Paris
Ministere de la solidarité et de la santé.pdf (Internet). http://solidarites-sante.gouv.fr/prevention-en-sante/sante-mentale-et-psychiatrie/article/etat-des-lieux-du-suicide-en-france#Le-suicide-en-France. Accessed 15 June 2018
INSEE. Institut national de la statistique et des études économique INSEE. https://www.insee.fr/fr/statistiques/2540209. Accessed 15 June 2018
Navet É, Mohia N (1990) Considérations sur la situation des Amérindiens de l’intérieur de la Guyane. J Société Américanistes 76(1):215–227
InVS (2012) Données Epidémiologique des Tentatives de suicides et de suicide en Guyane. http://invs.santepubliquefrance.fr/Dossiers-thematiques/Maladies-chroniques-et-traumatismes/Sante-mentale/Donnees-de-surveillance-par-pathologie/Tentatives-de-suicide-et-suicides. Accessed 20 Aug 2018
Archimbaud A, Chapdelaine A (2015) Suicides des jeunes Amérindiens en Guyane française: 37 propositions pour enrayer ces drames et créer les conditions d'un mieux être. Nov 2015 report to the prime minister. http://www.ladocumentationfrancaise.fr/var/storage/rapports-publics/154000882.pdf. Accessed 20 Aug 2018
IWGIA France. Amérindiens de Guyane (Internet). https://gitpa.org/Peuple%20GITPA%20500/gitpa500-2-GUYANEfiche.pdf. Accessed 15 June 2018
Santé publique France InVS (2014). http://www.sante.gouv.fr/IMG/pdf/rapport_hospitalisations_tentative_suicide_france_pmsimco_oscour_2007-2011-2.pdf. Accessed 20 Aug 2018
Premiers résultats du Baromètre santé DOM 2014—Résultats détaillés selon le DOM, l’âge et le sexe—2015:32. https://inpes.santepubliquefrance.fr/CFESBases/catalogue/pdf/1785.pdf. Accessed 15 June 2018
Quinlan-Davidson M, Sanhueza A, Espinosa I, Escamilla-Cejudo JA, Maddaleno M (2014) Suicide among young people in the Americas. J Adolesc Health 54(3):262–268
Graafsma T, Kerkhof A, Gibson D, Badloe R, van de Beek LM (2006) High rates of suicide and attempted suicide using pesticides in Nickerie, Suriname, South America. Crisis 27(2):77–81
Edwards D (2003) Suicide in Guyana: a sociological analysis. https://pdfs.semanticscholar.org/5057/b1e3baf935f1014f0a6d617b7fb0a05e967f.pdf. Accessed 20 Aug 2018
Tousignant M, Laliberté A, Bibeau G, Noël D (2008) Comprendre et agir sur le suicide chez les Premières Nations: Quelques lunes après l’initiation. Frontières 21(1):113
Fleury S (2016) Bien-être et pratiques culturelles. Comparaison du cas des Inuit du Nunavut au Canada et des Quichuas du Napo en Amazonie équatorienne. Études Can Can Stud 80:203–218
Kral MJ (2016) Suicide and suicide prevention among inuit in Canada. Can J Psychiatry 61(11):688–695
Charlier P, Malaurie J, Wasserman D, Carli V, Sarchiapone M, Dagenais-Everell C et al (2017) The EPA guidance on suicide treatment and prevention needs to be adjusted to fight the epidemics of suicide at the North Pole area and other autochthonous communities. Eur Psychiatry 41:129–131
MacNeil MS (2008) An epidemiologic study of aboriginal adolescent risk in Canada: the meaning of suicide. J Child Adolesc Psychiatr Nurs 21(1):3–12
Middlebrook Denise L, LeMaster Pamela L, Janette B, Novins Douglas K, Manson Spero M (2011) Suicide prevention in American Indian and Alaska native communities: a critical review of programs. Suicide Life Threat Behav 31(s1):132–149
May PA, Serna P, Hurt L, DeBruyn LM (2005) Outcome evaluation of a public health approach to suicide prevention in an American Indian tribal nation. Am J Public Health 95(7):1238–1244
Orellana JDY, Basta PC, de Souza MLP (2013) Mortality by suicide: a focus on municipalities with a high proportion of self-reported indigenous people in the state of Amazonas, Brazil. Rev Bras Epidemiol Braz J Epidemiol 16(3):658–669
Pollock NJ, Mulay S, Valcour J, Jong M (2016) Suicide rates in aboriginal communities in Labrador, Canada. Am J Public Health 106(7):1309–1315
Borowsky I, Resnick MD, Ireland M, Blum RW (1999) Suicide attempts among American Indian and Alaska native youth: risk and protective factors. Arch Pediatr Adolesc Med 153(6):573–580
Turecki G (2014) Epigenetics and suicidal behavior research pathways. Am J Prev Med 47(3):S144–S151
Oquendo MA, Sullivan GM, Sudol K, Baca-Garcia E, Stanley BH, Sublette ME et al (2014) Toward a biosignature for suicide. Am J Psychiatry 171(12):1259–1277
Coryell W, Schlesser M (2001 May) The dexamethasone suppression test and suicide prediction. Am J Psychiatry 158(5):748–753
Brown T (2014) Identification and replication of a combined epigenetic and genetic biomarker predicting suicide and suicidal behaviors. Am J Psychiatry 171:1287–1296
(2014) Évaluation du programme national d’actions contre le suicide 2011–2014. 74. https://www.hcsp.fr/Explore.cgi/avisrapportsdomaine?clefr=554. Accessed 20 Aug 2018
Pacot R, Guarmit B, Pradem M, Nacher M, Brousse P (2018) The problem of suicide among Amerindians in Camopi-Trois Sauts, French Guiana 2008–2015. BMC Psychiatry 18(1):99. https://doi.org/10.1186/s12888-018-1670-6
Lancy DF (2008) The anthropology of childhood: cherubs, chattel, changelings. Cambridge University Press, Cambridge
Le Clainche C, Courtet P. Facteurs de risque de suicide et de vulnérabilité au suicide. Observatoire National du suicide, 2ème rapport. http://drees.solidarites-sante.gouv.fr/IMG/pdf/ons2016_dossier2.pdf. Accessed 20 Aug 2018
Hsieh N (2017) A global perspective on religious participation and suicide. J Health Soc Behav 58(3):322–339
Merlin PC (2015) Intoxication au paraquat en Guyane Française de 2008 à 2015: une étude de 62 cas. 101. http://pepite-depot.univ-lille2.fr/nuxeo/site/esupversions/913842e0-c73b-44b7-838f-176e7b5214fe. Accessed 15 June 2018
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Regulatory and ethical aspects
The retrospective analysis of aggregated data is authorized by the Commission Nationale Informatique et Libertés. The Information system of the Centres Délocalisés de Prévention et de Soins is declared and authorized by the health authorities.
Rights and permissions
About this article
Cite this article
Guarmit, B., Brousse, P., Lucarelli, A. et al. Descriptive epidemiology of suicide attempts and suicide in the remote villages of French Guiana. Soc Psychiatry Psychiatr Epidemiol 53, 1197–1206 (2018). https://doi.org/10.1007/s00127-018-1570-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-018-1570-6