Abstract
Aims/hypothesis
Our aim was to investigate structural changes of cutaneous Schwann cells (SCs), including nociceptive Schwann cells (nSCs) and axons, in individuals with diabetic polyneuropathy. We also aimed to investigate the relationship between these changes and peripheral neuropathic symptoms in type 1 diabetes.
Methods
Skin biopsies (3 mm) taken from carefully phenotyped participants with type 1 diabetes without polyneuropathy (T1D, n=25), type 1 diabetes with painless diabetic polyneuropathy (T1DPN, n=30) and type 1 diabetes with painful diabetic polyneuropathy (P-T1DPN, n=27), and from healthy control individuals (n=25) were immunostained with relevant antibodies to visualise SCs and nerve fibres. Stereological methods were used to quantify the expression of cutaneous SCs and nerve fibres.
Results
There was a difference in the number density of nSCs not abutting to nerve fibres between the groups (p=0.004) but not in the number density of nSCs abutting to nerve fibres, nor in solitary or total subepidermal SC soma number density. The overall dermal SC expression (measured by dermal SC area fraction and subepidermal SC process density) and peripheral nerve fibre expression (measured by intraepidermal nerve fibre density, dermal nerve fibre area fraction and subepidermal nerve fibre density) differed between the groups (all p<0.05): significant differences were seen in participants with T1DPN and P-T1DPN compared with those without diabetic polyneuropathy (healthy control and T1D groups) (all p<0.05). No difference was found between participants in the T1DPN and P-T1DPN group, nor between participants in the T1D and healthy control group (all p>0.05). Correlational analysis showed that cutaneous SC processes and nerve fibres were highly associated, and they were weakly negatively correlated with different neuropathy measures.
Conclusions/interpretation
Cutaneous SC processes and nerves, but not SC soma, are degenerated and interdependent in individuals with diabetic polyneuropathy. However, an increase in structurally damaged nSCs was seen in individuals with diabetic polyneuropathy. Furthermore, dermal SC processes and nerve fibres correlate weakly with clinical measures of neuropathy and may play a partial role in the pathophysiology of diabetic polyneuropathy in type 1 diabetes.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Diabetic polyneuropathy (DPN) is one of the most common complications of diabetes [1, 2], and is characterised by sensory dysfunction and in some cases neuropathic pain [3,4,5]. However, the mechanisms behind DPN and painful DPN are not fully understood.
Axonal degeneration and functional loss have been found both in myelinated and unmyelinated peripheral nerve fibres in DPN [6,7,8], and the decreased cutaneous free nerve endings measured by intraepidermal nerve fibre density (IENFD) is an important confirmation in DPN diagnosis [9,10,11]. However, previous studies have reported that the reduction of nociceptors and their morphological abnormalities correlate poorly with symptoms of DPN and are unlikely to be a major contributor to the development of painful neuropathy [12, 13]. There is, therefore, a need to identify other potential markers that may explain why some individuals with diabetes, but not all, develop DPN.
As one of the main glia cell types in the peripheral nervous system (PNS), Schwann cells (SCs) not only provide vital neurotrophic factors for peripheral nerves but also serve as the main resource for axonal myelination in PNS [14, 15]. The existence and structural–functional normality of SCs are important for maintaining the integrity of peripheral nerves, thus making the SC a potential important factor in axonal degeneration and possibly development of symptoms of DPN [15,16,17,18].
A recent preclinical study reported a specialised cutaneous SC type, a nociceptive SC (nSC), which contributes to pain initiation [19]. A follow-up study showed a depletion of either nociceptors or nSCs in mouse skin after hydroxytamoxifen painting, which resulted in hyperalgesia induced by thermal and mechanical stimulations, suggesting a structural–functional relationship between nSCs and neuropathic symptoms in these animals [20]. Furthermore, our previous study found an increase in nSC number density in the hind-paw glabrous skin in a mouse model of type 1 diabetes, with hypersensitive behaviours stimulated by thermal and mechanical tests [21].
Here, we investigated structural changes in SCs and their axons in DPN and their association with symptoms of neuropathy. We quantified the expression level of SCs and peripheral nerves in skin biopsies taken from healthy control individuals and from well-characterised individuals with type 1 diabetes, including those without DPN, those with painless DPN and those with painful DPN.
Methods
Study participants and clinical diagnosis of DPN and pain
The participants included in this study were part of a larger cross-sectional study of 216 participants with type 1 diabetes and healthy controls without diabetes recruited at three Steno Diabetes Centers in Denmark (in Aarhus, Odense and Copenhagen) from 2019–2021. We randomly chose 20 participants from each group (healthy control individuals, individuals with type 1 diabetes without DPN [T1D], individuals with type 1 diabetes with painless DPN [T1DPN] and individuals with type 1 diabetes with painful DPN [P-T1DPN]) and added five to eight additional individuals solely based on self-reported sex and age to each group to minimise difference between the groups. Inclusion criteria for all participants were a confirmed diagnosis of type 1 diabetes for at least 5 years and age between 30 and 75 years. Exclusion criteria for all participants were inability to understand oral instructions, neuropathy with causes other than diabetes, severe pain with causes other than neuropathy, any history of alcohol (>14 or >21 units/week for women and men, respectively) or substance abuse, pregnancy, any skin disorder or chronic ulcer in biopsy area, clinical intermittent claudication, non-palpable foot pulses and known allergy to lidocaine. Inclusion criterion for healthy control individuals was age between 30 and 75 years. Exclusion criteria for healthy control individuals were the same as for the other groups, except that no neurological or metabolic disorders were allowed, neither were clinical depression and ongoing pain of any cause. It is unknown how well the study sample represents the source population in terms of sex, ethnicity, age, regional and socioeconomic factors. However, given the inclusion criteria, we only assessed individuals aged 30–75 years and the individuals were recruited at Steno Centers across Denmark. No information on ethnicity or race was collected, as this information was not believed to have any influence on the study outcome. The study was open to individuals of all races, sex and socioeconomic status.
Anthropometric measures were collected and comprehensive evaluation was conducted on all study participants. Ankle and knee reflexes were tested, and vibration detection threshold on the hallux was measured using a biothesiometer (Horwell Neurothesiometer; Scientific Laboratory Supplies, Nottingham, UK). Values over 25 V were considered abnormal. Mechanical detection threshold was assessed using a 10 g monofilament (Neuropen; Owen Mumford, Woodstock, UK) under the hallux, and a decreased sensation was indicated if seven or fewer out of ten stimuli were detected. Pinprick sensation was tested using Neurotip (Owen Mumford) on the hallux, and temperature sensation was evaluated using thermo-rollers of 25°C (cold) and 40°C (warmth) on top of the hallux (Rolltemp II, Somedic, Sösdala, Sweden). Participants were asked to indicate whether the rollers felt cold, warm or neutral. Additionally, the participants were assessed using DPNCheck (NeuroMetrix, Woburn, MA, USA), which is a surrogate for a full nerve conduction study and measures the amplitude and velocity of the sural nerve. Amplitude < 4 µV and velocity < 40 m/s were considered abnormal. A punch skin biopsy of 3 mm was taken and a panel of blood biomarkers was analysed. The Toronto Diabetic Neuropathy Expert Group criteria were used to diagnose DPN, through evaluation of a combination of symptoms and signs [10]. Signs of DPN were assessed using the tests described above, and the diagnosis was confirmed through abnormal IENFD results from skin biopsy and DPNCheck. Participants who had a diagnosis of diabetes, reported pain in both feet/legs, had abnormal sensory signs in the feet/legs and abnormal IENFD or DPNCheck results were considered to have neuropathic pain. The severity of DPN was determined by using the Toronto clinical neuropathy score (TCNS) and the level of pain was assessed using a numeric rating scale (NRS; only participants scoring 0 [non-painful DPN] or >3 [painful DPN] on the 0–10 NRS were included in the study) and the Neuropathic Pain Symptom Inventory questionnaire (NPSI).
The study was performed in accordance with the Helsinki Declaration II and had the approval from the Regional Ethics Committee as well as the Danish Data Protection Agency (1-10-72-103-19). All participants gave their voluntary consent following a detailed explanation of the study procedures.
Skin biopsy
Punch skin biopsies (Miltex, York, PA, USA) (3 mm), were taken at the distal leg (10 cm above the lateral malleolus) under sterile conditions following intradermal injection of 1% lidocaine, in accordance with published guidelines [22, 23]. Zamboni’s fixative and 20% (wt/vol.) sucrose (in 0.1 mol/l phosphate buffer) were used for the fixation (overnight) and cryoprotection (overnight) of the specimens. After snap freezing, all specimens were stored at −20°C until further processing. The experimenters were blinded to the origin of the skin biopsies during the immunofluorescent staining and quantification of skin biopsy measures.
Immunofluorescent staining
Skin sections (50 µm thick) were cut and transferred to a neutral PBS buffer in 48-well plates. Target retrieval (in 10 mmol/l sodium citrate buffer for 20 min at 80°C) and blocking (in 1% [wt/vol.] BSA, 0.3% [vol./vol.] Triton X-100 in PBS solution for 1 h) were performed before immunolabelling.
For the primary antibodies, SCs were labelled by rabbit anti-S100 calcium-binding protein B (S100B; the antibody is ready to use with no dilution; DAKO, Denmark) and goat anti-transcription factor SOX10 antibodies (1:100 in S100B antibody solution [ready to use], R&D system, UK), and mouse anti-PGP9.5 antibody (1:1000 in S100B antibody solution [ready to use]; Bio-Rad, USA) was used to label peripheral nerves. Skin sections were incubated with the three primary antibodies in blocking buffer over two nights at 4°C, followed by a 1.5 h incubation in secondary antibody solution. The secondary antibodies were used at a concentration of 1:650 in blocking buffer: Alexa Fluor 488 donkey anti-mouse IgG (H+L) (Abcam, UK); Alexa Fluor 647 donkey anti-rabbit IgG (H+L) (Invitrogen, USA); and Alexa Fluor 594 donkey anti-goat IgG (H+L) (Invitrogen, Waltham, MA, USA) at room temperature. Lastly, DAPI (1:5000 in PBS buffer; Sigma, St Louis, MI, USA) nucleus counterstaining was applied to the skin sections before mounting.
Imaging
Z-stack images (21 µm thick, with a 1.5 µm interval between images) were acquired with a ×40 lens using a laser-scanning spectral confocal microscope (LSM 800; Zeiss, Germany). The tile function from the ZEN microscopy software (Zeiss, Germany) was used to stitch single field images into one large image that included the entire region of interest (ROI). A minimum of two Z-stack images (15 stacks with a thickness of 21 µm) including the ROI in two individual skin sections from the same participant were captured and used for all quantitative analysis.
Quantification
All quantifications were performed on orthogonally projected images of the original Z-stack confocal images. Dermal SC (DSC) area fraction and dermal nerve fibre (DNF) area fraction were determined from orthogonal average-projection images of the original Z-stack confocal images using FIJI (University of Wisconsin, WI, USA). Other quantifications were analysed on the orthogonal max-projection images of the original Z-stack confocal images using ZEN 3.3 (blue edition, Zeiss, Germany).
SC quantification
nSCs were identified as S100+/SOX10+/DAPI+ cells localised within 25 µm below the epidermal–dermal border but excluding glands and large nerve bundles as in our previous study [21]. The number density of nSCs abutting to nerve fibres (nSC+nerve complex; PGP9.5+/S100+/SOX10+/DAPI+) and the number density of nSCs not abutting to nerve fibres (nSC−nerve complex; PGP9.5−/S100+/SOX10+/DAPI+) were estimated (for details see electronic supplementary material [ESM] Methods).
The total DSC expression level was estimated by measuring the DSC area fraction, which was estimated by measuring the DSC-occupied area, divided by the total area of the ROI in the dermal area within 200 µm below the epidermal–dermal border from the orthogonally projected 2D confocal images (for details see ESM Methods).
Peripheral nerve fibre quantification
IENFD was counted following published guidelines [22, 24].
The DNF expression level was estimated by measuring the DNF area fraction, the same method as used for measuring DSC area fraction (for details see ESM Methods).
Comparison between methods for DNF and SC quantifications
To compare the results with previously published methods, we analysed the expression of subepidermal SCs (including the subepidermal SC process [SSCP]) and subepidermal SC soma [SSCS]) and subepidermal nerve fibres (SNFs) using a method optimised from a published study [25]. Here, we quantified the solitary and total SSCS number density, SSCP density and SNF density per volume within 40 µm from the border (for details see ESM Methods), and per length within 40 µm from the border (the original method [25]).
Statistical analysis
Power calculation for sample size was based on expected moderate effect sizes (Cohen’s d=0.6), 80% power and α of 0.5, resulting in approximately 20–25 individuals needed in each group to show group differences in most skin biopsy measurements. Continuous data are presented as means ± SD or medians (IQR) according to distribution. Categorical data are presented as frequency with percentage. Non-normally distributed continuous data were normalised using square root transformation, when appropriate (determined by QQ plots). Comparisons between multiple groups were performed using either one-way ANOVA (parametric test) or Kruskal–Wallis equality-of-populations rank test (non-parametric test). ANCOVA analysis was performed adjusting for sex, age and HbA1c, providing adjusted p values. Fisher’s exact test was applied when comparing categorical variables. Co-linearity was checked by observing the variance inflation factor (VIF), which was deemed to show high correlation between two explanatory variables if >5 (this was not the case). Post hoc multiple comparisons were performed on variables showing significant differences. Parametric data were analysed with pairwise comparisons t tests adjusting for age, sex and HbA1c, and results were presented as reverse-transformed means with 95% CI and p values. Dunn’s test was used for post hoc multiple comparisons tests of non-parametric data, and the results were presented as p values (not adjusted for confounders). Both of the post hoc tests were corrected for multiple testing using Bonferroni correction. Linear correlation was carried out using Pearson’s correlation analysis. Finally, partial correlational analysis was performed by adjusting for age and sex, and HbA1c. Statistical significance (α) was set at a p value ≤0.05.
Results
Participant characterisation
A total of 107 participants consisting of 25 individuals with type 1 diabetes without DPN, 30 with type 1 diabetes and painless DPN, 27 with type 1 diabetes and painful DPN and 25 healthy control individuals, were included. Main clinical characteristics are described in Table 1. There were statistically significant differences between the groups in age, total cholesterol, diastolic BP, eGFR, HbA1c, LDL-cholesterol and urinary albumin/creatinine ratio. In the confirmatory tests of DPN, differences were seen in IENFD from skin biopsies and nerve conduction velocity and amplitude using DPNCheck between the groups (all p<0.001), and sensory tests (mechanical, vibration and thermal sensation) also differed between the groups (all p<0.001). Most of the participants with DPN showed both small- and large-fibre abnormalities, indicating presence of mixed fibre neuropathy. Median (IQR) pain intensity (assessed by NRS) was 5.0 (5.0–6.0) and 5.0 (5.0–7.0) in P-T1DPN at 24 h and 7 days, respectively, before the sensory test and skin biopsy acquisition.
Visualisation and quantification of SCs
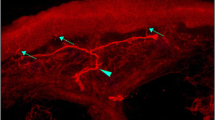
Nociceptors and nSCs were identified in the subepidermal area in human hairy skin (Fig. 1a–e and ESM Fig. 1) but they do not always form a glia–neuro complex as in mouse glabrous skin [19, 21]; for examples, see Fig. 1f–j. Conversely, most nSCs did not abut to nerve fibres (nSC–nerve complex), with the median percentage of nSCs abutting to nerve fibres (nSC+nerve complex) being <50% in all groups (Table 2). We found no difference in the number density of nSC+nerve complexes between the four groups (p<0.148, padj=0.551; Fig. 2a, Table 2). However, there was a difference in the number density of nSC–nerve complexes between the groups after adjusting for age, sex and HbA1c (p=0.078, padj=0.004; Fig. 2b, Table 2). Additionally, post hoc analysis revealed a significant increase of nSC–nerve complexes in the T1DPN and P-T1DPN groups compared with the healthy control group after adjusting for age, sex and HbA1c (both padj<0.01), but no significant difference was seen between the other two groups (all padj>0.05; Table 3).
Representative immunofluorescent visualisation of peripheral nerves and nSCs in human skin. (a–e) A representative structure of nSC+nerve complex: (a) S100 antibody-labelled overall DSCs and epidermal Langerhans cells (magenta); (b) SOX10-positive nuclei (red); (c) PGP9.5 antibody-labelled peripheral nerves (green); (d) nuclei labelled by DAPI (blue); (e) composite image. (f–j) A representative structure of nSC–nerve complex: (f) S100 antibody-labelled overall DSCs and epidermal Langerhans cells (magenta); (g) SOX10-positive nuclei (red); (h) PGP9.5 antibody-labelled peripheral nerves (green); (i) nuclei labelled by DAPI (blue); (j) composite image. (k) S100+ SCs in dermal ROI. (l) Filtered positive signals of DSCs. Scale bars, 50 μm (a–j) and 100 μm (k, l). Arrows indicate the expression of different markers of nSC or nerve fibre in the subepidermal area; yellow dotted lines indicate the epidermal–dermal border. D, dermal; E, epidermal
Quantification of DSCs in the skin. (a) Number density of nSCs abutting to nerve fibres (nSC+nerve complex). (b) Number density of nSCs not abutting to nerve fibres (nSC−nerve complex). (c) DSC area fraction in each group. (d) Solitary SSCS number density. (e) Total SSCS number density. (f) SSCP density. Post hoc analysis: parametric (square-root transformed) data are presented as adjusted p value and mean difference with 95% CI analysed by pairwise comparisons t tests, adjusting for age, sex and HbA1c (b, f); non-parametric data are presented as non-confounder adjusted p value by using Dunn’s test (c); *p<0.05 and **p<0.01
We then visualised and quantified the overall expression of DSCs localised within 200 µm below the dermal–epidermal border (Fig. 1k,l). There was a difference in DSC area fraction between the groups (p=0.003; Fig. 2c, Table 2). We found a statistically significant decline in DSC area fraction in the T1DPN group compared with the healthy control and T1D groups (both p<0.05; Table 3). Declines, albeit not statistically significant, were seen in the P-T1DPN group compared with the healthy control and T1D groups (Table 3).
Comparison between methods
To allow for a direct method comparison, we also quantified the SSCS and SSCP density using a quantification method that was modified from a recently published study [25]. There was no difference in either solitary or total SSCS number density between the groups, both before and after adjusting for age, sex and HbA1c (all p and padj>0.05; Fig. 2d,e; Table 2). However, a significant difference in SSCP density was seen between the four groups (p<0.001, padj<0.001; Fig. 2f; Table 2), and post hoc analysis showed declines of SSCP density in the T1DPN and P-T1DPN groups compared with the healthy control and T1D groups after adjusting for confounders (all padj<0.01; Table 3). We also quantified solitary and total SSCS number density and SSCP density per length using the methods published in the aforementioned study [25], and the results pointed to the same conclusion (data not shown).
Visualisation and quantification of cutaneous nerve fibres
Representative images of free nerve endings for each group are shown in Fig. 3a–d; quantification of IENFD is shown in Fig. 1g and Table 1. Post hoc analysis was not performed for IENFD as it was used in participant classification. The overall expression of DNFs was assessed by measuring DNF area fraction in the dermal area within 200 µm below the dermal–epidermal border, as illustrated in Fig. 3e,f. A difference in DNF area fraction was seen between the groups (p=0.001; Fig. 3h; Table 2). Post hoc group comparison showed no significant difference in DNF area fraction between participants with painless and painful DPN (p=1.000), but there was a decrease in the P-T1DPN group compared with the healthy control and T1D groups (both p<0.05), and a decrease in the T1DPN group compared with the control group (p=0.009; Table 3).
(a–d) Representative images of cutaneous nerve fibres (PGP9.5+) in participants in the P-T1DPN (a), T1DPN (b), T1D (c) and healthy control (d) groups. (e, f) Representative images for DNF occupancy analysis: (e) the ROI for DNF occupancy analysis; (f) the filtered positive signals of peripheral nerves within the ROI. (g) IENFD in each group (post hoc analysis was not performed for IENFD because IENFD was used in participant classification). (h) DNF area fraction in each group. (i) SNF density in each group. Scale bar, 100 μm (a–f). The yellow dotted line in (a–d) marks the border of the epidermis; in (e, f) the line marks the ROI for analysing the DNF occupancy. Post hoc analysis: parametric (square-root transformed) data are presented as adjusted p value and mean difference with 95% CI analysed by pairwise comparisons t tests, adjusting for age, sex and HbA1c (h); non-parametric data are presented as non-confounder adjusted p value by using Dunn’s test (i); *p<0.05 and **p<0.01. D, dermal; E, epidermal
Comparison between methods
A significant difference in SNF density per volume (a method modified from a published study [25]) was seen between the groups (p<0.001, padj<0.001; Fig. 3i; Table 2). Post hoc analysis showed reduced SNF density per volume in the T1DPN and P-T1DPN groups compared with the healthy control and T1D groups (all padj<0.05), while there was no difference between the T1DPN and P-T1DPN groups (padj=1.000, Table 3). Lastly, quantifying SNF density per length using the previously published method was also performed [25] and the results pointed towards the same conclusion (data not shown).
Association between cutaneous SCs and nerve fibres
To investigate the association between cutaneous SCs and nerve fibres, we performed correlational analysis between the skin biopsy quantifications (Table 4).
SC measures, including the number density of nSC+nerve complexes, SSCP density, solitary and total SSCS density, correlated positively with each other, but the number density of nSC−nerve complexes did not correlate with DSC area fraction or SSCP density.
IENFD correlated positively with DNF area fraction, SNF density, DSC area fraction, number density of nSC+nerve complexes, SSCP density and total (but not solitary) SSCS number density, and correlated negatively with the number density of nSC−nerve complexes.
Association between skin biopsy results and markers of neuropathy
Correlation analysis is shown in Table 5. The number density of nSC+nerve complexes had a weak negative correlation with the Michigan Neuropathy Screening Instrument (MNSI) total score and biothesiometer but no correlation was found after adjusting for confounders. The number density of nSC−nerve complexes had a weak and positive correlation with TCNS score after, but not before, adjusting for confounders. Total SSCS density had a weak negative correlation with MNSI total score and TCNS score but no correlation was observed after adjusting for confounders.
Moreover, DSC area fraction, SSCP density and SNF density were weakly and negatively correlated with the MNSI questionnaire (MSNI-Q), MNSI total score, TCNS and vibration test (biothesiometer), although the correlation between DSC area fraction and MNSI-Q lost significance after adjusting for confounders. Finally, DNF area fraction correlated negatively with MNSI-Q, MNSI total score and TCNS score but not with vibration test.
Discussion
This study investigated structural changes in specialised nSCs, as well as the overall cutaneous SCs and axons in individuals with type 1 diabetes and assessed their association with DPN and its symptoms. Together with the three group comparison results (ESM Results and Tables 1, 2), we found the following: (1) there was no difference in the number density of nSC+nerve complexes between the groups but there was an increase in the number density of nSC−nerve complexes in individuals with DPN (regardless of pain status) vs healthy control individuals and those without DPN; (2) there was a degeneration of overall DSCs (DSC area fraction) and SSCP density (but not solitary or total SSCS number density), and a degeneration of both epidermal and dermal cutaneous nerve fibres (IENFD, DNF area fraction and SNF density), in individuals with DPN compared with healthy control individuals and those without DPN; (3) there was no difference in any of the skin biopsy measurements between individuals with DPN with and without pain, nor between individuals without DPN and healthy control individuals, indicating that the markers do not play a significant role in diabetes or painful DPN, but possibly do in DPN; and (4) the expression of overall SCs, SC processes and cutaneous nerves correlated weakly and negatively with clinical examinations, including MNSI-Q, MNSI total score, TCNS score and biothesiometer. Taken together, the findings suggest that the expression of cutaneous SCs (particularly processes) and nerves are both reduced and interdependent in this cohort of individuals with DPN and correlate weakly with neuropathy severity but not neuropathic pain.
These findings are of interest for several reasons. First, just as in previous mouse studies, we found that nociceptors and nSC processes are interdependent in diabetes, meaning that if one cell type degenerates or is damaged, the other one will degenerate as well [20, 21]. Second, individuals with DPN display an increase of nSC−nerve complexes compared with healthy control individuals, while at the same time they have degenerated cutaneous nerve fibres and SSCPs. It is unclear whether these specialised nSCs exhibit greater plasticity than other types following damage. Third, we showed that there were no significant differences in any of the skin biopsy measurements between individuals with DPN with and without pain but the degenerated cutaneous SCs and nerves were associated with DPN. Importantly, the overall SCs, SSCPs and cutaneous nerves correlated negatively, albeit weakly, with MNSI-Q, MNSI total score, TCNS and biothesiometer. These results indicate that, like cutaneous nerves, SC processes, but not SC somata and specialised nSCs, are to some degree associated with neuropathy measures in this cohort of individuals with type 1 diabetes. Fourth, the findings highlight that the common classification of SCs into myelin and non-myelin SCs (also known as Remak SCs) may be oversimplified and that it is important to differentiate between different subtypes of SCs and their function.
There is currently no consensus on how to define and quantify nSCs and DSCs, making comparisons between studies difficult. We, therefore, supplemented our method of quantification with a replication of the methods used in the other study quantifying subepidermal SC and axons [25]. Our methods for quantifying overall DSCs and nerves yielded slightly different results compared with the optimised method described in the previous study for quantifying subepidermal SCs and nerves. More profound degeneration was found in SC processes and in nerves in the subepidermal area (40 μm below the epidermal–dermal border) compared with the SCs and nerves in the overall dermal area (200 μm below epidermal–dermal border). However, quantification of subepidermal SCs and nerves using both the original and modified methods described in the published study and this present study pointed to the same conclusions, suggesting that both methods are reliable.
In our preclinical study in mice, nSCs were defined as being S100+ and SOX10+ and co-localised with peripheral nerve fibres to form a mesh-like network at the subepidermal area (within 25 µm below the epidermal–dermal border), with glia–neuro projections entering the epidermis [21]. Here we observed similar structures in the human skin but most of the nSCs were not co-localised with peripheral nerve fibres. The structural differences in nSCs when comparing mice and humans might be due to the difference in skin biopsy locations (glabrous skin biopsies in mice and hairy skin biopsies in humans). The lack of specific biomarkers for the specialised nSCs is a considerable challenge for understanding those glial–neuronal complexes. Additionally, caution should be used when translating the nSC quantification criteria from preclinical studies in glabrous skin to clinical studies in hairy skin.
The discussion of SC classification and nSC definition prompts a reconsideration of how heterogeneous cutaneous SCs interact with cutaneous nerves and respond to nerve damage, as well as their involvement in neuropathic pain. This knowledge will aid in identifying more specific treatment targets for peripheral nerve diseases [26]. A further question arising from this study is whether the reprogramming capacity of cutaneous SCs remains the same, and how the associated biomarkers (e.g. SOX10) are involved in nSCs following nerve damage caused by hyperglycaemia.
The study has several limitations. The participants with DPN included in this study had relatively mild symptoms; most had median pain intensity with only few having severe pain. This may have resulted in less pronounced differences between the groups in some of the measures, including the nSCs, and thereby possibly the study was underpowered. Additionally, we were unable to completely match the groups of participants according to sex and age. However, the influence of these confounding factors on the results was minimised through adjusting for these confounders. Lastly, the cross-sectional design of the study did not allow us to investigate whether it is the nociceptors or the SCs that are damaged first in type 1 diabetes. Despite these limitations, the study has strengths, including careful phenotyping of individuals according to recommended guidelines as well as a detailed assessment of nerve fibres and SCs and their morphology using different methods.
Conclusion
Cutaneous SCs and nerve fibres are partially interdependent in this cohort of individuals with type 1 diabetes with and without diabetic polyneuropathy. We found a degeneration of nerve fibres in the epidermis and dermis and of SC processes in individuals with DPN compared with healthy control individuals and those without DPN, but found no differences when comparing those with and without pain. Additionally, a correlational analysis between dermal fibres and DSC processes with clinical measures of neuropathy indicate that they are weakly associated with neuropathy measures, thus potentially playing a role in the pathophysiology of diabetic polyneuropathy in type 1 diabetes.
Abbreviations
- DNF:
-
Dermal nerve fibre
- DPN:
-
Diabetic polyneuropathy
- DSC:
-
Dermal SC
- IENFD:
-
Intraepidermal nerve fibre density
- MNSI:
-
Michigan Neuropathy Screening Instrument
- MNSI-Q:
-
MNSI questionnaire
- NRS:
-
Numeric rating scale
- nSC:
-
Nociceptive SC
- nSC+nerve complex:
-
Nociceptive SC abutting to nerve fibres
- nSC−nerve complex:
-
Nociceptive SC not abutting to nerve fibres
- PNS:
-
Peripheral nervous system
- P-T1DPN:
-
Type 1 diabetes with painful diabetic polyneuropathy (group)
- ROI:
-
Region of interest
- S100B:
-
S100 calcium-binding protein B
- SC:
-
Schwann cell
- SNF:
-
Subepidermal nerve fibre
- SSCP:
-
Subepidermal SC process
- SSCS:
-
Subepidermal SC soma
- TCNS:
-
Toronto clinical neuropathy score
- T1D:
-
Type 1 diabetes without diabetic polyneuropathy (group)
- T1DPN:
-
Type 1 diabetes with painless diabetic polyneuropathy (group)
References
Zochodne DW (2019) The challenges of diabetic polyneuropathy: a brief update. Curr Opin Neurol 32(5):666–675. https://doi.org/10.1097/wco.0000000000000723
Iqbal Z, Azmi S, Yadav R et al (2018) Diabetic peripheral neuropathy: epidemiology, diagnosis, and pharmacotherapy. Clin Ther 40(6):828–849. https://doi.org/10.1016/j.clinthera.2018.04.001
Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL (2012) Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol 11(6):521–534. https://doi.org/10.1016/s1474-4422(12)70065-0
Zochodne DW (2014) Clinical features of diabetic polyneuropathy. Handb Clin Neurol 126:23–30. https://doi.org/10.1016/b978-0-444-53480-4.00002-3
Gylfadottir SS, Christensen DH, Nicolaisen SK et al (2020) Diabetic polyneuropathy and pain, prevalence, and patient characteristics: a cross-sectional questionnaire study of 5,514 patients with recently diagnosed type 2 diabetes. Pain 161(3):574–583. https://doi.org/10.1097/j.pain.0000000000001744
Frank T, Nawroth P, Kuner R (2019) Structure-function relationships in peripheral nerve contributions to diabetic peripheral neuropathy. Pain 160(Suppl 1):S29–S36. https://doi.org/10.1097/j.pain.0000000000001530
Sorensen L, Molyneaux L, Yue DK (2006) The relationship among pain, sensory loss, and small nerve fibers in diabetes. Diabetes Care 29(4):883–887. https://doi.org/10.2337/diacare.29.04.06.dc05-2180
Britland ST, Young RJ, Sharma AK, Clarke BF (1990) Association of painful and painless diabetic polyneuropathy with different patterns of nerve fiber degeneration and regeneration. Diabetes 39(8):898–908. https://doi.org/10.2337/diab.39.8.898
Umapathi T, Tan WL, Loke SC, Soon PC, Tavintharan S, Chan YH (2007) Intraepidermal nerve fiber density as a marker of early diabetic neuropathy. Muscle Nerve 35(5):591–598. https://doi.org/10.1002/mus.20732
Tesfaye S, Boulton AJ, Dyck PJ et al (2010) Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 33(10):2285–2293. https://doi.org/10.2337/dc10-1303
Joint Task Force of the EFNS and the PNS (2010) European Federation of Neurological Societies/Peripheral Nerve Society Guideline on the use of skin biopsy in the diagnosis of small fiber neuropathy. Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society. J Peripher Nerv Syst: JPNS 15(2):79–92. https://doi.org/10.1111/j.1529-8027.2010.00269.x
Karlsson P, Hincker AM, Jensen TS, Freeman R, Haroutounian S (2019) Structural, functional, and symptom relations in painful distal symmetric polyneuropathies: a systematic review. Pain 160(2):286–297. https://doi.org/10.1097/j.pain.0000000000001381
Karlsson P, Gylfadottir SS, Kristensen AG et al (2021) Axonal swellings are related to type 2 diabetes, but not to distal diabetic sensorimotor polyneuropathy. Diabetologia 64(4):923–931. https://doi.org/10.1007/s00125-020-05352-9
Kidd GJ, Ohno N, Trapp BD (2013) Biology of Schwann cells. Handb Clin Neurol 115:55–79. https://doi.org/10.1016/b978-0-444-52902-2.00005-9
Wilson ER, Della-Flora Nunes G (2021) Schwann cell interactions during the development of the peripheral nervous system. Dev Neurobiol 81(5):464–489. https://doi.org/10.1002/dneu.22744
Liu YP, Shao SJ, Guo HD (2020) Schwann cells apoptosis is induced by high glucose in diabetic peripheral neuropathy. Life Sci 248:117459. https://doi.org/10.1016/j.lfs.2020.117459
Naruse K (2019) Schwann cells as crucial players in diabetic neuropathy. Adv Exp Med Biol 1190:345–356. https://doi.org/10.1007/978-981-32-9636-7_22
Mizisin AP (2014) Mechanisms of diabetic neuropathy: Schwann cells. Handb Clin Neurol 126:401–428. https://doi.org/10.1016/b978-0-444-53480-4.00029-1
Abdo H, Calvo-Enrique L (2019) Specialized cutaneous Schwann cells initiate pain sensation. Science 365(6454):695–699. https://doi.org/10.1126/science.aax6452
Rinwa P, Calvo-Enrique L, Zhang MD, Nyengaard JR, Karlsson P, Ernfors P (2021) Demise of nociceptive Schwann cells causes nerve retraction and pain hyperalgesia. Pain 162(6):1816–1827. https://doi.org/10.1097/j.pain.0000000000002169
Hu X, Agarwal N, Zhang MD et al (2022) Identification and quantification of nociceptive Schwann cells in mice with and without Streptozotocin-induced diabetes. J Chem Neuroanat 123:102118. https://doi.org/10.1016/j.jchemneu.2022.102118
Lauria G, Bakkers M, Schmitz C et al (2010) Intraepidermal nerve fiber density at the distal leg: a worldwide normative reference study. J Peripher Nerv Syst: JPNS 15(3):202–207. https://doi.org/10.1111/j.1529-8027.2010.00271.x
Karlsson P, Nyengaard JR, Polydefkis M, Jensen TS (2015) Structural and functional assessment of skin nerve fibres in small-fibre pathology. Eur J Pain (London, England) 19(8):1059–1070. https://doi.org/10.1002/ejp.645
Karlsson P (2022) Chapter 5: skin biopsy analysis in diabetic neuropathy. In: Tavakoli M (ed) Diabetic neuropathy. Elsevier, Amsterdam/Oxford/Cambridge. https://doi.org/10.1016/B978-0-12-820669-0.00013-X
Özdağ Acarlı AN, Klein T, Egenolf N, Sommer C (2022) Subepidermal Schwann cell counts correlate with skin innervation - an exploratory study. Muscle Nerve 65(4):471–479. https://doi.org/10.1002/mus.27496
Negro S, Pirazzini M, Rigoni M (2022) Models and methods to study Schwann cells. J Anat 241(5):1235–1258. https://doi.org/10.1111/joa.13606
Funding
Open access funding provided by Royal Danish Library, Aarhus University Library
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data availability
Due to restrictions related to Danish law protecting patient privacy, the data used in this study can only be made available through an application to Aarhus University by contacting the corresponding author or Aarhus University (clin@au.dk).
Funding
Open access funding provided by Royal Danish Library, Aarhus University Library. This research was funded by the Novo Nordisk Foundation (grant no. NNF18OC0052301) and by the Lundbeck Foundation (grant no. R359-2020-2620). XH is funded by a PhD stipend from the Danish Diabetes Academy, which is funded by the Novo Nordisk Foundation (grant no. NNF17SA0031406).
Authors’ relationships and activities
PK has received personal fees from Grünenthal, Alnylam and Vertex Pharmaceuticals and has received a research grant from Merck outside the submitted work. The other authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
All authors meet the ICMJE uniform requirements for authorship and approved the final version of the manuscript. PK, TSJ, CSB, CSH, KBY, JRN, PE, MDZ and XH conceptualised the study and contributed to study design. XH and PK participated in skin biopsy data acquisition. XH, PK, CSB and MBS participated in data analysis. CSB, CSH, PK, KBY, KS, HIM and HK contributed to clinical data acquisition. All authors contributed to manuscript drafting, editing and revision for intellectual content. PK and XH are responsible for the integrity of the work as a whole.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, X., Buhl, C.S., Sjogaard, M.B. et al. Structural changes in Schwann cells and nerve fibres in type 1 diabetes: relationship with diabetic polyneuropathy. Diabetologia 66, 2332–2345 (2023). https://doi.org/10.1007/s00125-023-06009-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-023-06009-z