Abstract
Purpose
Chronic somatic complaint (CSC) can cause significant impairment of psychosocial functioning and therefore is of considerable interest in medicine, psychology, and related health sciences. To date, the type, distribution, and associated factors of CSC have been examined in only a limited number of studies. Main research questions of this investigation focused on the prevalence of CSC, the predictive validity of parent reports, and the associations with social class, health status, and psychosocial distress.
Methods
Data were obtained from a population-based, German-wide representative Health Survey (N = 1,027 self-reports, and parent reports from 11- to 18-year-olds). In addition to study-specific items, the standardized Giessen Physical Complaints Inventory for Children and Adolescents was used (GPCI).
Results
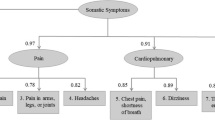
The most frequent CSCs in self-report forms were skin impurities/pimples, cold hands, and fatigue; older adolescents, especially females, were at a higher risk for CSC. The sensitivity of parent reports in all complaints observed was very low (Med = 0.21) and specificity varied between 0.94 and 1.00. Parents significantly underestimated CSC that were not externally observable, as well as CSC in males. Across different predictors and CSC dimensions, psychosocial distress showed the highest predictive value.
Conclusions
The results provide data regarding the subjective physical health of adolescents, as well as an empirical reference to evaluate the distribution of chronic symptoms in specific clinical populations (which is needed for prevention and treatment).

Similar content being viewed by others
References
Barkmann C, Schulte-Markwort M (2005) Emotional and behavioral problems of children and adolescents in germany—an epidemiological screening. Soc Psychiatry Psychiatr Epidemiol 40:357–366
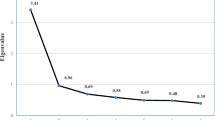
Barkmann C, Mack B, Braehler E, Schulte-Markwort M (2008) The “Gießener Beschwerdebogen für Kinder und Jugendliche” (GBB-KJ): factorial validity, reliability, and standardization of the self- and parent report form for 4- to 18-year-olds. Diagnostica 54:99–111
Barkmann C, Schulte-Markwort M, Braehler E (2007) Physical complaints of children and adolescents in germany—results of a population-based survey. Z Klin Psychol Psychiatr Psychother 55:49–58
Barsky AJ, Borus JF (1999) Functional somatic syndromes. Ann Intern Med 130:910–921
Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchadt CM, Crosby RD (1997) Somatic symptoms in anxious-depressed school refusers. J Am Acad Child Adolesc Psychiatry 36:661–668
Berntsson LT, Gustafsson JE (2000) Determinants of psychosomatic complaints in Swedish schoolchildren aged seven to twelve years. Scand J Public Health 28:283–293
Berntsson LT, Kohler L, Gustafsson JE (2001) Psychosomatic complaints in schoolchildren: a Nordic comparison. Scand J Public Health 29:44–54
Braehler E (1992) The Giessen Physical Complaints Inventory for Children and Adolescents (GPCI). Manual, Huber, Bern
Campo JV, Comer DM, Jansen-McWilliams L, Gardner W, Kelleher KJ (2002) Recurrent pain, emotional distress, and health service use on childhood. J Pediatr 141:576–583
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Hillsdale
Craig TKJ, Cox AD, Klein K (2002) Intergenerational transmission of somatization behaviour: a study of chronic somatizers and their children. Psychol Med 32:805–816
Dhossche D, Ferdinand R, van der Ende J, Verhulst F (2001) Outcome of self-reported functional-somatic symptoms in a community sample of adolescents. Ann Clin Psychiatry 13:191–199
Egger HL, Costello EJ, Erkanli A, Angold A (1999) Somatic complaints and psychopathology in children and adolescents: stomach aches, musculoskeletal pains, and headaches. J Am Acad Child Adolesc Psychiatry 38:852–860
Eminson M (2007) Mecically unexplained symptoms in children and adolescents. Clin Psychol Rev 27:855–871
Fritz GK, Fritsch S, Hagino O (1997) Somatoform disorders in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 36:1329–1338
Garber J, van Slyke DA, Walker LS (1998) Concordance between mothers’ and children’s reports of somatic and emotional symptoms in patients with recurrent abdominal pain or emotional disorders. J Abnorm Child Psychol 26:381–391
Garber J, Walker LS, Zeman J (1991) Somatization symptoms in a community sample of children and adolescents: further validation of the children’s somatization inventory. Psychol Assess 3:588–595
Gledhill J, Garralda ME (2006) Functional symptoms and somatoform disorders in children and adolescents: the role of standardised measures in assessment. Child Adolesc Ment Health 11:208–214
Hagekull B, Bohlin G (2004) Predictors of middle childhood psychosomatic problems: an emotion regulation approach. Infant Child Dev 13:389–405
Haugland S, Wold B (2001) Subjective health complaints in adolescence—reliability and validity of survey methods. J Adolesc 24:611–624
Hessel A, Geyer M, Schumacher J, Braehler E (2003) Somatoforme Beschwerden bei Jugendlichen in Deutschland. Psychotherapeut 48:109–116
Hotopf M (2002) Childhood experience of illness as a risk factor for medically unexplained symptoms. Scand J Psychol 43:139–146
Husain K, Browne T, Chalder T (2007) A review of psychological models and interventions for medically unexplained somatic symptoms in children. Child Adolesc Ment Health 12:2–7
Janicke DM, Finney JW, Riley A (2001) Children’s health care use: a prospective investigation of factors related to care-seeking. Med Care 39:990–1001
Laurell K, Larsson B, Eeg-Olofsson O (2005) Headache in schoolchildren: association with other pain, family history and psychosocial factors. Pain 119:150–158
Lieb R, Mastaler M, Wittchen HU (1998) Are there somatoform disorders in adolescents and young adults? First epidemiological findings based on a representative population sample. Verhaltenstherapie 8:81–93
Livingston R, Martin-Cannici C (1985) Multiple somatic complaints and possible somatization disorder in prepubertal children. J Am Acad Child Adolesc Psychiatry 24:603–607
Murberg TA, Bru E (2004) School-related stress and psychomatic symptoms among Norwegian adolescents. Sch Psychol Int 25:317–332
Pennebaker JW (1982) The psychology of physical symptoms. Springer, Berlin
Rhee H (2005) Relationships between physical symptoms and pubertal development. J Pediatr Health Care 19:95–103
Roth-Isigkeit A, Thyen U, Stoeven H, Schwarzenberger J, Schmucker P (2005) Pain among children and adolescents: restrictions in daily living and triggering factors angela. Pediatrics 115:e152–e162
Sundblad GM, Saartok T, Engstroem LM (2006) Child–parent agreement on reports of disease, injury and pain. BMC Public Health 6:276. doi:10.1186/1471-2458-6-276.PMCID:PMC1654155
Takata Y, Sakata Y (2004) Development of a psychosomatic complaints scale for adolescents. Psychiatry Clin Neurosci 58:3–7
Tanaka H, Tamai H, Terashima S, Takenaka Y, Tanaka T (2000) Psychosocial factors affecting psychosomatic symptoms in Japanese schoolchildren. Pediatr Int 42:354–358
Taylor DC, Satzmari P, Boyle MH, Offord DR (1996) Somatization and the vocabulary of everyday bodily experiences and concerns: a community study of adolescents. J Am Acad Child Adolesc Psychiatry 35:491–499
Walker LS, Garber J, Greene JW (1991) Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol 19:379–394
Walker LS, Garber J, Smith CA, van Slyke DA, Claar R (2001) The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. J Consult Clin Psychol 69:85–91
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barkmann, C., Braehler, E., Schulte-Markwort, M. et al. Chronic somatic complaints in adolescents: prevalence, predictive validity of the parent reports, and associations with social class, health status, and psychosocial distress. Soc Psychiatry Psychiatr Epidemiol 46, 1003–1011 (2011). https://doi.org/10.1007/s00127-010-0273-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0273-4