Abstract
The increasing incidence of type 2 diabetes, which represents 90% of diabetes cases globally, is a major public health concern. Improved glucose management reduces the risk of vascular complications and mortality; however, only a small proportion of the type 2 diabetes population have blood glucose levels within the recommended treatment targets. In recent years, diabetes technologies have revolutionised the care of people with type 1 diabetes, and it is becoming increasingly evident that people with type 2 diabetes can also benefit from these advances. In this review, we describe the current knowledge regarding the role of technologies for people living with type 2 diabetes and the evidence supporting their use in clinical practice. We conclude that continuous glucose monitoring systems deliver glycaemic benefits for individuals with type 2 diabetes, whether treated with insulin or non-insulin therapy; further data are required to evaluate the role of these systems in those with prediabetes (defined as impaired glucose tolerance and/or impaired fasting glucose and/or HbA1c levels between 39 mmol/mol [5.7%] and 47 mmol/mol [6.4%]). The use of insulin pumps seems to be safe and effective in people with type 2 diabetes, especially in those with an HbA1c significantly above target. Initial results from studies exploring the impact of closed-loop systems in type 2 diabetes are promising. We discuss directions for future research to fully understand the potential benefits of integrating evidence-based technology into care for people living with type 2 diabetes and prediabetes.
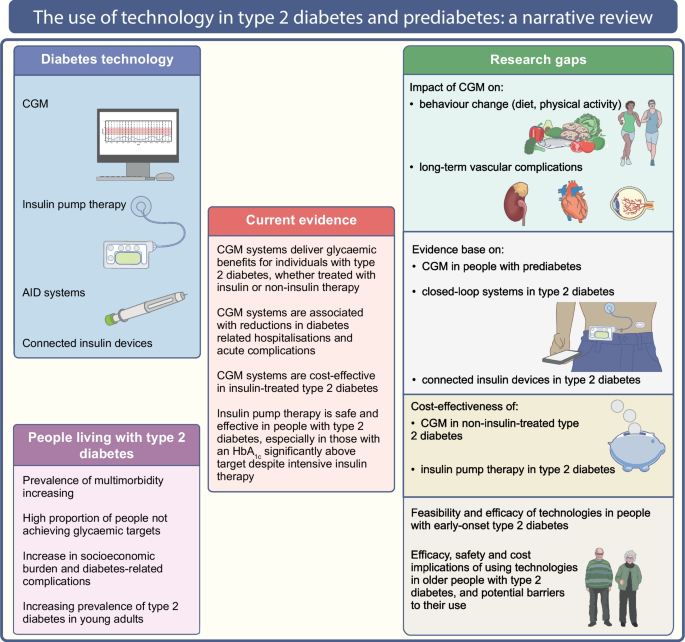
Graphical Abstract
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a major public health issue characterised as a worldwide pandemic. A total of 537 million adults live with diabetes globally, with 90% of all cases diagnosed as type 2 diabetes [1]. This figure is predicted to rise by almost 50% in the next 20 years, which will be associated with increased rates of vascular complications [1]. Improved glucose management reduces the risk of vascular complications and mortality in people with type 2 diabetes [2,3,4,5]. However, data suggest that only around 50% of people with type 2 diabetes achieve the recommended HbA1c target of <53 mmol/mol (7%) [6, 7], highlighting the need for better therapeutic options.
Technologies such as continuous glucose monitoring (CGM), insulin pumps and automated insulin delivery (AID) therapies have been shown to improve HbA1c, reduce hypoglycaemia and diabetes distress, and improve quality of life (QoL) in people with type 1 diabetes [8,9,10], and it is becoming increasingly evident that type 2 diabetes populations can also benefit from these advances [11, 12].
The aim of this review is to describe the current evidence regarding the role of technologies in people with type 2 diabetes, based on randomised trials, observational studies, systematic reviews and meta-analyses. We used the keywords ‘type 2 diabetes’, ‘diabetes technology’, ‘continuous glucose monitoring’, ‘flash glucose monitoring’, ‘intermittently-scanned continuous glucose monitoring’, ‘real-time continuous glucose monitoring’, ‘continuous subcutaneous insulin infusion’, ‘insulin pump’, ‘closed-loop’, ‘automated insulin delivery’, ‘artificial pancreas’, ‘connected insulin devices’, ‘smart insulin pen’ and ‘smart insulin pen caps’ alone and in combination to retrieve available literature from PubMed from inception until January 2024. The current evidence and research gaps in the use of technology in type 2 diabetes and prediabetes (defined as impaired glucose tolerance and/or impaired fasting glucose and/or HbA1c levels between 39 mmol/mol [5.7%] and 47 mmol/mol [6.4%]) are illustrated in Fig. 1.
The use of technology in type 2 diabetes and prediabetes. This figure describes the current evidence and research gaps in the use of technology in type 2 diabetes and prediabetes. CGM improves glucose management in insulin- and non-insulin-treated type 2 diabetes, while the role of CGM in prediabetes requires further research. Insulin pumps improve glucose management in individuals with type 2 diabetes, especially in those with high HbA1c despite intensive insulin therapy. The impact of CGM on behaviour changes and vascular complications, and the evidence base on connected insulin devices and closed-loop systems in type 2 diabetes, require further investigation. This figure is available as a downloadable slide
CGM in type 2 diabetes
Current glucose monitoring technology enables intermittently scanned CGM (isCGM) and real-time CGM (rtCGM). isCGM involves sensors that need to be scanned to provide glucose values, while in rtCGM the sensors display glucose data on a reader or app automatically, without the need for scanning.
A meta-analysis of 26 RCTs (17 rtCGM, nine isCGM), involving 2783 people with type 2 diabetes, showed that, compared with self-monitoring of blood glucose (SMBG), rtCGM and isCGM reduced HbA1c by 0.19 percentage points (pp) (2 mmol/mol) (95% CI −0.34, −0.04 pp) and 0.31 pp (3 mmol/mol) (95% CI −0.46, −0.17 pp), respectively. Time in range (TIR) increased significantly in isCGM users (three RCTs) and non-significantly in rtCGM users (six RCTs) [13]. CGM did not significantly impact glucose concentrations, glucose variability, measures of body composition, blood pressure or lipid levels [14, 15]. There was no difference in risk of hypoglycaemia between CGM and SMBG [14, 16,17,18,19]. Treatment satisfaction improved with CGM use, especially with newer generation systems, compared with SMBG [13, 17, 20, 21]. A more recent systematic review of CGM in adults with type 2 diabetes, which excluded studies investigating professional CGM and those combining CGM with additional glucose-lowering treatment, identified 12 RCTs (eight rtCGM, four isCGM) involving 1248 people [22]. Compared with SMBG, CGM (isCGM or rtCGM) resulted in a reduction in HbA1c (mean difference [MD] −3.43 mmol/mol [−0.31 pp], 95% CI −4.75, −2.11 mmol/mol; p<0.00001). The effect size was comparable between studies including individuals on insulin ± oral therapy (MD −3.27 mmol/mol [−0.30 pp], 95% CI −6.22, −0.31 mmol/mol; p=0.03) and studies including those on oral therapy only (MD −3.22 mmol/mol [−0.29 pp], 95% CI −5.39, −1.05 mmol/mol; p=0.004). Using rtCGM showed a trend towards a larger effect (MD −3.95 mmol/mol [−0.36 pp], 95% CI −5.46, −2.44 mmol/mol; p<0.00001) than using isCGM (MD −1.79 mmol/mol [−0.16 pp], 95% CI −5.28, 1.69 mmol/mol; p=0.31). CGM compared with SMBG was also associated with increased TIR (+6.36%, 95% CI +2.48%, +10.24%; p=0.001) and decreased time below range (TBR) (−0.66 pp, 95% CI −1.21, −0.12 pp; p=0.02). No significant differences in severe hypoglycaemia or macrovascular complications were found between CGM and SMBG. No trials reported data on microvascular complications [22]. Table 1 summarises the main findings of the key RCTs on CGM use in type 2 diabetes.
CGM use in people with type 2 diabetes on intensive insulin therapies
The DIAMOND RCT [15] showed that, compared with SMBG, rtCGM resulted in a greater HbA1c reduction (MD −0.3 pp [–3 mmol/mol]) in a type 2 diabetes population treated with multiple daily insulin injections (MDI). However, the study did not incorporate structured diabetes education to optimise self-management and included people undertaking SMBG at least twice daily at baseline, while the control group were asked to perform SMBG four or more times daily. This may have resulted in underestimation of the impact of rtCGM on plasma glucose levels. In the REPLACE RCT, isCGM resulted in no difference in HbA1c compared with SMBG. Nevertheless, the hypoglycaemia burden decreased and treatment satisfaction improved in isCGM users. An inclusion criterion of SMBG at least twice daily at baseline was reported and no education on data interpretation was provided [17], suggesting possible underestimation of the impact of isCGM on HbA1c. Another RCT of isCGM vs SMBG in a type 2 diabetes population on MDI showed that, although the primary outcome of treatment satisfaction was not met (p=0.053), users reported more flexibility (p=0.019) and would recommend isCGM to others (p=0.023) [23].
Overall, using CGM in those on intensive insulin therapy is beneficial. Several RCTs and real-world retrospective studies support CGM use, demonstrating improvements in HbA1c and decreased frequency and severity of hypoglycaemia [24,25,26,27]. However, to date, no studies have investigated the impact of CGM in people with type 2 diabetes treated with mixed insulin; further research is required to evaluate the potential benefits in this group.
CGM use in people with type 2 diabetes on basal insulin
The MOBILE RCT [14] found that, compared with SMBG, rtCGM resulted in a greater HbA1c reduction (MD −4 mmol/mol [–0.4 pp]), improved TIR and decreased time above range (TAR) and TBR in a type 2 diabetes population treated with basal insulin (p<0.05 for all). The total dose of insulin and body weight did not differ between groups, which raises the possibility that rtCGM use may be directly associated with dietary and activity changes. This is an area that needs to be addressed in future research to gain a more detailed understanding of how CGM may drive glycaemic improvements in this group.
CGM use in people with type 2 diabetes on non-insulin therapy
A pilot RCT of a structured diabetes education programme with episodic rtCGM use in a non-insulin-treated type 2 diabetes population demonstrated no significant HbA1c improvement compared with SMBG [28], while an RCT of intermittent short-term use of rtCGM compared with SMBG found a 0.64 pp (6 mmol/mol) HbA1c reduction (p=0.014) [29]. In another RCT [30], isCGM users showed a higher HbA1c reduction than SMBG users at 24 weeks (MD –3.2 mmol/mol [−0.29 pp]; p=0.022). The IMMEDIATE RCT explored the glycaemic efficacy of isCGM plus diabetes self-management education compared with education alone in a type 2 diabetes population on at least one non-insulin therapy [11]. TIR at 4 months was higher in isCGM users (p=0.009), with little change in medication use (non-insulin glucose-lowering therapies were added for <10% of participants in each arm). This raises the possibility that CGM use may change behaviours, impacting glycaemic outcomes. The effect of CGM use on behaviour change is an area ripe for future research.
A retrospective analysis of 728 people with type 2 diabetes on non-insulin therapies using isCGM found a 1.6 pp (16 mmol/mol) HbA1c reduction (p<0.001); a limitation of this analysis was the lack of a control group [31].
CGM use and acute diabetes-related complications and hospitalisation
The RELIEF [32] retrospective study evaluated 40,846 people with type 2 diabetes (and 33,165 individuals with type 1 diabetes) in the first 12 months following isCGM initiation. Most within the type 2 diabetes cohort were treated with MDI, while a small proportion were treated with basal insulin or oral agents only. Twelve months following isCGM initiation, hospitalisation for acute diabetes complications decreased by 39% [32]. Specifically, in the type 2 diabetes population, the annual percentage of hospital admissions decreased for diabetic ketoacidosis (DKA) (from 1.7% to 0.82%), hypoglycaemia (from 0.7% to 0.62%), diabetes-related comas (from 0.23% to 0.16%) and hyperglycaemia (from 0.12% to 0.09%). The 2-year follow-up showed a persistent reduction in acute diabetes-related hospitalisations, from 2.0% before initiating isCGM to 0.75% at 1 year and 0.6% at 2 years follow-up [33]. Similarly, in a retrospective study carried out in the Netherlands, use of isCGM reduced diabetes-related hospital admissions from 13.7% to 4.7% (p<0.05) [34].
The LIBERATES RCT [18] investigated the effect of isCGM vs SMBG on blood glucose levels in a type 2 diabetes population with acute myocardial infarction, already treated with therapies that may result in hypoglycaemia. Although there was no significant difference in HbA1c or TIR between groups, isCGM significantly reduced the subsequent risk of hypoglycaemia (Table 1).
CGM use in prediabetes
An RCT in individuals with prediabetes showed that isCGM combined with lifestyle coaching improved blood glucose levels and reduced carbohydrate intake and body weight [35]. A pilot RCT in 13 individuals with prediabetes or type 2 diabetes suggested that rtCGM may facilitate self-monitoring behaviour and increase exercise adherence accompanied by improvements in health-related QoL [36]. Similarly, a qualitative study in 26 individuals at moderate to high risk of developing type 2 diabetes suggested that using a combination of isCGM and a physical activity monitor may increase self-awareness regarding the impact of lifestyle on short-term health and guide behaviour change [37]. However, the feedback provided by the devices lacked meaning for several individuals, posing barriers to making changes to diet and physical activity levels. Hence, these findings highlight the need for further research to explore potential modifications required to digital health technologies, including CGM, to sustain engagement and behaviour change in individuals with prediabetes.
In summary, high-quality evidence demonstrates that both isCGM and rtCGM deliver glycaemic benefits for people with type 2 diabetes, whether treated with insulin or non-insulin therapy. The available data suggest that the mechanisms for improvements in blood glucose levels in response to CGM may not be directly reacted to therapeutic change, as one might assume. Further studies are required to provide a detailed understanding of the impact of CGM on dietary intake and physical activity, in addition to exploring the potential benefits of CGM in those with type 2 diabetes treated with mixed insulins.
Continuous subcutaneous insulin infusion in type 2 diabetes
Continuous subcutaneous insulin infusion (CSII), also known as insulin pump therapy, has a clear place in the management of type 1 diabetes [38]. In contrast, the guidelines for using CSII in type 2 diabetes are less consistent [39,40,41].
The OpT2mise RCT, which included 331 individuals with MDI-treated type 2 diabetes, found that, compared with MDI, CSII resulted in a significant 0.7 pp (7 mmol/mol) HbA1c reduction after 6 months, without increased rates of hypoglycaemia, DKA or hospitalisation [42]. In another RCT, individuals randomised to the CSII arm achieved a significant 0.9 pp (9 mmol/mol) HbA1c reduction compared with 0.3 pp (3 mmol/mol) in the MDI arm. After 6 months, the MDI arm crossed over to CSII and at 12 months the individuals continuing CSII had an additional 0.7 pp (7 mmol/mol) reduction in HbA1c and those switching from MDI to CSII experienced a 0.5 pp (5 mmol/mol) HbA1c reduction [43]. Similarly, the VIVID study demonstrated that, compared with MDI, CSII improved HbA1c without increasing body weight or severe hypoglycaemia [44].
Real-world data suggest that using CSII in type 2 diabetes can be safe and effective for improving blood glucose levels, particularly in those individuals with higher HbA1c levels, and is associated with high user satisfaction [45,46,47]. In one study, the HbA1c reduction was sustained for 6 years, indicating the potential long-term benefits of CSII therapy for those with type 2 diabetes [46].
Initiating CSII in type 2 diabetes has been associated with improved patient-reported outcomes and user satisfaction [48]. A recent real-world study demonstrated that, compared with MDI, use of a tubeless insulin pump in adults with type 2 diabetes contributed to significant behavioural and psychosocial benefits, including improvements in overall well-being, diabetes distress, hypoglycaemia-related concerns and QoL, as well as greater glycaemic improvement [49]. User satisfaction and improved glycaemic outcomes have also been shown in studies exploring the use of simplified CSII systems with no need for pump programming or detailed education sessions [50, 51].
Overall, CSII is safe and effective in populations with type 2 diabetes, especially in those with an HbA1c significantly above target despite MDI. CSII may also be associated with decreased healthcare costs as a result of lower rates of diabetes-related complications [51,52,53,54].
AID systems in type 2 diabetes
AID systems, also known as closed-loop systems, include ‘hybrid’ closed-loop (HCL) therapies, which require carbohydrate counting and user-initiated, pump-delivered meal boluses, and fully closed-loop systems, which eliminate the need for manual mealtime boluses.
An RCT in 136 individuals with type 2 diabetes showed that, compared with subcutaneous insulin therapy, a fully AID system resulted in a significant 24.3 pp TIR increase and 25.9 pp TAR reduction without increasing hypoglycaemia. User satisfaction was also high in the closed-loop group [55]. Similar results were observed in other RCTs performed in inpatient settings [56, 57].
Randomised trials conducted in outpatient settings also suggest glycaemic benefits of fully closed-loop systems [58,59,60]. A randomised crossover study in 26 adults with type 2 diabetes compared a fully closed-loop system with standard insulin therapy and a masked glucose sensor (control). The authors demonstrated a significant 15 mmol/mol (1.4 pp) HbA1c reduction and 35.3 pp TIR increase without elevated hypoglycaemia rates following closed-loop therapy compared with control [59].
A recent meta-analysis of seven RCTs assessing the efficacy of fully closed-loop systems compared with conventional insulin therapy in 390 people with type 2 diabetes showed that fully closed-loop systems improved TIR (MD +22.40 pp, 95% CI 12.88, 31.91 pp; p<0.01) and reduced TAR (MD −22.67 pp, 95% CI −30.87, −14.46 pp; p<0.01) without a significant difference in hypoglycaemia [61].
The literature on HCL therapies in type 2 diabetes is limited [62, 63]. A feasibility trial in 24 adults with type 2 diabetes managed in an outpatient setting found that HCL was associated with a 14 mmol/mol (1.3 pp) HbA1c reduction, 21.9 pp TIR increase, 16.9 pp TAR reduction and 0% of time at glucose <3 mmol/l (<54 mg/dl), without a significant change in total daily insulin dose or body weight [62]. Similarly, a prospective single-arm trial demonstrated a substantial glycaemic improvement (TIR increased by 15 pp) without increased hypoglycaemia in 30 adults with type 2 diabetes using HCL therapy [63].
In summary, small studies suggest that closed-loop systems could be a potential future therapeutic option in type 2 diabetes. More long-term follow-up studies are required to assess their clinical and cost-effectiveness.
Connected insulin devices in type 2 diabetes
Missed and late insulin injections negatively impact blood glucose levels [64]. Connected insulin devices, including tracking insulin pens, and smart insulin pens and caps, can record and transfer data about insulin doses and timing to smartphone applications, as well as provide reminders to bolus and facilitate insulin dose calculations [65]. These features support decision making and inform counselling strategies for the diabetes care team [65,66,67,68].
In a randomised trial that aimed to assess the efficacy of a smart insulin pen cap for the management of individuals with suboptimally controlled type 2 diabetes (intervention group: feedback and alarm notifications; control group: masked device without alarm notifications), compared with the control group (n=40), the intervention group (n=40) experienced a greater HbA1c reduction (−0.98 pp [–10 mmol/mol] vs −0.72 pp [–7 mmol/mol]; p=0.006) and lower blood glucose levels (8.2 ± 1.9 vs 8.7 ± 2.3 mmol/l [147.0 ± 34 vs 157.6 ± 42 mg/dl]; p<0.01). The device was also associated with high user satisfaction [69]. In the STYLCONNECT study, people with type 2 diabetes showed a strong interest in using a device that could automate the collection of their insulin data and integrate data from glucose measurement devices [70]. Another study demonstrated that people with type 2 diabetes preferred connected over non-connected insulin pens because of the capability for automated recording of insulin dose and glucose levels [71].
Evidence around the use of connected insulin devices in type 2 diabetes is still in an early phase. However, existing literature suggests that these systems may have the potential to improve plasma glucose and user satisfaction, highlighting the importance of further research in this area [72].
Special groups
Early-onset type 2 diabetes
Type 2 diabetes in young people is associated with an excess lifetime risk of vascular complications and premature death [73,74,75,76]. Improving HbA1c is crucial to reduce long-term diabetes-related complications and mortality rates [3, 4]. Despite emerging evidence suggesting the glycaemic benefits of technologies such as CGM in older adults with type 2 diabetes [11, 12], research around the use of such systems in young individuals is scarce and limited to small studies [77, 78]. Small pilot studies suggest that rtCGM is acceptable and feasible and associated with significant improvements in QoL and glycaemic outcomes in adolescents and young adults with type 2 diabetes [77, 78]. To date, there are no studies exploring the impact of CSII or closed-loop systems in young people with type 2 diabetes. Further studies assessing the use of technologies in people with early-onset type 2 diabetes are needed to explore the potential benefit of these therapies in this high-risk cohort.
Pregnancy and type 2 diabetes
Pregnancy complicated by type 2 diabetes is associated with adverse maternal and fetal outcomes [79]. Maternal hyperglycaemia is a major modifiable risk factor for pregnancy outcomes [79], and it seems logical that CGM could improve blood glucose levels and optimise the care of pregnant women with pre-existing diabetes. rtCGM reduces the risk of adverse fetal outcomes in women with type 1 diabetes [80] and may support the management of women with pre-existing diabetes, including the high-risk type 2 diabetes population [81, 82]. Non-randomised studies suggest that isCGM can be useful for improving blood glucose levels in pregnant women with type 2 diabetes and is accurate and well-received [83, 84]. However, RCT-derived data assessing the efficacy of CGM for maternal glucose management and perinatal outcomes in women with type 2 diabetes are currently lacking, while existing studies involve small numbers of individuals [85,86,87]. The ADA clinical practice recommendations for the management of diabetes in pregnancy state that there are insufficient data to support CGM use in all individuals with type 2 diabetes and that the decision to use CGM should be individualised [88]. NICE guidelines on the management of diabetes in pregnancy indicate that rtCGM should be considered in pregnant women with insulin-treated type 2 diabetes if they have problematic severe hypoglycaemia or unstable blood glucose levels causing concern despite efforts to optimise plasma glucose [89]. Although the International Consensus on Time in Range defines CGM target ranges for people with diabetes, there are currently no internationally agreed goals for pregnant women with type 2 diabetes [88, 90].
Future research should aim to investigate the impact of CGM in pregnant women with type 2 diabetes, assess associations of CGM metrics with pregnancy outcomes and identify the appropriate amount of time spent within defined glucose targets for this population.
End-stage renal disease and type 2 diabetes
The evidence for using technologies in the type 2 diabetes population with end-stage renal disease on dialysis is scarce. Observational studies suggest that CGM is an accurate and efficient method of monitoring interstitial glucose levels in individuals receiving haemodialysis [91,92,93,94,95]. Data suggest that there is increased glucose variability during dialysis days, which could be an additional risk factor for cardiovascular complications [96, 97]. CGM can capture glucose variations, guide insulin therapy optimisation and improve glucose levels and hypoglycaemia detection in individuals with insulin-treated type 2 diabetes receiving dialysis [98,99,100]. However, these outcomes should be interpreted with caution as most of the existing studies are observational with short-term follow-up, include small numbers of participants and no control group, and provide very limited evidence on peritoneal dialysis. RCTs and studies with longer follow-up are therefore needed.
A post hoc analysis of an RCT in a type 2 diabetes population undergoing inpatient haemodialysis showed that, compared with subcutaneous insulin therapy, a fully closed-loop system was associated with a significant 37.6% increase in the proportion of time when blood glucose was within the target range (5.6–10.0 mmol/l [100–180 mg/dl]), without increasing hypoglycaemia [101]. Similarly, an RCT in 26 adults with type 2 diabetes requiring dialysis in an outpatient setting showed that a fully AID system significantly increased TIR by 14.6 pp without increased hypoglycaemia compared with standard insulin therapy [58], suggesting that closed-loop systems could be a novel way to achieve safe and effective glucose management in this vulnerable population.
Older people and type 2 diabetes
The adoption of diabetes technologies in older people remains at an early stage and clinical knowledge is currently modest. Cognitive impairment, multimorbidity and sensory deficits due to increasing age are important challenges in this group [102, 103], while the significance of reducing hypoglycaemia is emphasised in international recommendations [90].
Two RCTs including people with type 2 diabetes on MDI over the age of 60 years found that CGM was associated with a 0.3–0.5 pp (3–5 mmol/mol) HbA1c reduction compared with SMBG [15, 23]. Additional data suggesting that pump therapy may be beneficial in older people with type 2 diabetes on MDI were described in the OpT2mise trial, which included individuals aged up to 75 years [42]. Another RCT demonstrated that, compared with MDI, a fully closed-loop system resulted in a significant 27.4 pp TIR increase, a 27.7 pp TAR reduction and an unchanged TBR of <1% in 30 people with type 2 diabetes (mean age 69.5 years) requiring nursing support at home. There were no episodes of severe hypoglycaemia or ketoacidosis and both participants and caregivers were highly satisfied with the AID system [60].
A recent review from the International Geriatric Diabetes Society described the low uptake of diabetes technologies in older adults because of individual and healthcare system-related barriers [104]. Future studies should aim to explore the efficacy, safety, role, cost implications and potential barriers of using technologies in older people with type 2 diabetes, including those with multimorbidity and cognitive and functional impairment and those living in supervised facilities.
Cost-effectiveness of technologies in type 2 diabetes
The increasing prevalence of type 2 diabetes globally, particularly in younger individuals who will live longer with their disease and have an increased risk of costly diabetes-related complications, is expected to result in several challenges for healthcare systems and clinicians. Increased rates of emergency department use and hospital admissions due to diabetes-related complications are associated with significant healthcare costs [105]. Hence, using cost-effective technologies, which improve HbA1c and thereby reduce complications, is imperative.
The cost–benefits of CGM in type 2 diabetes have been described previously [106, 107]. A recent retrospective analysis showed that the mean per-patient per-month cost for diabetes-related medical costs in a type 2 diabetes population decreased by US$424 following ≥6 months of rtCGM use. A decrease in hospital admissions was also reported [108]. Other studies have also demonstrated that CGM use in type 2 diabetes is associated with a reduction in diabetes-related admissions, which would imply cost savings for healthcare systems [24, 33]. A base-case analysis showed that long-term isCGM use was cost-effective compared with SMBG in individuals with type 2 diabetes receiving intensive insulin treatment [109]. Similarly, another analysis demonstrated that rtCGM was likely to be cost-effective compared with SMBG in a type 2 diabetes population receiving insulin therapy, with HbA1c reduction and QoL benefit from reduced fingerstick testing being the main drivers of the outcomes observed [110]. Taken together, the available data suggest that CGM is cost-effective, which has led to the inclusion of such systems in guidelines for the management of type 2 diabetes [40, 111].
Evidence suggesting the cost-effectiveness of CSII in type 2 diabetes is scarce. Compared with MDI, CSII was associated with a gain in quality-adjusted life-years ranging between 0.17 and 0.43 and a 15–20% reduction in diabetes-related complication costs, which mitigated the higher mean lifetime costs [53, 54, 112]. Sensitivity analyses showed that insulin pump therapy was most cost-effective in individuals with the highest baseline HbA1c, suggesting that CSII may represent a cost-effective therapeutic alternative for MDI-treated type 2 diabetes populations who have HbA1c levels above target [112].
To date, there are no cost-effective analyses of closed-loop systems in type 2 diabetes, and studies comparing the cost-effectiveness of such systems with that of the available glucose-lowering therapies are needed. Lastly, connected insulin devices in this population are potentially cost saving, but further data are required [72].
Conclusion
People with type 2 diabetes face several challenges in achieving glycaemic targets. Advances in diabetes technologies have provided tools that can facilitate self-management in this high-risk group, especially those on insulin therapy with HbA1c values above target. Further research will indicate the best place within treatment guidelines of newer technologies such as closed-loop therapies, which have shown very promising results at this initial stage.
Abbreviations
- AID:
-
Automated insulin delivery
- CGM:
-
Continuous glucose monitoring
- CSII:
-
Continuous subcutaneous insulin infusion
- DKA:
-
Diabetic ketoacidosis
- HCL:
-
Hybrid closed-loop
- isCGM:
-
Intermittently scanned continuous glucose monitoring
- MD:
-
Mean difference
- MDI:
-
Multiple daily injections
- pp:
-
Percentage points
- QoL:
-
Quality of life
- rtCGM:
-
Real-time continuous glucose monitoring
- SMBG:
-
Self-monitoring of blood glucose
- TAR:
-
Time above range
- TBR:
-
Time below range
- TIR:
-
Time in range
References
International Diabetes Federation (2021) IDF diabetes atlas, 10th edn. Available from: https://www.diabetesatlas.org. Accessed 14 Jan 2024
UK Prospective Diabetes Study (UKPDS) Group (1998) Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352(9131):854–865. https://doi.org/10.1016/S0140-6736(98)07037-8
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359(15):1577–1589. https://doi.org/10.1056/NEJMoa0806470
Stratton IM, Adler AI, Neil HA et al (2000) Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321(7258):405–412. https://doi.org/10.1136/bmj.321.7258.405
Maranta F, Cianfanelli L, Cianflone D (2021) Glycaemic control and vascular complications in diabetes mellitus type 2. Adv Exp Med Biol 1307:129–152. https://doi.org/10.1007/5584_2020_514
NHS Digital (2023) National Diabetes Audit Core Report 1: Care processes and treatment targets 2022-23, underlying data. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/report-1-cp-and-tt-data-release-2022-23/national-diabetes-audit-report-1---care-processes-and-treatment-targets-2022-23-underlying-data. Accessed 15 Jan 2024
Fang M, Wang D, Coresh J, Selvin E (2021) Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med 384(23):2219–2228. https://doi.org/10.1056/NEJMsa2032271
Deshmukh H, Wilmot EG, Gregory R et al (2020) Effect of flash glucose monitoring on glycemic control, hypoglycemia, diabetes-related distress, and resource utilization in the Association of British Clinical Diabetologists (ABCD) nationwide audit. Diabetes Care 43(9):2153–2160. https://doi.org/10.2337/dc20-0738
Jeyam A, Gibb FW, McKnight JA et al (2021) Marked improvements in glycaemic outcomes following insulin pump therapy initiation in people with type 1 diabetes: a nationwide observational study in Scotland. Diabetologia 64(6):1320–1331. https://doi.org/10.1007/s00125-021-05413-7
Crabtree TSJ, Griffin TP, Yap YW et al (2023) Hybrid closed-loop therapy in adults with type 1 diabetes and above-target HbA1c: a real-world observational study. Diabetes Care 46(10):1831–1838. https://doi.org/10.2337/dc23-0635
Aronson R, Brown RE, Chu L et al (2023) IMpact of flash glucose Monitoring in pEople with type 2 Diabetes Inadequately controlled with non-insulin Antihyperglycaemic ThErapy (IMMEDIATE): A randomized controlled trial. Diabetes Obes Metab 25(4):1024–1031. https://doi.org/10.1111/dom.14949
Choe HJ, Rhee EJ, Won JC, Park KS, Lee WY, Cho YM (2022) Effects of patient-driven lifestyle modification using intermittently scanned continuous glucose monitoring in patients with type 2 diabetes: results from the randomized open-label PDF study. Diabetes Care 45(10):2224–2230. https://doi.org/10.2337/dc22-0764
Seidu S, Kunutsor SK, Ajjan RA, Choudhary P (2023) Efficacy and safety of continuous glucose monitoring and intermittently scanned continuous glucose monitoring in patients with type 2 diabetes: a systematic review and meta-analysis of interventional evidence. Diabetes Care 47(1):169–179. https://doi.org/10.2337/dc23-1520
Martens T, Beck RW, Bailey R et al (2021) Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA 325(22):2262–2272. https://doi.org/10.1001/jama.2021.7444
Beck RW, Riddlesworth TD, Ruedy K et al (2017) Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med 167(6):365–374. https://doi.org/10.7326/m16-2855
Ilany J, Bhandari H, Nabriski D, Toledano Y, Konvalina N, Cohen O (2018) Effect of prandial treatment timing adjustment, based on continuous glucose monitoring, in patients with type 2 diabetes uncontrolled with once-daily basal insulin: A randomized, phase IV study. Diabetes, Obes Metab 20(5):1186–1192. https://doi.org/10.1111/dom.13214
Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline JP, Rayman G (2017) Flash glucose-sensing technology as a replacement for blood glucose monitoring for the management of insulin-treated type 2 diabetes: a multicenter, open-label randomized controlled trial. Diabetes Ther 8(1):55–73. https://doi.org/10.1007/s13300-016-0223-6
Ajjan RA, Heller SR, Everett CC et al (2023) Multicenter randomized trial of intermittently scanned continuous glucose monitoring versus self-monitoring of blood glucose in individuals with type 2 diabetes and recent-onset acute myocardial infarction: results of the LIBERATES trial. Diabetes Care 46(2):441–449. https://doi.org/10.2337/dc22-1219
Ajjan RA, Jackson N, Thomson SA (2019) Reduction in HbA1c using professional flash glucose monitoring in insulin-treated type 2 diabetes patients managed in primary and secondary care settings: a pilot, multicentre, randomised controlled trial. Diab Vasc Dis Res 16(4):385–395. https://doi.org/10.1177/1479164119827456
Cox DJ, Banton T, Moncrief M, Conaway M, Diamond A, McCall AL (2020) Minimizing Glucose Excursions (GEM) with continuous glucose monitoring in type 2 diabetes: a randomized clinical trial. J Endocr Soc 4(11):118. https://doi.org/10.1210/jendso/bvaa118
Tang TS, Digby EM, Wright AM et al (2014) Real-time continuous glucose monitoring versus internet-based blood glucose monitoring in adults with type 2 diabetes: a study of treatment satisfaction. Diabetes Res Clin Pract 106(3):481–486. https://doi.org/10.1016/j.diabres.2014.09.050
Jancev M, Vissers T, Visseren FLJ et al (2024) Continuous glucose monitoring in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetologia 67(5):798–810. https://doi.org/10.1007/s00125-024-06107-6
Yaron M, Roitman E, Aharon-Hananel G et al (2019) Effect of flash glucose monitoring technology on glycemic control and treatment satisfaction in patients with type 2 diabetes. Diabetes Care 42(7):1178–1184. https://doi.org/10.2337/dc18-0166
Miller E, Kerr MSD, Roberts GJ, Nabutovsky Y, Wright E (2021) Flash CGM associated with event reduction in nonintensive diabetes therapy. Am J Manag Care 27(11):e372–e377. https://doi.org/10.37765/ajmc.2021.88780
Fokkert M, van Dijk P, Edens M et al (2019) Improved well-being and decreased disease burden after 1-year use of flash glucose monitoring (FLARE-NL4). BMJ Open Diabetes Res Care 7(1):e000809. https://doi.org/10.1136/bmjdrc-2019-000809
Charleer S, Mathieu C, Nobels F et al (2018) Effect of continuous glucose monitoring on glycemic control, acute admissions, and quality of life: a real-world study. J Clin Endocrinol Metab 103(3):1224–1232. https://doi.org/10.1210/jc.2017-02498
Elliott T, Beca S, Beharry R, Tsoukas MA, Zarruk A, Abitbol A (2021) The impact of flash glucose monitoring on glycated hemoglobin in type 2 diabetes managed with basal insulin in Canada: a retrospective real-world chart review study. Diab Vasc Dis Res 18(4):14791641211021374. https://doi.org/10.1177/14791641211021374
Price DA, Deng Q, Kipnes M, Beck SE (2021) Episodic real-time CGM use in adults with type 2 diabetes: results of a pilot randomized controlled trial. Diabetes Ther 12(7):2089–2099. https://doi.org/10.1007/s13300-021-01086-y
Moon SJ, Kim KS, Lee WJ, Lee MY, Vigersky R, Park CY (2023) Efficacy of intermittent short-term use of a real-time continuous glucose monitoring system in non-insulin-treated patients with type 2 diabetes: A randomized controlled trial. Diabetes Obes Metab 25(1):110–120. https://doi.org/10.1111/dom.14852
Wada E, Onoue T, Kobayashi T et al (2020) Flash glucose monitoring helps achieve better glycemic control than conventional self-monitoring of blood glucose in non-insulin-treated type 2 diabetes: a randomized controlled trial. BMJ Open Diabetes Res Care 8(1):e001115. https://doi.org/10.1136/bmjdrc-2019-001115
Wright EE Jr, Kerr MSD, Reyes IJ, Nabutovsky Y, Miller E (2021) Use of flash continuous glucose monitoring is associated with A1C reduction in people with type 2 diabetes treated with basal insulin or noninsulin therapy. Diabetes Spectr 34(2):184–189. https://doi.org/10.2337/ds20-0069
Roussel R, Riveline JP, Vicaut E et al (2021) Important drop in rate of acute diabetes complications in people with type 1 or type 2 diabetes after initiation of flash glucose monitoring in France: the RELIEF study. Diabetes Care 44(6):1368–1376. https://doi.org/10.2337/dc20-1690
Guerci B, Roussel R, Levrat-Guillen F et al (2023) Important decrease in hospitalizations for acute diabetes events following free style libre system initiation in people with type 2 diabetes on basal insulin therapy in France. Diabetes Technol Ther 25(1):20–30. https://doi.org/10.1089/dia.2022.0271
Bergenstal RM, Kerr MSD, Roberts GJ, Souto D, Nabutovsky Y, Hirsch IB (2021) Flash CGM is associated with reduced diabetes events and hospitalizations in insulin-treated type 2 diabetes. J Endocr Soc 5(4):bvab013. https://doi.org/10.1210/jendso/bvab013
Kitazawa M, Takeda Y, Hatta M et al (2023) Lifestyle intervention with smartphone app and is CGM for people at high risk of type 2 diabetes: randomized trial. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgad639
Bailey KJ, Little JP, Jung ME (2016) Self-monitoring using continuous glucose monitors with real-time feedback improves exercise adherence in individuals with impaired blood glucose: a pilot study. Diabetes Technol Ther 18(3):185–193. https://doi.org/10.1089/dia.2015.0285
Whelan ME, Denton F, Bourne CLA et al (2021) A digital lifestyle behaviour change intervention for the prevention of type 2 diabetes: a qualitative study exploring intuitive engagement with real-time glucose and physical activity feedback. BMC Public Health 21(1):130. https://doi.org/10.1186/s12889-020-09740-z
Holt RIG, DeVries JH, Hess-Fischl A et al (2021) The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 64(12):2609–2652. https://doi.org/10.1007/s00125-021-05568-3
National Institute fo Health and Care Excellence (2008) Continuous subcutaneous insulin infusion for the treatment of diabetes mellitus. Technology appraisal guidance [TA151]. Available from: https://www.nice.org.uk/guidance/ta151. Accessed 16 Jan 2024
American Diabetes Association Professional Practice Committee (2024) 7. Diabetes Technology: Standards of Care in Diabetes-2024. Diabetes Care 47(Suppl 1):S126-s144. https://doi.org/10.2337/dc24-S007
Davies MJ, Aroda VR, Collins BS et al (2022) Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 65(12):1925–1966. https://doi.org/10.1007/s00125-022-05787-2
Reznik Y, Cohen O, Aronson R et al (2014) Insulin pump treatment compared with multiple daily injections for treatment of type 2 diabetes (OpT2mise): a randomised open-label controlled trial. Lancet 384(9950):1265–1272. https://doi.org/10.1016/s0140-6736(14)61037-0
Chlup R, Runzis S, Castaneda J, Lee SW, Nguyen X, Cohen O (2018) Complex assessment of metabolic effectiveness of insulin pump therapy in patients with type 2 diabetes beyond HbA1c reduction. Diabetes Technol Ther 20(2):153–159. https://doi.org/10.1089/dia.2017.0283
Grunberger G, Bhargava A, Ly T et al (2020) Human regular U-500 insulin via continuous subcutaneous insulin infusion versus multiple daily injections in adults with type 2 diabetes: The VIVID study. Diabetes Obes Metab 22(3):434–441. https://doi.org/10.1111/dom.13947
Gentry CK, Cross LB, Gross BN, McFarland MS, Bestermann WH (2011) Retrospective analysis and patient satisfaction assessment of insulin pump therapy in patients with type 2 diabetes. South Med J 104(1):24–28. https://doi.org/10.1097/SMJ.0b013e3181fa7230
Reznik Y, Morera J, Rod A et al (2010) Efficacy of continuous subcutaneous insulin infusion in type 2 diabetes mellitus: a survey on a cohort of 102 patients with prolonged follow-up. Diabetes Technol Ther 12(12):931–936. https://doi.org/10.1089/dia.2010.0110
Stallings DE, Higgins KJ (2023) The use of multiple daily injections versus insulin pump therapy for HgbA1c reduction in patients with insulin-dependent type 2 diabetes. J Am Assoc Nurse Pract 35(10):615–619. https://doi.org/10.1097/jxx.0000000000000890
Frias JP, Bode BW, Bailey TS, Kipnes MS, Brunelle R, Edelman SV (2011) A 16-week open-label, multicenter pilot study assessing insulin pump therapy in patients with type 2 diabetes suboptimally controlled with multiple daily injections. J Diabetes Sci Technol 5(4):887–893. https://doi.org/10.1177/193229681100500410
Polonsky WH, Soriano EC (2023) Psychosocial and glycemic benefits for insulin-using adults with type 2 diabetes after six months of pump therapy: a quasi-experimental approach. J Diabetes Sci Technol 4:19322968231198532. https://doi.org/10.1177/19322968231198533
Mader JK, Lilly LC, Aberer F et al (2018) Improved glycaemic control and treatment satisfaction with a simple wearable 3-day insulin delivery device among people with Type 2 diabetes. Diabet Med 35(10):1448–1456. https://doi.org/10.1111/dme.13708
Ekanayake P, Edelman S (2023) Identifying patients with type 2 diabetes who might benefit from insulin pump therapy: Literature review, clinical opportunities, potential benefits and challenges. Diabetes Obes Metab 25(Suppl 2):3–20. https://doi.org/10.1111/dom.15059
David G, Gill M, Gunnarsson C, Shafiroff J, Edelman S (2014) Switching from multiple daily injections to CSII pump therapy: insulin expenditures in type 2 diabetes. Am J Manag Care 20(11):e490-497
Roze S, Duteil E, Smith-Palmer J et al (2016) Cost-effectiveness of continuous subcutaneous insulin infusion in people with type 2 diabetes in the Netherlands. J Med Econ 19(8):742–749. https://doi.org/10.3111/13696998.2016.1167695
Wahlqvist P, Warner J, Morlock R (2018) Cost-effectiveness of simple insulin infusion devices compared to multiple daily injections in uncontrolled type 2 diabetics in the United States based on a simulation model. J Health Econ Outcomes Res 6(1):84–95. https://doi.org/10.36469/9789
Bally L, Thabit H, Hartnell S et al (2018) Closed-loop insulin delivery for glycemic control in noncritical care. N Engl J Med 379(6):547–556. https://doi.org/10.1056/NEJMoa1805233
Thabit H, Hartnell S, Allen JM et al (2017) Closed-loop insulin delivery in inpatients with type 2 diabetes: a randomised, parallel-group trial. Lancet Diabetes Endocrinol 5(2):117–124. https://doi.org/10.1016/s2213-8587(16)30280-7
Boughton CK, Bally L, Martignoni F et al (2019) Fully closed-loop insulin delivery in inpatients receiving nutritional support: a two-centre, open-label, randomised controlled trial. Lancet Diabetes Endocrinol 7(5):368–377. https://doi.org/10.1016/s2213-8587(19)30061-0
Boughton CK, Tripyla A, Hartnell S et al (2021) Fully automated closed-loop glucose control compared with standard insulin therapy in adults with type 2 diabetes requiring dialysis: an open-label, randomized crossover trial. Nat Med 27(8):1471–1476. https://doi.org/10.1038/s41591-021-01453-z
Daly AB, Boughton CK, Nwokolo M et al (2023) Fully automated closed-loop insulin delivery in adults with type 2 diabetes: an open-label, single-center, randomized crossover trial. Nat Med 29(1):203–208. https://doi.org/10.1038/s41591-022-02144-z
Reznik Y, Carvalho M, Fendri S et al (2024) Should people with type 2 diabetes treated by multiple daily insulin injections with home health care support be switched to hybrid closed-loop? The CLOSE AP+ randomized controlled trial. Diabetes Obes Metab 26(2):622–630. https://doi.org/10.1111/dom.15351
Amer BE, Yaqout YE, Abozaid AM, Afifi E, Aboelkhier MM (2024) Does fully closed-loop automated insulin delivery improve glycaemic control in patients with type 2 diabetes? A meta-analysis of randomized controlled trials. Diabet Med 41(1):e15196. https://doi.org/10.1111/dme.15196
Davis GM, Peters AL, Bode BW et al (2023) Safety and efficacy of the omnipod 5 automated insulin delivery system in adults with type 2 diabetes: from injections to hybrid closed-loop therapy. Diabetes Care 46(4):742–750. https://doi.org/10.2337/dc22-1915
Levy CJ, Raghinaru D, Kudva YC et al (2024) Beneficial effects of control-IQ automated insulin delivery in basal-bolus and basal-only insulin users with type 2 diabetes. Clin Diabetes 42(1):116–124. https://doi.org/10.2337/cd23-0025
Randløv J, Poulsen JU (2008) How much do forgotten insulin injections matter to hemoglobin a1c in people with diabetes? A simulation study. J Diabetes Sci Technol 2(2):229–235. https://doi.org/10.1177/193229680800200209
Lingen K, Pikounis T, Bellini N, Isaacs D (2023) Advantages and disadvantages of connected insulin pens in diabetes management. Endocr Connect 12(11):e230108. https://doi.org/10.1530/ec-23-0108
MacLeod J, Im GH, Smith M, Vigersky RA (2024) Shining the spotlight on multiple daily insulin therapy: real-world evidence of the InPen smart insulin pen. Diabetes Technol Ther 26(1):33–39. https://doi.org/10.1089/dia.2023.0365
MacLeod J, Vigersky RA (2023) A review of precision insulin management with smart insulin pens: opening up the digital door to people on insulin injection therapy. J Diabetes Sci Technol 17(2):283–289. https://doi.org/10.1177/19322968221134546
Heinemann L, Jendle J (2023) Language matters: connected pens, smart pens, connected smart pens, or just digital pens? J Diabetes Sci Technol 17(4):875–877. https://doi.org/10.1177/19322968221148508
Galindo RJ, Ramos C, Cardona S et al (2023) Efficacy of a smart insulin pen cap for the management of patients with uncontrolled type 2 diabetes: a randomized cross-over trial. J Diabetes Sci Technol 17(1):201–207. https://doi.org/10.1177/19322968211033837
Naïditch N, Mauchant C, Benabbad I et al (2023) STYLCONNECT study: an assessment of automatic data collection devices by people living with diabetes and using an insulin pen. Diabetes Ther 14(2):303–318. https://doi.org/10.1007/s13300-022-01337-6
Seo J, Heidenreich S, Aldalooj E et al (2023) Patients’ preferences for connected insulin pens: a discrete choice experiment among patients with type 1 and type 2 diabetes. Patient 16(2):127–138. https://doi.org/10.1007/s40271-022-00610-x
Cranston I, Jamdade V, Liao B, Newson RS (2023) Clinical, economic, and patient-reported benefits of connected insulin pen systems: a systematic literature review. Adv Ther 40(5):2015–2037. https://doi.org/10.1007/s12325-023-02478-1
Duncan BB, Schmidt MI (2023) Many years of life lost to young-onset type 2 diabetes. Lancet Diabetes Endocrinol 11(10):709–710. https://doi.org/10.1016/s2213-8587(23)00255-3
Misra S, Ke C, Srinivasan S et al (2023) Current insights and emerging trends in early-onset type 2 diabetes. Lancet Diabetes Endocrinol 11(10):768–782. https://doi.org/10.1016/s2213-8587(23)00225-5
Magliano DJ, Sacre JW, Harding JL, Gregg EW, Zimmet PZ, Shaw JE (2020) Young-onset type 2 diabetes mellitus - implications for morbidity and mortality. Nat Rev Endocrinol 16(6):321–331. https://doi.org/10.1038/s41574-020-0334-z
Emerging Risk Factors Collaboration (2023) Life expectancy associated with different ages at diagnosis of type 2 diabetes in high-income countries: 23 million person-years of observation. Lancet Diabetes Endocrinol 11(10):731–742. https://doi.org/10.1016/s2213-8587(23)00223-1
Chesser H, Srinivasan S, Puckett C, Gitelman SE, Wong JC (2022) Real-time continuous glucose monitoring in adolescents and young adults with type 2 diabetes can improve quality of life. J Diabetes Sci Technol 19322968221139873. https://doi.org/10.1177/19322968221139873
Chang N, Barber ROB, Llovido Alula J, Durazo-Arvizu R, Chao LC (2023) Continuous glucose monitoring versus standard of care in adolescents with type 2 diabetes: a pilot randomized cross-over trial. J Diabetes Sci Technol 17:1419–1420. https://doi.org/10.1177/19322968231178284
Murphy HR, Howgate C, O’Keefe J et al (2021) Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: a 5-year national population-based cohort study. Lancet Diabetes Endocrinol 9(3):153–164. https://doi.org/10.1016/s2213-8587(20)30406-x
Feig DS, Donovan LE, Corcoy R et al (2017) Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet 390(10110):2347–2359. https://doi.org/10.1016/s0140-6736(17)32400-5
Sanusi AA, Xue Y, McIlwraith C et al (2024) Association of continuous glucose monitoring metrics with pregnancy outcomes in patients with preexisting diabetes. Diabetes Care 47(1):89–96. https://doi.org/10.2337/dc23-0636
McLean A, Barr E, Tabuai G, Murphy HR, Maple-Brown L (2023) Continuous glucose monitoring metrics in high-risk pregnant women with type 2 diabetes. Diabetes Technol Ther 25(12):836–844. https://doi.org/10.1089/dia.2023.0300
McLean A, Sinha A, Barr E, Maple-Brown L (2023) Feasibility and acceptability of intermittently scanned continuous glucose monitoring for women with type 2 diabetes in pregnancy. J Diabetes Sci Technol 17:256–258. https://doi.org/10.1177/19322968221124956
Scott EM, Bilous RW, Kautzky-Willer A (2018) Accuracy, user acceptability, and safety evaluation for the FreeStyle Libre flash glucose monitoring system when used by pregnant women with diabetes. Diabetes Technol Ther 20(3):180–188. https://doi.org/10.1089/dia.2017.0386
Wilkie G, Melnik V, Brainard L et al (2023) Continuous glucose monitor use in type 2 diabetes mellitus in pregnancy and perinatal outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol MFM 5(7):100969. https://doi.org/10.1016/j.ajogmf.2023.100969
Tumminia A, Milluzzo A, Festa C et al (2021) Efficacy of flash glucose monitoring in pregnant women with poorly controlled pregestational diabetes (FlashMom): a randomized pilot study. Nutr Metab Cardiovasc Dis 31(6):1851–1859. https://doi.org/10.1016/j.numecd.2021.03.013
Rademaker D, van der Wel AWT, van Eekelen R et al (2023) Continuous glucose monitoring metrics and pregnancy outcomes in insulin-treated diabetes: a post-hoc analysis of the GlucoMOMS trial. Diabetes Obes Metab 25(12):3798–3806. https://doi.org/10.1111/dom.15276
American Diabetes Association Professional Practice Committee (2024) 15. Management of diabetes in pregnancy: standards of care in diabetes-2024. Diabetes Care 47(Suppl 1):S282-s294. https://doi.org/10.2337/dc24-S015
National Institute for Health and Care Excellence (2020) Diabetes in pregnancy: management from preconception to the postnatal period. NICE guideline [NG3]. Available from: https://www.nice.org.uk/guidance/ng3. Accessed 20 Jan 2024
Battelino T, Danne T, Bergenstal RM et al (2019) Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 42(8):1593–1603. https://doi.org/10.2337/dci19-0028
Villard O, Breton MD, Rao S et al (2022) Accuracy of a factory-calibrated continuous glucose monitor in individuals with diabetes on hemodialysis. Diabetes Care 45(7):1666–1669. https://doi.org/10.2337/dc22-0073
Hissa MRN, Hissa PNG, Guimarães SB, Hissa MN (2021) Use of continuous glucose monitoring system in patients with type 2 mellitus diabetic during hemodialysis treatment. Diabetol Metab Syndr 13(1):104. https://doi.org/10.1186/s13098-021-00722-8
Mambelli E, Cristino S, Mosconi G, Göbl C, Tura A (2021) Flash glucose monitoring to assess glycemic control and variability in hemodialysis patients: the GIOTTO study. Front Med (Lausanne) 8:617891. https://doi.org/10.3389/fmed.2021.617891
Wang F, Wang D, Lu XL, Sun XM, Duan BH (2022) Continuous glucose monitoring in diabetes patients with chronic kidney disease on dialysis: a meta-analysis. Minerva Endocrinol (Torino) 47(3):325–333. https://doi.org/10.23736/s2724-6507.20.03284-8
Avari P, Tang W, Jugnee N et al (2023) The accuracy of continuous glucose sensors in people with diabetes undergoing hemodialysis (ALPHA Study). Diabetes Technol Ther 25(7):447–456. https://doi.org/10.1089/dia.2023.0013
Yusof Khan AHK, Zakaria NF, Zainal Abidin MA, Kamaruddin NA (2021) Prevalence of glycemic variability and factors associated with the glycemic arrays among end-stage kidney disease patients on chronic hemodialysis. Medicine (Baltimore) 100(30):e26729. https://doi.org/10.1097/md.0000000000026729
Colette C, Monnier L (2007) Acute glucose fluctuations and chronic sustained hyperglycemia as risk factors for cardiovascular diseases in patients with type 2 diabetes. Horm Metab Res 39(9):683–686. https://doi.org/10.1055/s-2007-985157
Mirani M, Berra C, Finazzi S et al (2010) Inter-day glycemic variability assessed by continuous glucose monitoring in insulin-treated type 2 diabetes patients on hemodialysis. Diabetes Technol Ther 12(10):749–753. https://doi.org/10.1089/dia.2010.0052
Gallieni M, De Salvo C, Lunati ME et al (2021) Continuous glucose monitoring in patients with type 2 diabetes on hemodialysis. Acta Diabetol 58(8):975–981. https://doi.org/10.1007/s00592-021-01699-6
Jakubowska Z, Malyszko J (2023) Continuous glucose monitoring in people with diabetes and end-stage kidney disease-review of association studies and Evidence-Based discussion. J Nephrol https://doi.org/10.1007/s40620-023-01802-w
Bally L, Gubler P, Thabit H et al (2019) Fully closed-loop insulin delivery improves glucose control of inpatients with type 2 diabetes receiving hemodialysis. Kidney Int 96(3):593–596. https://doi.org/10.1016/j.kint.2019.03.006
Srikanth V, Sinclair AJ, Hill-Briggs F, Moran C, Biessels GJ (2020) Type 2 diabetes and cognitive dysfunction-towards effective management of both comorbidities. Lancet Diabetes Endocrinol 8(6):535–545. https://doi.org/10.1016/s2213-8587(20)30118-2
Espeland MA, Justice JN, Bahnson J et al (2022) Eight-year changes in multimorbidity and frailty in adults with type 2 diabetes mellitus: associations with cognitive and physical function and mortality. J Gerontol A Biol Sci Med Sci 77(8):1691–1698. https://doi.org/10.1093/gerona/glab342
Huang ES, Sinclair A, Conlin PR et al (2023) The growing role of technology in the care of older adults with diabetes. Diabetes Care 46(8):1455–1463. https://doi.org/10.2337/dci23-0021
Stedman M, Lunt M, Davies M et al (2020) Cost of hospital treatment of type 1 diabetes (T1DM) and type 2 diabetes (T2DM) compared to the non-diabetes population: a detailed economic evaluation. BMJ Open 10(5):e033231. https://doi.org/10.1136/bmjopen-2019-033231
Aleppo G, Hirsch IB, Parkin CG et al (2023) Coverage for continuous glucose monitoring for individuals with type 2 diabetes treated with nonintensive therapies: an evidence-based approach to policymaking. Diabetes Technol Ther 25(10):741–751. https://doi.org/10.1089/dia.2023.0268
Fonda SJ, Graham C, Munakata J, Powers JM, Price D, Vigersky RA (2016) The cost-effectiveness of Real-Time Continuous Glucose Monitoring (RT-CGM) in type 2 diabetes. J Diabetes Sci Technol 10(4):898–904. https://doi.org/10.1177/1932296816628547
Norman GJ, Paudel ML, Parkin CG, Bancroft T, Lynch PM (2022) Association between real-time continuous glucose monitor use and diabetes-related medical costs for patients with type 2 diabetes. Diabetes Technol Ther 24(7):520–524. https://doi.org/10.1089/dia.2021.0525
Ajjan R, Bilir SP, Hellmund R, Souto D (2022) Cost-effectiveness analysis of flash glucose monitoring system for people with type 2 diabetes receiving intensive insulin treatment. Diabetes Ther 13(11–12):1933–1945. https://doi.org/10.1007/s13300-022-01325-w
Isitt JJ, Roze S, Sharland H et al (2022) Cost-effectiveness of a real-time continuous glucose monitoring system versus self-monitoring of blood glucose in people with type 2 diabetes on insulin therapy in the UK. Diabetes Ther 13(11–12):1875–1890. https://doi.org/10.1007/s13300-022-01324-x
National Institute for Health and Care Excellence (2022) Type 2 diabetes in adults: management. NICE guideline [NG28]. Available from: https://www.nice.org.uk/guidance/ng28. Accessed 16 Jan 2024
Roze S, Smith-Palmer J, Delbaere A et al (2019) Cost-effectiveness of continuous subcutaneous insulin infusion versus multiple daily injections in patients with poorly controlled type 2 diabetes in Finland. Diabetes Ther 10(2):563–574. https://doi.org/10.1007/s13300-019-0575-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This review received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Authors’ relationships and activities
ALL has received support to attend conferences from Eli Lilly and Novo Nordisk and research support from the Association of British Clinical Diabetologists. LL has received research support from Abbott Diabetes Care and Dexcom, participated in advisory groups for Abbott Diabetes Care, Insulet, Dexcom, Medtronic and Roche Diabetes, and received fees for speaking from Sanofi, Insulet, Medtronic and Abbott. EGW has received personal fees from Abbott, AstraZeneca, Dexcom, Eli Lilly, Embecta, Glooko, Insulet, Medtronic, Novo Nordisk, Roche, Sanofi, Sinocare and Ypsomed, research support from the Association of British Clinical Diabetologists, Abbott, Diabetes UK, Embecta, Insulet, Novo Nordisk and Sanofi, and medical writing support from Abbott, Eli Lilly and Embecta, and has participated in consultancy/been an advisory board member for Abbott, Dexcom, Eli Lilly, Embecta, Insulet, Medtronic, Novo Nordisk, Roche and Sanofi. JZML declares that there are no relationships or activities that might bias, or be perceived to bias, this work.
Contribution statement
All authors were responsible for drafting the article and reviewing it critically for important intellectual content. All authors approved the version to be published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alexandros L. Liarakos and Jonathan Z. M. Lim are joint first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liarakos, A.L., Lim, J.Z.M., Leelarathna, L. et al. The use of technology in type 2 diabetes and prediabetes: a narrative review. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06203-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00125-024-06203-7


