Abstract
Aims/hypothesis
It is not known whether the early-pregnancy metabolome differs in patients with early- vs late-onset gestational diabetes mellitus (GDM) stratified by maternal overweight. The aims of this study were to analyse correlations between early-pregnancy metabolites and maternal glycaemic and anthropometric characteristics, and to identify early-pregnancy metabolomic alterations that characterise lean women (BMI <25 kg/m2) and women with overweight (BMI ≥25 kg/m2) with early-onset GDM (E-GDM) or late-onset GDM (L-GDM).
Methods
We performed a nested case–control study within the population-based prospective Early Diagnosis of Diabetes in Pregnancy cohort, comprising 210 participants with GDM (126 early-onset, 84 late-onset) and 209 normoglycaemic control participants matched according to maternal age, BMI class and primiparity. Maternal weight, height and waist circumference were measured at 8–14 weeks’ gestation. A 2 h 75 g OGTT was performed at 12–16 weeks’ gestation (OGTT1), and women with normal results underwent repeat testing at 24–28 weeks’ gestation (OGTT2). Comprehensive metabolomic profiling of fasting serum samples, collected at OGTT1, was performed by untargeted ultra-HPLC-MS. Linear models were applied to study correlations between early-pregnancy metabolites and maternal glucose concentrations during OGTT1, fasting insulin, HOMA-IR, BMI and waist circumference. Early-pregnancy metabolomic features for GDM subtypes (participants stratified by maternal overweight and gestational timepoint at GDM onset) were studied using linear and multivariate models. The false discovery rate was controlled using the Benjamini–Hochberg method.
Results
In the total cohort (n=419), the clearest correlation patterns were observed between (1) maternal glucose concentrations and long-chain fatty acids and medium- and long-chain acylcarnitines; (2) maternal BMI and/or waist circumference and long-chain fatty acids, medium- and long-chain acylcarnitines, phospholipids, and aromatic and branched-chain amino acids; and (3) HOMA-IR and/or fasting insulin and l-tyrosine, certain long-chain fatty acids and phospholipids (q<0.001). Univariate analyses of GDM subtypes revealed significant differences (q<0.05) for seven non-glucose metabolites only in overweight women with E-GDM compared with control participants: linolenic acid, oleic acid, docosapentaenoic acid, docosatetraenoic acid and lysophosphatidylcholine 20:4/0:0 abundances were higher, whereas levels of specific phosphatidylcholines (P-16:0/18:2 and 15:0/18:2) were lower. However, multivariate analyses exploring the early-pregnancy metabolome of GDM subtypes showed differential clustering of acylcarnitines and long-chain fatty acids between normal-weight and overweight women with E- and L-GDM.
Conclusions/interpretation
GDM subtypes show distinct early-pregnancy metabolomic features that correlate with maternal glycaemic and anthropometric characteristics. The patterns identified suggest early-pregnancy disturbances of maternal lipid metabolism, with most alterations observed in overweight women with E-GDM. Our findings highlight the importance of maternal adiposity as the primary target for prevention and treatment.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Gestational diabetes mellitus (GDM) is defined as hyperglycaemia detected for the first time during pregnancy [1], excluding overt diabetes. Increasing frequencies of up to 15% are seen internationally, paralleling the obesity epidemic [1, 2]. Both GDM and maternal obesity are associated with adverse short- and long-term health outcomes in the mothers and their offspring [1].
Recent evidence suggests that women with GDM display heterogeneity in terms of both pathophysiology and clinical outcomes [3, 4]. The dominant defect may be excess insulin resistance, insufficient insulin secretion, or both [5]. Other sources of heterogeneity are the presence or absence of maternal overweight [6] and the gestational timepoint at GDM onset [7]. Although, GDM is traditionally diagnosed in the latter half of gestation, increasing recognition is being given to the maternal metabolic environment as a central determinant of fetoplacental development from the time of conception [8]. Interestingly, a recent RCT showed that early treatment of women with GDM diagnosed at <20 weeks’ gestation improves neonatal outcomes [9].
Studies on type 2 diabetes, obesity and insulin resistance have revealed various typical metabolomic signatures [10, 11]. However, findings from metabolomic studies on GDM have been inconsistent [12, 13], possibly due to small sample sizes and lack of consideration of the confounding effects of maternal overweight [14,15,16] or other phenotypic differences between GDM subtypes [17]. Further, many studies collected maternal samples only in the second half of pregnancy, preventing examination of critical early-pregnancy metabolism. A recent study showed unique metabolomic and genetic patterns in insulin-deficient and insulin-resistant GDM subtypes in late pregnancy [18]. Whether the early-pregnancy metabolome differs in lean and overweight GDM subtypes, or depends on the gestational timepoint at GDM onset, remains unclear [7, 19].
The present study is a nested case–control study within the Finnish prospective, population-based Early Diagnosis of Diabetes in Pregnancy (EDDIE) cohort [20]. Using untargeted ultra-HPLC-MS, we aimed to analyse correlations between early-pregnancy metabolites and maternal glycaemic and anthropometric characteristics (fasting and post-load glucose concentrations, fasting insulin, HOMA-IR, maternal BMI and waist circumference [WC]) and to identify early-pregnancy metabolomic alterations that characterise normal-weight and overweight women with early-onset GDM (E-GDM) diagnosed at 12–16 weeks’ gestation or late-onset GDM (L-GDM) diagnosed at 24–28 weeks’ gestation.
Methods
Study participants and sample collection
The EDDIE cohort is a prospective, population-based cohort of 1605 pregnant women from South Karelia, Finland, between 2013 and 2016. Details of cohort formation have been published previously [20]. Briefly, 2305 pregnant women were asked to participate in the study during the first ultrasound screening appointment at South Karelia Central Hospital (Lappeenranta, Finland) or Honkaharju Hospital (Imatra, Finland) between 8 and 14 weeks’ gestation. Of these women, 527 (22.9%) declined to participate and 173 (7.5%) were excluded. Exclusion criteria were previously diagnosed type 1 or type 2 diabetes, use of a medication that affects glucose metabolism, such as corticosteroids, or the inability to understand the consent forms due to insufficient language skills. Although data on ethnicity was not collected, the Finnish population is relatively homogenous in terms of ethnicity, with most being of European descent.
Maternal height, weight and WC were measured, venous blood samples were drawn for HbA1c analysis, and information about pregnancy history and diabetes risk factors was collected using a structured questionnaire. All participants were referred for a 2 h 75 g OGTT between 12 and 16 weeks’ gestation (OGTT1). Additional fasting serum samples were collected at the time of the OGTT1.
GDM was diagnosed according to the Finnish Current Care Guidelines [21] if any of the following thresholds were met or exceeded: 0 h (fasting plasma) glucose ≥5.3 mmol/l, 1 h glucose ≥10.0 mmol/ or 2 h glucose ≥8.6 mmol/l. Participants who had a normal OGTT1 were referred for a repeat OGTT at 24–28 weeks’ gestation (OGTT2). The same diagnostic thresholds were used to diagnose E-GDM at OGTT1 and L-GDM at OGTT2 [21].
For the present case–control study, we initially selected all EDDIE participants with E-GDM or L-GDM for whom a fasting serum sample collected at OGTT1 was available. Women who reported smoking during pregnancy and those with thyroid, autoimmune or hypertensive disorders requiring medication were excluded due to potential effects on the early-pregnancy metabolome. In total, we identified 210 women with GDM who met the inclusion criteria: 126 women with E-GDM (abnormal OGTT1) and 84 women with L-GDM (normal OGTT1, abnormal OGTT2). Forty women were treated with insulin and/or metformin (29 women with E-GDM and 11 women with L-GDM). These women were matched with 210 control women (both OGTT1 and OGTT2 normal) according to age (±3 years), primiparity (yes/no) and BMI class (<18.5 kg/m2, 18.5–24.99 kg/m2, 25–29.99 kg/m2, 30–35.99 kg/m2, ≥40 kg/m2). The case–control matching function in SPSS Statistics 26.0 for Mac (IBM, USA) was used for matching of GDM patients and control participants.
Analysis of HbA1c, plasma glucose and serum insulin concentrations
HbA1c and plasma glucose concentrations during the OGTTs were analysed at the South Karelia Central Hospital Laboratory from fresh venous blood samples. Fasting serum insulin was analysed at Vita Laboratories (Helsinki, Finland) from serum samples collected at the time of OGTT1 and frozen at −80°C until analysis (see electronic supplementary material [ESM] Methods for further details).
Sample preparation and LC-MS analysis
Fasting serum samples, stored at −80°C until use, were analysed by Afekta Technologies (Kuopio, Finland) using LC-MS, comprising a Vanquish Flex UHPLC system (Thermo Scientific, Germany) coupled with a high-resolution Orbitrap mass spectrometer (Q Exactive Focus, Thermo Scientific). Sample preparation and the analytical methods are described in detail in the ESM Methods and in previous publications [22, 23]. In brief, a Zorbax Eclipse XDB-C18 column (2.1×100 mm, particle size 1.8 µm; Agilent Technologies, USA) was used for the reversed-phase separation, and an Aqcuity UPLC BEH amide column (Waters, USA) was used for the hydrophilic interaction liquid chromatography separation, combined with jet stream electrospray ionisation in both positive and negative modes. The samples were analysed in three batches comprising 154, 165 and 165 samples, including quality control samples. The same quality control samples were used in all batches to enable batch effect correction. One control sample was inadvertently omitted from the LC-MS analysis, resulting in a final sample of 209 control participants.
Data analysis
Analysis of clinical data
An unpaired, independent-sample Student’s t test, χ2 test and ANOVA were used to compare characteristics between the groups. In cases of violation of the normality assumptions, a permutation t test or a bootstrap-type method was applied. The significance of pairwise multiple comparisons was corrected using the Šídák method. The normality of variables was tested using the Shapiro–Wilk test. Insulin resistance was quantified using HOMA-IR [24]. The Stata 17 statistical package (StataCorp, USA) was used for the analyses.
Analysis of MS data
Peak detection and alignment were performed using MS-DIAL version 4.60 [25]. Minimum peak height was set at 250,000. The peaks were detected using the linear weighted moving-average algorithm. Peak alignment parameters included a retention time tolerance of 0.05 min and an m/z tolerance of 0.015 Da, with a requirement that the maximum signal be at least five times the mean of the solvent blank samples. Data preprocessing and clean-up steps included drift correction, low-quality feature flagging, imputation and batch effect correction using the notame package, version 0.06 [23]. Batch effects between the three batches were corrected using the batchCorr R package [26].
For univariate analyses, we used linear regression models fitted separately for each molecular feature. The feature levels (peak areas based on signal counts) were used as the dependent variable in all models. Models were run using OGTT1 plasma glucose concentrations, continuous BMI values, fasting insulin concentrations and WC as predictors. Additional models were run to evaluate the effects of GDM groups (control participants, E-GDM, L-GDM and total GDM groups) in the BMI categories (BMI <25 kg/m2 vs BMI ≥25 kg/m2). In multivariate analyses, a partial least-squares discriminant analysis (PLS-DA) model was applied in the MUVR R package (version 0.0.974, Chalmers University of Technology, Sweden) to identify metabolites that predict group differences. The statistical models are explained in detail in ESM Methods. The Benjamini–Hochberg method was used to control for the false discovery rate. Corrected p values (q values) <0.05 were considered significant. All metabolomic data analyses were performed using R version 3.6.3 (R Foundation, Austria) and notame version 0.0.6 [23].
Compound identification
The chromatographic and mass spectrometric characteristics (retention time, exact mass and MS/MS spectra) of the significantly different molecular features were compared with entries in an in-house standard library, publicly available databases and published literature. Annotation of each metabolite and the level of identification were made based on the recommendations of the Chemical Analysis Working Group Metabolomics Standards Initiative [27].
Ethical approval
All study participants provided written informed consent for the study. The study protocol was approved by the ethical committee of the Hospital District of Helsinki and Uusimaa (343/13/03/03/2012), with the latest amendment accepted on 13 November 2019 (HUS/1794/2016).
Results
Maternal and offspring characteristics in the total cohort
Maternal characteristics at the time of enrolment and basic offspring characteristics are summarised in Table 1. GDM and control participants were well-matched for age, maternal BMI and primiparity. Birthweight, fetal sex distribution and gestational age at birth were similar between the groups. In contrast, women with GDM had larger WC and higher BP, glucose concentrations at OGTT1, HbA1c levels, fasting insulin concentrations and HOMA-IR (all p values <0.05).
Overlapping and distinct early-pregnancy metabolomic alterations are observed in GDM and maternal overweight
Overall, 7259 good-quality molecular features were included in the statistical analyses after data preprocessing and clean-up. Initially we examined the entire cohort of 419 women to obtain an overview of the early-pregnancy metabolites that differ between GDM/non-GDM participants and overweight or normal-weight participants.
GDM vs control women
First, we compared all women diagnosed with GDM, regardless of BMI and time of GDM onset, with matched control participants (Fig. 1a). Several long-chain fatty acids, medium- and long-chain acylcarnitines (ACar), a few lysophosphatidylcholines (lysoPCs) and phenylalanyltryptophan (Phe-Trp, a dipeptide formed from l-phenylalanine and l-tryptophan residues) were identified as present in higher abundance in GDM women compared with control participants (q<0.05). In contrast, a few phosphatidylcholine (PC) species were present in lower abundance.
Volcano plots showing differential metabolites associated with (a) GDM (regardless of BMI and time of GDM onset) compared with matched control participants without GDM and (b) maternal overweight in women without GDM compared with normal-weight control participants without GDM. Identified metabolites with statistically significant alterations in abundance are labelled by colour according to group: long-chain fatty acids (orange), acylcarnitines (red), derivatives of phospholipids (blue), carbohydrates (brown) and amino acids (purple). Grey dots indicate unidentified metabolites. The dashed line indicates level of significance (q value <0.05). PS, phosphatidylserine; SM, sphingomyelin
Overweight vs normal-weight control participants
Next we compared overweight and normal-weight control participants without GDM (Fig. 1b). The abundances of long-chain fatty acids, e.g. docosatetraenoic acid (FA C22:4) and oleic acid, medium- and long-chain ACar, lysoPCs, Phe-Trp and sphingomyelin d32:2 were increased, and that of certain PCs and phosphatidylserine O-20:0/0:0 was decreased, in overweight control participants vs normal-weight control participants (q<0.05).
Maternal glycaemic and anthropometric traits correlate with early-pregnancy lipid, acylcarnitine and amino acid metabolites
As overlapping metabolomic alterations were detected in GDM and maternal overweight, we continued our analyses by exploring correlations between maternal glycaemic and anthropometric variables and early-pregnancy metabolites. The heatmap in Fig. 2 demonstrates the direction, strength and statistical significance of Pearson correlations between detected metabolites and (1) glucose concentrations during OGTT1 at 12–16 weeks’ gestation; (2) maternal BMI and WC; and (3) fasting insulin concentrations and HOMA-IR, in the entire cohort. We observed the correlations described below, with a correlation coefficient greater than 0.2 and a q value <0.001.
Heatmaps illustrating the clustering and correlations of annotated early-pregnancy metabolites with maternal plasma glucose concentrations (fasting, 1 h and 2 h post-load plasma glucose during an OGTT at 12–16 weeks’ gestation on a continuous scale), maternal BMI and WC, and maternal fasting serum insulin and HOMA-IR. The level of significance is indicated with differently shaped symbols (circles, triangles, stars) . 5-AVAB, 5-Aminovaleric acid betaine; DG, diacylglycerol; DHEA-S, dehydroepiandrosterone sulfate; FAHFA, fatty acid ester of hydroxy fatty acid; HETE, hydroxyeicosatetraenoic acid; 7-HOCA, 7α-hydroxy-3-oxo-4-cholestenoic acid; LysoPE, lysophosphatidyl ethanolamine; MG, monoglyceride; PE, phosphatidyl ethanolamine PS, phosphatidylserine; SM, sphingomyelin
Fasting glucose concentrations
Fasting plasma glucose at OGTT1 correlated moderately only with a few metabolites, e.g. docosatetraenoic acid (FA C22:4) and oleic acid.
Post-load glucose concentrations
Glucose concentrations 1 h and 2 h post-load correlated most strongly with docosatetraenoic acid and oleic acid, and these correlations were stronger than those observed for fasting plasma glucose. Post-load glucose concentrations, particularly the 2 h glucose value, also correlated with other long-chain fatty acids. Weaker but statistically significant correlations were found between 1 h and/or 2 h post-load glucose concentrations and medium and long-chain ACar, Phe-Trp, certain cholesterol metabolites (7α-hydroxy-3-oxo-4-cholestenoic acid and 7-ketocholesterol [sterol C27H44O22]), diacylglycerol 16:1/18:1, and specific phospholipids (PC 16:0/20:4, PC 32:1 and lysoPC 20:3/0:0).
Maternal BMI and WC
BMI and WC correlated with long-chain fatty acids and ACar, particularly with docosatetraenoic acid, oleic acid, and ACar 6:0, 12:1 and 16:1. Sphingomyelin d32:2 showed a stronger correlation with maternal BMI, whereas the aromatic amino acids (AAA) l-tyrosine and phenylalanine correlated most strongly with maternal WC. In addition, BMI and WC correlated positively with branched-chain amino acids (BCAA) and other amino acids, Phe-Trp, certain cholesterol metabolites and lysoPCs 16:1, 16:1/0:0, 0:0/16:1 and 20:3/0:0, and negatively with certain PCs, lysoPC 20:0 and phosphatidylserine O-20:0/0:0.
Fasting insulin and HOMA-IR
HOMA-IR correlated most strongly with l-tyrosine. A weaker correlation was observed between fasting insulin and l-tyrosine. Weaker correlations were also seen between both parameters of insulin resistance and β-alanine, Phe-Trp, diacylglycerol 16:1/18:1 and docosatetraenoic acid. HOMA-IR also correlated with myristic acid, oleic acid, lysoPCs 20:3/0:0 and 16:1. LysoPC 20:0 and PC 40:8 correlated negatively with both HOMA-IR and fasting insulin.
Maternal and offspring characteristics in GDM subtypes
For the analysis of the early-pregnancy metabolome in GDM subtypes, we stratified our study participants by the time of GDM onset and maternal overweight. Table 2 compares maternal background characteristics in normal-weight and overweight E-GDM, L-GDM and control women.
BMI <25 kg/m2
Normal-weight women with GDM had higher glucose concentrations at all time points of OGTT1 (fasting, 1 h and 2 h glucose) and higher fasting insulin concentrations than control participants (all p<0.05). Those with E-GDM had higher HOMA-IR compared with L-GDM and control participants (both p<0.05). Women with L-GDM had higher early-pregnancy BP and larger WCs compared with normal-weight control participants (both p<0.05). Basic offspring characteristics did not differ between the groups.
BMI ≥25 kg/m2
As expected, overweight women with E-GDM had higher glucose concentrations at all time points of OGTT1 than overweight L-GDM and control women (all p<0.001). HbA1c levels were also higher in overweight women with GDM vs control participants (p<0.001). Differences in fasting insulin, maternal WC and HOMA-IR were observed only between overweight E-GDM women and control participants (all p<0.001). Maternal early-pregnancy BP and basic offspring characteristics did not differ between the groups.
Alterations in early-pregnancy lipid metabolism characterise overweight women with gestational diabetes
Univariate linear models revealed 162 identified or putatively annotated metabolites that had differential mean abundances between normal-weight and overweight women with E-GDM or L-GDM compared with control participants (raw p value <0.05) (ESM Table 1). Eight metabolites reached a q value <0.05 (glucose, lysoPC 20:4/0:0, lysoPC 20:3/0:0, PC P–16:0/18:2, PC 15:0/18:2, PC 16:0/20:3, linolenic acid, linoleic acid, oleic acid, docosapentaenoic acid [FA C22:5] and docosatetraenoic acid [FA C22:4]). In volcano plot analyses comparing early-pregnancy metabolites in women with E-GDM and L-GDM stratified by BMI, glucose was present in higher abundance in women with E-GDM regardless of BMI (Fig. 3a,b). All significantly differing non-glucose metabolites were detected in overweight women with E-GDM (Fig. 3b). Most metabolites were detected in higher abundance, although metabolites with lower abundances were also observed (e.g. PC P-16:0/18:2 and PC 15:0/18:2). Volcano plot analyses did not reveal statistically significant differences in the early-pregnancy metabolome of normal-weight women with L-GDM vs normal-weight control participants (Fig. 3c), or between overweight women with L-GDM vs overweight control participants (Fig. 3d).
Volcano plots showing differential metabolites associated with (a) E-GDM in normal-weight individuals (BMI <25 kg/m2) vs normal-weight control participants, (b) E-GDM in overweight individuals (BMI ≥25 kg/m2) vs overweight control participants, (c) L-GDM in normal-weight individuals vs normal-weight control participants, and (d) L-GDM in overweight individuals vs overweight control participants. Identified metabolites are labelled by colour according to main metabolite group: long-chain fatty acids (orange), acylcarnitines (red), derivatives of phospholipids (blue), carbohydrates (brown) and amino acids (purple) and those with statistically significant alterations in abundance are named. Grey dots indicate unidentified metabolites. The dashed line in (a) and (b) indicates the level of significance (q<0.05)
The box plots in Fig. 4 show metabolites with statistically significant differential abundance in either E-GDM or L-GDM vs control participants or in the total GDM group vs control participants, stratified by overweight. Further details are shown in ESM Tables 2–9. Differential abundances of non-glucose metabolites were observed only for lipid metabolites in overweight women. Glucose was detected in higher abundance in E-GDM participants (both normal-weight and overweight) (both q<0.05).
Box plots of significantly differential PCs, lysoPCs and long-chain fatty acids in comparisons of E-GDM and L-GDM vs control participants for normal-weight individuals (BMI <25 kg/m2) and overweight individuals (BMI ≥25 kg/m2). E-GDM, normal weight: n=39; L-GDM, normal weight: n=37; control participants, normal weight: n=76; E-GDM, overweight: n=87; L-GDM, overweight: n=47; control participants, overweight: n=134. Brackets indicate statistically significant differences between two groups; combined brackets indicate statistically significant differences between a combined group and control participants. Asterisks indicate significant differences for the comparisons between the subgroups: *q<0.05, **q<0.01, ***q<0.001
BMI ≥25 kg/m2
PC P-16:0/18:2 and PC 15:0/18:2 were detected in lower abundance in E-GDM women compared with BMI-matched control participants (q<0.01 and q<0.05, respectively). PC 16:0/20:3 was detected in lower abundance in the total GDM group (q<0.05). In contrast, lysoPC 20:4/0:0 was increased in the E-GDM subgroup and lysoPC (20:3/0:0) was increased in the total GDM group (both q<0.05). Linolenic acid, docosapentaenoic acid (FA C22:5), oleic acid and docosatetraenoic acid (FA C22:4) abundances were increased in the E-GDM group (q<0.05, q<0.05, q<0.05 and q<0.01, respectively). Further, oleic acid and docosatetraenoic acid (FA C22:4) showed higher abundances in overweight control participants compared with normal-weight control participants (both q<0.05). Linoleic acid was increased in overweight women in the total GDM group vs overweight control participants (q<0.05).
Early-pregnancy metabolic fingerprints of GDM subtypes
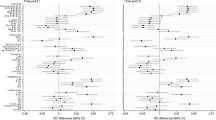
Finally, we applied a multivariate PLS-DA model to explore early-pregnancy metabolite patterns or ‘metabolic fingerprints’ that best differentiate GDM groups (ESM Tables 10–17). Metabolites that predict differences between normal-weight and overweight women with E-GDM or L-GDM vs control participants are shown in Fig. 5. The clearest patterns showed clustering of medium- and long-chain ACar in normal-weight women with E-GDM or L-GDM (Fig. 5a) and overweight women with E-GDM (Fig. 5b), and clustering of long-chain fatty acids and phospholipids in normal-weight women with E-GDM (Fig. 5a) and overweight women with E-GDM or L-GDM (Fig. 5b).
Venn diagrams of metabolites included in PLS-DA models that discriminate E-GDM and L-GDM patients from control participants for both normal-weight (a) and overweight (b) women. Subgroup-specific AUC estimates are reported for the best-fitting models. 5-AVAB, 5-aminovaleric acid betaine; DG, diacylglycerol; HETE, hydroxyeicosatetraenoic acid; MG, monoglyceride; PE, phosphatidyl ethanolamine
Discussion
The results of our nested case–control study within the Finnish population-based EDDIE cohort demonstrate that the maternal early-pregnancy metabolome differs in early- and late-onset GDM subtypes and is significantly modified by maternal overweight. At 12–16 weeks’ gestation, the clearest correlation patterns were detected between (1) maternal OGTT glucose concentrations and long-chain fatty acids and ACar, (2) maternal adiposity and long-chain fatty acids, phospholipids, ACar, AAA, BCAA and other amino acids, and (3) indicators of insulin resistance and l-tyrosine, specific long-chain fatty acids and phospholipids. All the differential non-glucose metabolites identified in univariate analyses comparing GDM subtypes were lipid metabolites in women with overweight and GDM, with most alterations detected in long-chain fatty acids and phospholipids in E-GDM. Univariate analyses did not identify statistically significant differences in non-glucose metabolites between normal-weight women with E-GDM or L-GDM vs control participants. However, multivariate analyses comparing the ‘metabolomic fingerprints’ of GDM subgroups vs control participants suggested differences in ACar in normal-weight GDM women and long-chain fatty acids in women with overweight and GDM, regardless of time of GDM onset. E-GDM subtypes in both normal-weight and overweight women showed differences in both ACar and long-chain fatty acids.
To our knowledge, this is the first study to analyse associations between early-pregnancy metabolites and maternal glycaemic and anthropometric traits, and to identify early-pregnancy metabolomic differences between participants with E-GDM and L-GDM, stratified by maternal overweight. Access to the large, population-based EDDIE cohort enabled selection of participants from a mixed ‘real-world’ pool of low- and high-risk pregnant women and the matching of GDM and control participants. All OGTTs were performed in the same laboratory, using standard test protocols [20]. Many previous metabolomic studies have exploited targeted methods, but we used unbiased high-performance LC-MS/MS, enabling wide-scale screening of differential metabolites. One limitation of our study is that the unselected EDDIE cohort included few severely obese participants, which prevented us from studying the various classes of obesity separately. Moreover, although our sample size is more robust than in most previous untargeted LC-MS/MS studies on GDM, a larger sample size would probably enable the detection of more subtle early-pregnancy alterations in GDM subgroups, such as normal-weight women with GDM. The use of an ethnically homogenous study population may also affect the generalisability of our results.
Few previous metabolomic studies have considered the heterogeneity of GDM [17]. A Finnish study using NMR spectroscopy reported metabolomic changes across gestation in obese women with GDM, obese women without GDM and non-obese women with GDM compared with non-obesed women without GDM [28]. However, only women from high-risk obstetric cohorts were included, and metabolomic differences between E-GDM and L-GDM were not explored [28]. Similarly, Lee et al demonstrated differences in the metabolomic and genetic architecture between insulin-sensitive vs insulin-resistant L-GDM subtypes; however, in their study, blood samples were collected at approximately 28 weeks’ gestation [18].
Metabolomic changes involving BCAA and AAA characterise obesity, insulin resistance and type 2 diabetes in non-pregnant individuals [10, 11, 29]. Findings in pregnant women have been inconsistent [30]. Increased levels of BCAA in early pregnancy have been reported in obese women [15] and lean women [31] who develop L-GDM. In contrast, a targeted metabolomics study performed in the first trimester did not observe BCAA differences between women with L-GDM and control participants [32]. Another recent study found that BCAA and AAA concentrations at 15–26 weeks’ gestation, but not at 10–14 weeks’ gestation, were positively associated with L-GDM risk [33]. Similarly, we did not discover significant differences in early-pregnancy BCAA or AAA between E-GDM women or L-GDM women vs control participants in univariate analyses. However, maternal BMI and/or WC correlated positively with AAA (tyrosine and phenylalanine) and BCAA (leucine and valine), and HOMA-IR and fasting insulin correlated with l-tyrosine. Moreover, in PLS-DA models, l-leucine and l-phenylalanine were observed to be differential metabolites in normal-weight women with L-GDM, and l-tyrosine was a differential metabolite in overweight women with E-GDM. Previous studies have also linked these amino acids to insulin resistance in early pregnancy [34] and late pregnancy [18, 35], and to L-GDM in obese women [15].
Exaggerated late-pregnancy dyslipidaemia and alterations in maternal, placental and fetal fatty acid metabolism have been reported in GDM and in pregnancies in women with obesity [15, 36]. Data on lipid metabolism in early pregnancy are less abundant. We observed increased early-pregnancy levels of several long-chain fatty acids, e.g. oleic acid, docosapentaenoic acid, docosatetraenoic acid, and linolenic acid, particularly in women with E-GDM. These fatty acids correlated most strongly with post-load glucose concentrations, maternal BMI and WC, and emerged as differential metabolites characterising the early-pregnancy metabolomic profiles of women with E-GDM and overweight GDM vs control participants. These results agree with studies showing elevated levels of long-chain fatty acids, such as oleic acid and linoleic acid, in non-pregnant obese adults [37] and in early pregnancy in women who develop L-GDM [38]. Elevated docosapentaenoic acid levels, on the other hand, have been previously associated with reduced L-GDM risk when measured in early pregnancy [39], although an increased risk of the metabolic syndrome has been reported in non-pregnant individuals [40].
Both obesity and diabetes are associated with derangements of sphingolipid, phospholipid and lysolipid pathways [41]. The association of sphingomyelin d32:2 with maternal overweight in early pregnancy and its correlation with maternal BMI in our cohort confirm earlier findings [34]. Our observations of reduced early-pregnancy abundance of various PC species in overweight and/or GDM women, and the negative correlations of several PC species with BMI and WC, are also in concordance with the results of previous studies [14, 42]. Regarding lysoPCs, studies in non-pregnant individuals have shown reduced levels in relation to obesity [37, 43] and type 2 diabetes [11, 43]. Studies in lean pregnant women [44, 45] and obese pregnant women [42] have yielded less consistent results, suggesting both positive and negative associations between levels of lysoPC species in early pregnancy and L-GDM. In agreement with this, we observed negative correlations between lysoPC 20:0 and maternal BMI and WC, but positive correlations between lysoPC 16:1 and parameters of adiposity and insulin resistance. Moreover, higher abundances of lysoPC 20:4/0:0 were identified in overweight women with E-GDM, whereas lysoPC 20:3/0:0 showed higher abundance among overweight women in the total GDM group in univariate analyses and correlated with post-load glucose, maternal WC and HOMA-IR. Hence, our findings support the involvement of lysoPCs in the metabolomic alterations of early pregnancy that characterise E-GDM and perhaps also L-GDM, but the gestational timepoint and maternal BMI may influence species-specific directions of associations.
Short- and long-chain ACar are associated with type 2 diabetes risk [10, 11]. While short-chain ACar are linked to BCAA catabolism, long-chain ACar may result from incomplete fatty acid oxidation, contributing to insulin resistance [46]. A longitudinal cohort study reported associations between increased levels of medium-chain ACar (C14:1-OH) at 10–14 weeks’ gestation and L-GDM [46]. Likewise, in our whole cohort, medium- and long-chain ACar were elevated in GDM and overweight women, and correlated positively with post-load glucose, maternal BMI and WC. Although we did not observe differences in ACar between GDM subgroups in univariate analyses, ACar emerged as differential metabolites in normal-weight women with E-GDM and L-GDM, and in overweight women with E-GDM, in multivariate PLS-DA models. This finding is interesting given that Lee et al reported that several ACar in late pregnancy were associated with insulin-deficient GDM [18].
We observed the most extensive metabolomic perturbations in overweight women with E-GDM, in accordance with reports showing high risks of perinatal complications in insulin-resistant [4], early-onset [7] and overweight [6, 47] GDM subtypes. In contrast, our data suggest fewer early-pregnancy metabolomic differences between overweight women with L-GDM vs overweight control participants, as supported by the lowest AUC value in the PLS-DA model. For normal-weight women with GDM, we were surprised that only glucose emerged as an altered metabolite in E-GDM women vs control participants, and that the metabolome of L-GDM women did not statistically significantly differ from that of BMI-matched control participants at 12–16 weeks’ gestation in univariate analyses. It is plausible that, in lean women with GDM, genetic risk factors and beta cell dysfunction play a greater pathogenetic role than chronic insulin resistance. Although most known GDM risk alleles identified are variants that associate with beta cell function, a recent genome-wide association study reported genetic risk alleles for GDM in central glucose homeostasis, steroidogenesis and placental expression [48]. It is noteworthy that, in our study, normal-weight women with E-GDM showed elevated fasting insulin concentrations and HOMA-IR compared with normal-weight and overweight normoglycaemic control participants, suggesting some degree of early-pregnancy insulin resistance. This is in line with previous observations indicating deficient first-trimester beta cell function and substantial reduction in early-pregnancy insulin sensitivity in women with E-GDM [49].
In conclusion, our untargeted LC-MS metabolomic analyses revealed specific early-pregnancy metabolome differences between lean and overweight women with E-GDM and L-GDM. Most metabolomic alterations were detected in overweight women with E-GDM and involved lipid metabolites that correlated with post-glucose concentrations, maternal BMI and WC, underscoring the importance of maternal pre-conception weight management.
Abbreviations
- ACar:
-
Acylcarnitine(s)
- AAA:
-
Aromatic amino acids
- BCAA:
-
Branched-chain amino acids
- EDDIE:
-
Early diagnosis of diabetes in pregnancy
- E-GDM:
-
Early gestational diabetes mellitus
- FA:
-
Fatty acid
- GDM:
-
Gestational diabetes mellitus
- L-GDM:
-
Late gestational diabetes mellitus
- LysoPC:
-
Lysophosphatidylcholine
- PC:
-
Phosphatidylcholine
- Phe-Trp:
-
Phenylalanyltryptophan
- WC:
-
Waist circumference
References
Sweeting A, Wong J, Murphy HR, Ross GP (2022) A clinical update on gestational diabetes mellitus. Endocr Rev 43(5):763–793. https://doi.org/10.1210/endrev/bnac003
Saeedi M, Cao Y, Fadl H, Gustafson H, Simmons D (2021) Increasing prevalence of gestational diabetes mellitus when implementing the IADPSG criteria: a systematic review and meta-analysis. Diabetes Res Clin Pract 172:108642. https://doi.org/10.1016/j.diabres.2020.108642
Powe CE, Hivert MF, Udler MS (2020) Defining heterogeneity among women with gestational diabetes mellitus. Diabetes 69(10):2064–2074. https://doi.org/10.2337/dbi20-0004
Benhalima K, Van Crombrugge P, Moyson C et al (2019) Characteristics and pregnancy outcomes across gestational diabetes mellitus subtypes based on insulin resistance. Diabetologia 62(11):2118–2128. https://doi.org/10.1007/s00125-019-4961-7
Powe CE, Allard C, Battista MC et al (2016) Heterogeneous contribution of insulin sensitivity and secretion defects to gestational diabetes mellitus. Diabetes Care 39(6):1052–1055. https://doi.org/10.2337/dc15-2672
Ijas H, Koivunen S, Raudaskoski T, Kajantie E, Gissler M, Vaarasmaki M (2019) Independent and concomitant associations of gestational diabetes and maternal obesity to perinatal outcome: a register-based study. PLoS One 14(8):e0221549. https://doi.org/10.1371/journal.pone.0221549
Immanuel J, Simmons D (2017) Screening and treatment for early-onset gestational diabetes mellitus: a systematic review and meta-analysis. Curr Diab Rep 17(11):115. https://doi.org/10.1007/s11892-017-0943-7
Desoye G (2018) The human placenta in diabetes and obesity: friend or foe? The 2017 Norbert Freinkel Award Lecture. Diabetes Care 41(7):1362–1369. https://doi.org/10.2337/dci17-0045
Simmons D, Immanuel J, Hague WM et al (2023) Treatment of gestational diabetes mellitus diagnosed early in pregnancy. N Engl J Med 388(23):2132–2144. https://doi.org/10.1056/NEJMoa2214956
Guasch-Ferre M, Hruby A, Toledo E et al (2016) Metabolomics in prediabetes and diabetes: a systematic review and meta-analysis. Diabetes Care 39(5):833–846. https://doi.org/10.2337/dc15-2251
Morze J, Wittenbecher C, Schwingshackl L et al (2022) Metabolomics and type 2 diabetes risk: an updated systematic review and meta-analysis of prospective cohort studies. Diabetes Care 45(4):1013–1024. https://doi.org/10.2337/dc21-1705
Alesi S, Ghelani D, Rassie K, Mousa A (2021) Metabolomic biomarkers in gestational diabetes mellitus: a review of the evidence. Int J Mol Sci 22(11):5512. https://doi.org/10.3390/ijms22115512
Wang QY, You LH, Xiang LL, Zhu YT, Zeng Y (2021) Current progress in metabolomics of gestational diabetes mellitus. World J Diabetes 12(8):1164–1186. https://doi.org/10.4239/wjd.v12.i8.1164
Shokry E, Marchioro L, Uhl O et al (2019) Impact of maternal BMI and gestational diabetes mellitus on maternal and cord blood metabolome: results from the PREOBE cohort study. Acta Diabetol 56(4):421–430. https://doi.org/10.1007/s00592-019-01291-z
White SL, Pasupathy D, Sattar N et al (2017) Metabolic profiling of gestational diabetes in obese women during pregnancy. Diabetologia 60(10):1903–1912. https://doi.org/10.1007/s00125-017-4380-6
Mokkala K, Vahlberg T, Pellonperä O, Houttu N, Koivuniemi E, Laitinen K (2020) Distinct metabolic profile in early pregnancy of overweight and obese women developing gestational diabetes. J Nutr 150(1):31–37. https://doi.org/10.1093/jn/nxz220
Zhang M, Yang H (2022) Perspectives from metabolomics in the early diagnosis and prognosis of gestational diabetes mellitus. Front Endocrinol (Lausanne) 13:967191. https://doi.org/10.3389/fendo.2022.967191
Lee K, Kuang A, Bain JR et al (2024) Metabolomic and genetic architecture of gestational diabetes subtypes. Diabetologia 67:895–907. https://doi.org/10.1007/s00125-024-06110-x
Wexler DJ, Powe CE, Barbour LA et al (2018) Research gaps in gestational diabetes mellitus: executive summary of a National Institute of Diabetes and Digestive and Kidney Diseases workshop. Obstet Gynecol 132(2):496–505. https://doi.org/10.1097/aog.0000000000002726
Jokelainen M, Stach-Lempinen B, Rönö K et al (2020) Oral glucose tolerance test results in early pregnancy: a Finnish population-based cohort study. Diabetes Res Clin Pract 162:108077. https://doi.org/10.1016/j.diabres.2020.108077
Finnish Medical Society Duodecim Working Group (2013) Update on current care guidelines: gestational diabetes. Duodecim 129(17): 1798-1799 [article in Finnish]
Hanhineva K, Lankinen MA, Pedret A et al (2015) Nontargeted metabolite profiling discriminates diet-specific biomarkers for consumption of whole grains, fatty fish, and bilberries in a randomized controlled trial. J Nutr 145(1):7–17. https://doi.org/10.3945/jn.114.196840
Klåvus A, Kokla M, Noerman S et al (2020) ‘notame’: workflow for non-targeted LC-MS metabolic profiling. Metabolites 10(4):135. https://doi.org/10.3390/metabo10040135
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419. https://doi.org/10.1007/bf00280883
Tsugawa H, Cajka T, Kind T et al (2015) MS-DIAL: data-independent MS/MS deconvolution for comprehensive metabolome analysis. Nature Methods 12(6):523–526. https://doi.org/10.1038/nmeth.3393
Brunius C, Shi L, Landberg R (2016) Large-scale untargeted LC-MS metabolomics data correction using between-batch feature alignment and cluster-based within-batch signal intensity drift correction. Metabolomics 12(11):173. https://doi.org/10.1007/s11306-016-1124-4
Sumner LW, Amberg A, Barrett D et al (2007) Proposed minimum reporting standards for chemical analysis: Chemical Analysis Working Group (CAWG) Metabolomics Standards Initiative (MSI). Metabolomics 3(3):211–221. https://doi.org/10.1007/s11306-007-0082-2
Sormunen-Harju H, Huvinen E, Girchenko PV et al (2023) Metabolomic profiles of nonobese and obese women with gestational diabetes. J Clin Endocrinol Metab 108(11):2862–2870. https://doi.org/10.1210/clinem/dgad288
Rangel-Huerta OD, Pastor-Villaescusa B, Gil A (2019) Are we close to defining a metabolomic signature of human obesity? A systematic review of metabolomics studies. Metabolomics 15(6):93. https://doi.org/10.1007/s11306-019-1553-y
Huynh J, Xiong G, Bentley-Lewis R (2014) A systematic review of metabolite profiling in gestational diabetes mellitus. Diabetologia 57(12):2453–2464. https://doi.org/10.1007/s00125-014-3371-0
Li N, Li J, Wang H et al (2022) Branched-chain amino acids and their interactions with lipid metabolites for increased risk of gestational diabetes. J Clin Endocrinol Metab 107(7):e3058–e3065. https://doi.org/10.1210/clinem/dgac141
Bentley-Lewis R, Huynh J, Xiong G et al (2015) Metabolomic profiling in the prediction of gestational diabetes mellitus. Diabetologia 58(6):1329–1332. https://doi.org/10.1007/s00125-015-3553-4
Yang J, Wu J, Tekola-Ayele F et al (2023) Plasma amino acids in early pregnancy and midpregnancy and their interplay with phospholipid fatty acids in association with the risk of gestational diabetes mellitus: results from a longitudinal prospective cohort. Diabetes Care 46(4):722–732. https://doi.org/10.2337/dc22-1892
Hellmuth C, Lindsay KL, Uhl O et al (2017) Association of maternal prepregnancy BMI with metabolomic profile across gestation. Int J Obes 41(1):159–169. https://doi.org/10.1038/ijo.2016.153
Liu Y, Kuang A, Talbot O et al (2020) Metabolomic and genetic associations with insulin resistance in pregnancy. Diabetologia 63(9):1783–1795. https://doi.org/10.1007/s00125-020-05198-1
Herrera E, Desoye G (2016) Maternal and fetal lipid metabolism under normal and gestational diabetic conditions. Horm Mol Biol Clin Investig 26(2):109–127. https://doi.org/10.1515/hmbci-2015-0025
Park S, Sadanala KC, Kim EK (2015) A metabolomic approach to understanding the metabolic link between obesity and diabetes. Mol Cells 38(7):587–596. https://doi.org/10.14348/molcells.2015.0126
Enquobahrie DA, Denis M, Tadesse MG, Gelaye B, Ressom HW, Williams MA (2015) Maternal early pregnancy serum metabolites and risk of gestational diabetes mellitus. J Clin Endocrinol Metab 100(11):4348–4356. https://doi.org/10.1210/jc.2015-2862
Zhu Y, Li M, Rahman ML et al (2019) Plasma phospholipid n-3 and n-6 polyunsaturated fatty acids in relation to cardiometabolic markers and gestational diabetes: a longitudinal study within the prospective NICHD Fetal Growth Studies. PLoS Med 16(9):e1002910. https://doi.org/10.1371/journal.pmed.1002910
Wu Q, Li J, Sun X et al (2021) Multi-stage metabolomics and genetic analyses identified metabolite biomarkers of metabolic syndrome and their genetic determinants. eBioMedicine 74:103707. https://doi.org/10.1016/j.ebiom.2021.103707
Yousri NA, Suhre K, Yassin E et al (2022) Metabolic and metabo-clinical signatures of type 2 diabetes, obesity, retinopathy, and dyslipidemia. Diabetes 71(2):184–205. https://doi.org/10.2337/db21-0490
Barber MN, Risis S, Yang C et al (2012) Plasma lysophosphatidylcholine levels are reduced in obesity and type 2 diabetes. PLoS One 7(7):e41456. https://doi.org/10.1371/journal.pone.0041456
Wang Y, Wu P, Huang Y et al (2022) BMI and lipidomic biomarkers with risk of gestational diabetes in pregnant women. Obesity (Silver Spring) 30(10):2044–2054. https://doi.org/10.1002/oby.23517
Liu J, Li J, Li S et al (2020) Circulating lysophosphatidylcholines in early pregnancy and risk of gestational diabetes in Chinese women. J Clin Endocrinol Metab 105(4):dgaa058. https://doi.org/10.1210/clinem/dgaa058
Furse S, White SL, Meek CL et al (2019) Altered triglyceride and phospholipid metabolism predates the diagnosis of gestational diabetes in obese pregnancy. Mol Omics 15(6):420–430. https://doi.org/10.1039/c9mo00117d
Lin Y, Wu J, Zhu Y et al (2021) A longitudinal study of plasma acylcarnitines throughout pregnancy and associations with risk of gestational diabetes mellitus. Clin Nutr 40(8):4863–4870. https://doi.org/10.1016/j.clnu.2021.07.008
Sovio U, Murphy HR, Smith GC (2016) Accelerated fetal growth prior to diagnosis of gestational diabetes mellitus: a prospective cohort study of nulliparous women. Diabetes Care 39(6):982–987. https://doi.org/10.2337/dc16-0160
Elliott A, Walters RK, Pirinen M et al (2024) Distinct and shared genetic architectures of gestational diabetes mellitus and type 2 diabetes mellitus. Nat Genet 56:377–382. https://doi.org/10.1038/s41588-023-01607-4
Thaweethai T, Soetan Z, James K, Florez JC, Powe CE (2023) Distinct insulin physiology trajectories in euglycemic pregnancy and gestational diabetes mellitus. Diabetes Care 46(12):2137–2146. https://doi.org/10.2337/dc22-2226
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Acknowledgements
Research nurses Sirpa Valpas (South Karelia Central Hospital) and Pirjo Munnukka (Honkaharju Hospital) are acknowledged for recruiting all participants and collecting data. The doctors Mervi Jokelainen, Beata Stach-Lempinen, Tero Tapiola, Antti Sotka, Ulla Pikarinen and Antti Valpas, in addition to Arja Nenonen, Arja Heikkinen, midwives and other personnel working at the South Karelia Central Hospital antenatal outpatient clinic, labour ward, operating theatres, laboratory and research administration, also provided crucial input and assistance in the implementation of this study. Data scientist Atte Lihtamo (Afekta Technologies Ltd) is thanked for his collaboration and contributions in the copy-editing phase.
Data availability
The data that support the findings of this study are not openly available for reasons of sensitivity, but may be available from the corresponding author upon reasonable request.
Funding
Open Access funding provided by University of Helsinki (including Helsinki University Central Hospital). This work was supported by the Research Foundation of South Karelia Central Hospital, the Viipuri Tuberculosis Foundation, Finnish State Funding for University-Level Health Research, the Päivikki and Sakari Sohlberg Foundation, the Diabetes Research Foundation and the Juho Vainio Foundation. Additionally, individual researchers received grants from the Viipuri Tuberculosis Foundation (MMK and SM), the Päivikki and Sakari Sohlberg Foundation (MMK and SM), South Karelia Medical Association (MMK), the Finnish Medical Foundation (MMK), the Maud Kuistila Memorial Foundation (MMK), the Research Foundation for Obstetrics and Gynecology (MMK), Biomedicum Helsinki Research Foundation (MMK), the Finnish Cultural Foundation (MMK), the Jalmari and Rauha Ahokas Foundation (MMK) and the Paulo Foundation (KR).
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
MMK initiated the population-based EDDIE study. This nested case–control study was planned by MMK, TJJ and KR. Metabolomics analyses were planned and implemented in collaboration with OK, AK and VK. KR was responsible for clinical data management and analysis. All authors participated in the planning of statistical analyses and interpretation of metabolomics data. SM and MMK wrote the manuscript. All authors contributed toward critically revising the paper, which was accepted by all authors. MMK is the guarantor of this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Masalin, S., Klåvus, A., Rönö, K. et al. Analysis of early-pregnancy metabolome in early- and late-onset gestational diabetes reveals distinct associations with maternal overweight. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06237-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00125-024-06237-x